Differentiating Depression and Bipolar Depression
advertisement

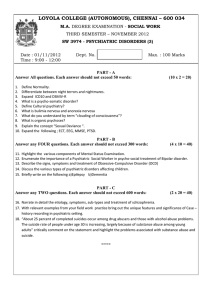
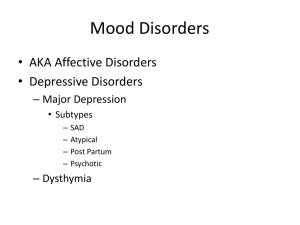
Differentiating Depression and Bipolar Depression M. Joyce Sasse DNP APRN PMHNP-BC PMHCNS-BC About BHECN The Behavioral Health Education Center of Nebraska (BHECN, pronounced “beacon”) was created by the Legislature to address the shortage of behavioral health professionals in rural and underserved areas. BHECN recruits & educates students in behavioral health and trains & retains professionals in the workforce. By increasing the number of behavioral health professionals, improving accessibility of behavioral health care, and building competence of the workforce, we are improving the health of all Nebraskans. Learn more at unmc.edu/bhecn Keep up with the latest events and trainings from BHECN: facebook.com/BHECN About the Mental & Behavioral Health Care Webinar Series Individual webinars will focus on common psychiatric disorders using a holistic approach to include cultural awareness, spirituality, interdisciplinary collaboration, psychopharmacology, and principles of recovery. Acknowledgements BHECN would like to acknowledge the collaboration with the American Psychiatric Nurses Association, NE Chapter (APNA-NE) in the development and implementation of this educational series. Learn more at: www.apna.org Differentiating Depression and Bipolar Depression M. Joyce Sasse DNP APRN PMHNP-BC PMHCNS-BC Conflict of Interest Disclosure Dr. Sasse is the president and sole owner of Joyce K Sasse NP, PC, which manages her private psychiatric practice, consulting, and educational nursing activities. Dr. Sasse has no other financial interests or conflicts with other organizations or entities that will detract from the balance, independence, objectivity, or scientific rigor of this program. Off-Label Use of Medications Dr. Sasse will mention off-label uses for medications in her lecture Handouts for this program can be downloaded under the “Handouts” tab in your GoToWebinar gray control box Handouts clearly label any off-label use of medications, recourses, and other information for the participants. Poll Question Is the following statement true or false? People who commit suicide are mentally ill. Depression in General In the U.S., 6-12% of the population will suffer from depression sometime during its life. Suicide is the eighth-leading of cause of death in the U.S. Almost all people who complete a suicide have a diagnosable mental disorder with or without substance abuse, and substance abuse is often a form of self- medicating depression. (Andrew 2014) Suicide In 2005, suicides accounted for 1.4% of all deaths worldwide. This statistic is low because many suicides go unreported for many reasons. Sadly, over 60% of people who commit and complete suicide have seen a doctor within 30 days of the event. (Andrew 2014) Depression People with depression are more likely to suffer from: • Type 2 diabetes and cardiovascular disease • Unipolar depression. (Unipolar depression is projected to be the second-leading cause of disability worldwide.) (Andrew, 2014) Unipolar Depression 66% of people with depression don’t know they have a treatable illness and don’t look for treatment. 50% of persons diagnosed with major depression receive any kind of treatment. 20% of those individuals receive treatment that meets current practice guidelines. (Gonzales, Vega, Williams et al. 2010) Bipolar Depression Lifelong prevalence of Bipolar Disorder in the U. S. is between 3.7% and 3.9%. • • • • Bipolar Disorder Type I (BPI) (1.0%) Bipolar Disorder Type II (BPII) (1.1%) Sub-threshold Bipolar Disorders (2.4-4.7%) International prevalence (5-7%) (Soreff, 2015) Bipolar Depression 15% of all persons suffering from Bipolar disorders will commit suicide 36.3% risk of suicide–25% of all completed suicides (American Psychiatric Association, 2013) Poll Question Is the following statement true or false? Science is close to isolating the two genes that control depressive and manic behaviors. Isn’t All Depression the Same? “Modern genomics suggests that the spectrum is not a single disease, but a complex of hundreds if not thousands of different diseases, with overlapping genetic, epigenetic, and biomarkers as well as clinical symptoms and functional outcomes.” (Stahl 2013) Brain SPECT Scans Chromosome 12 Chromosome 10 Two genetic variants on Chromosome 10 found in women with recurrent Major Depressive Disorder: one near SIRT1 & one at LHPP In a further analysis of women with severe MDD, a stronger genetic signal appeared at SIRT1 (Cai, Chang, Li, & Li, et al. 2015) Depression Odds 50% Unipolar Depression 2% Bipolar I Disorder 15% Bipolar II Disorder 33% Bipolar Spectrum Disorder (Stahl 2013) How to Tell Them Apart Depression is the common subset of symptoms between Unipolar and Bipolar Spectrum Disorders. Symptomatic persons of both disorders spend most of their time in the depressed state. Depression is the symptom that most often brings the person in for treatment. (LeBano 2015) Information Sources Family History/Genetics Close Family Members Age of Onset of Symptoms Response to Psychiatric Medications Symptom Observation and Questions Tests: Young Mania Rating Scale, Hamilton Depression Scale, et al (Hegerl, Bottner, Holtschmodt-Taschner, et al, 2008, Stahl 2013,Vieta, SanchezMoreno, Lahuerta, et al 2008, Zimmerman, Ruggero, Chelminski & Young 2008) Social History Social History (Environmental Influences, Moves and Reasons, Housing Conditions) Military Hx Family Dynamics/Demographic and Historical Information Parents Siblings Married Children Significant Other Friends Losses in Last 12 Months Spiritual Preference Social History Environmental Influences, Moves and Reasons, Housing Conditions • What in your background from childhood, school or your past brings you here today • Or can help me understand you better, • Or help me understand the problems you bring today better Birth/Adoptive Family Family Dynamics/Demographic and Historical Information • Parents: – Names, where they live, and if the patient has emotional attachment to them • Siblings: – How many, birth order, and if the patient has emotional attachment to them Nuclear Family Married: Spouse, marital status, number of children from this marriage , and if any, their whereabouts Children: First name and ages Significant Other: Name and how long together Outside Attachments Friends: Do you have any friends that you consider your emotional support group? Losses in Last 12 Months Spiritual Preference Mental Health History Family Hx Hospitalizations Past Tx: Medication Therapy Current Symptoms Current Tx Psychiatrist Therapist Family Psychiatric History In your blood-related family, have there been any members who: • Had psychiatric diagnoses from medical providers? • Received treatment with psychiatric medications? • Been hospitalized for psychiatric reasons? • Had possible undiagnosed mental health problems? Psychiatric Hospitalizations Have you ever been hospitalized overnight for psychiatric reasons? • What was your diagnosis or the reason for the admission? • Did you receive any medication or special treatments? • Do you know the name of the doctor who treated you at the hospital? Past Treatment: Medication What psychiatric medications have you been on in the past? • How did each of these work for you? • What are you current psychiatric medications? • How are your current psychiatric medications working for you? Past Treatment: Therapy Have you seen a Therapist or a Counselor? • Where and when? • Why did you see the therapist or a counselor? • Are you currently in therapy or counseling? • If so, for what reason(s)? Current Psychiatric Symptoms Begin with Historical Questions • When was the first time you ever remember being depressed? • What caused it? • How long did that episode last? • How many other depressive episodes have you had? Current Psychiatric Symptoms During those depressed episodes, did you ever have an abrupt change of mood where you were giddy/happy or hyper-irritable? • Did the mood change period go on for two days, one week, or longer? • During that period, did you have an inflated self-esteem or grandiosity? • Did you have a decreased need for sleep without loss of energy? Current Psychiatric Symptoms During those depressed episodes, did you ever have an abrupt change of mood where you were giddy/happy or hyper-irritable? • Did you have an increase in goal-directed activity? • Were you more talkative than usual, talking faster than usual, or did you talk to more people than usual? • Did you have ideas race through your head that went so fast, you could not keep up with them? Current Psychiatric Symptoms During those depressed episodes, did you ever have an abrupt change of mood where you were giddy/happy or hyper-irritable? • Were you more distractible than usual? • Did you feel more distractible than usual, use more alcohol or drugs, or did you feel more agitated than usual? • Did you have a high involvement in risky behaviors or do things that were fun but could have resulted in painful consequences? Current Psychiatric Symptoms In the past two weeks, have you: • Been depressed most of the day, most every day? • Had a markedly diminished joy or interest in all or almost all activities, or can you still find joy in life? • Been able to perform all of your daily activities without a struggle? Current Psychiatric Symptoms In the past two weeks, have you: • Had a change in appetite or change in weight that you did not plan? • Had any trouble with sleeping: falling asleep, waking during the night, or waking up early? • Have you awakened refreshed? Current Psychiatric Symptoms In the past two weeks, have you: • Felt fatigued or had a loss of energy nearly every day? • Felt agitated nearly every day? • Had feelings of worthlessness or excessive guilt? Current Psychiatric Symptoms In the past two weeks, have you: • Had trouble with thinking, concentration, memory, or the ability to make decisions? • Had recurrent thoughts about death, suicidal ideations, or a plan to commit suicide? Have you ever attempted suicide? Current Psychiatric Symptoms In the past two weeks, have you: • Had any homicidal thoughts or plans? • Had panic attacks, anxiety attacks, or constant feelings of anxiety? If so: -What are the symptoms? -What triggers them? -What helps them to get better? Current Psychiatric Symptoms Continue asking questions to cover: • Obsessive-Compulsive Disorder • Eating Disorder • Hallucinations • Derealization • Self-Harm -Do you feel the need to cut, burn, or self-harm in any way to reduce internal pain or distress? Poll Question Is the following statement true or false? Alcoholism is a disease that is regulated by one’s genetic makeup. Substance Abuse History Family CD Hx: Client Use: alcohol, street drugs or abuse of prescription drugs • Drug of Choice • First Use • Last Use Substance Abuse History Client Use: • Do you feel you have a problem with drugs or alcohol? • Treatment History • Collateral Information Further Information Have the patient take some of the objective tests Ask the patient for permission to speak to family members for further information Medication Treatment Antidepressants Lithium Antipsychotics Anticonvulsants Others Antidepressants SSRIs SNRIs SSNRIs Other TCAs-Tri & Tetracyclics MAOIs Lithium Effective for mania and prevention of mania Somewhat effective with depression Stabilizes mood Helps prevent suicide in bipolar disorder Augmenting agent for unipolar depression (off-label) Antipsychotics Atypicals • Aripiprazole • Quetiapine • Lurasidone • Respiradone • Paliperidone • Olanzapine and Olanzapine + Fluoxetine • Ziprazidone • Asenapine Anticonvulsants Valproate Carbamazepine Lamotrigine Oxcarbazepine Topiramate Zonisamide Gabapentin & Pregabalin Levetiracetam Others Ketamine Nimodipine-Calcium Channel Blockers Benzodiazepines Folate (Bipolar Network News, 2015, Stahl, 2013) Case: 30 year old male; c/o stress and depression Mood: Depressed and his affect is irritable. Psychosocial: States he is unmarried, h/o 1 divorce; 2 failed long term relationships; no children; lives alone in a rented apartment Has always lived in this city. Father divorced his mother when he was 10. Had trouble paying attention in school; has difficulty with remembering things. Graduated from high school. Was better at sports than with academic work. Did not do well in college and dropped out after his first semester. Is a plumber's assistant in a family owned business. Psych Hx: Has never been on any psychiatric medications. Was evaluated when he was younger and it was suggested that he take medication for Attention Deficit Disorder. His father refused to let him take the medication so he did not receive or take them. Family History: Positive for a mother with bipolar disorder, a maternal aunt with bipolar disorder, his father suffered from what his mother thought was attention deficit hyperactivity disorder and his older brother has depression and moodiness. Was first depressed when he was 8 years old and he saw his parents fighting. His depression has been off and on through his whole life with varying severity. Wonders if there is any reason for him to be alive but denies any suicide attempts. Has times when he will become very irritable and angry-these episodes will last for 3-4 days. During these time he will not be like himself, When those days are over he is more depressed than ever. Poll Question What else do you want to find out to help you make a differential diagnosis(es) for James ? References American Psychiatric Association. (2013).Bipolar and related disorders. In American Psychiatric Association, Diagnostic and statistical manual of mental disorders fifth edition (pp 123-154). Arlington, VA: American Psychiatric Publishing. American Psychiatric Association. (2013).Depressive Disorders. In American Psychiatric Association, Diagnostic and statistical manual of mental disorders fifth edition (pp 155-188). Arlington, VA: American Psychiatric Publishing. Andrew, L.B. (2014). Depression and suicide. Medscape. Retrieved from http://emedicine.medscape.com/article/805459-overview#a2 Aziz, R., Lorberg, B., & Tampi. (2006, December). Treatments for late-life bipolar disorder. American Journal of Geriatric Pharmacotherapy, 4(4) pp347-364 Andrew, L.B. (2014). Depression and suicide. Medscape. Retrieved from http://emedicine.medscape.com/article/805459-overview#a2 Bipolar Network News.(2012, October) A genetic Risk factor for bipolar disorder: The CACNA1C gene. Bipolar Network News. Retrieved from http://bipolarnews.org/index.php?s=Nimodipine Bipolar Network News.(2012, October) A genetic Risk factor for bipolar disorder: The CACNA1C gene. Bipolar Network News. Retrieved from http://bipolarnews.org/index.php?s=Nimodipine Bipolar Network News.(2015, April) Gene CACNA1C is associated with early-onset bipolar disorder. Bipolar Network News. Retrieved from http://bipolarnews.org/index.php?s=Nimodipine Cai, N., Chang, S, Li, Y., Li, Q., Hu, J., Liang, J., Song, L., Kretzschmar, W., Gan, X., Nicod, J., Rivera, M., Deng, H., Du, B., Li, K., Sang, W., Gao, J., Gao, S., Ha., Ho H.Y., Hu, C., Hu, Z., Huang, G., Jiang, G., Jiang, T., Jin, W., Li. G., Li, K., Li, Y., Li, Y., Li, Y., Lin, YT., Liu, L., Liu, T., Liu, Y., Liu, Y., Lu, Y., Lv. L., Meng, H., Qian, P., Sang, H., Shen, J., Shi, J., Sun, J., Tao, M., Wang, G., Wang, G., Wang, J., Wang, L., Wang, X., Wang, X., Yang, H., Yang L., Yin, Y., Zhang, J., Zhang, K., Sun, N., Zhang, W., Zhang, X., Zhang, Z., Zhong, H., Breen, G., Wang, J., Marchini, J., Cgen, Y., Xu, Q., Xu, X., Mott, R., Huang, G., Kendler, K., & Flint, J. (2015, May) Molecular signatures of major depression. Current Biology, 25(9) pp1146-1156 Citrome, L (2014, December) Treatment of bipolar depression: Making sensible decisions. CNS Spectrum, 19, pp4-12 Gonzalez, H.M., Vega, W.A., Williams, DR., Tarraf W., West, B.T., & Neighbors, H.W. (2010, January). Depression care in the United Stated: Too little for too few. Archives of General Psychiatry, 67(1) pp37-46 Hallowell, L.(Sen. Ed.). (2016) Nursing 2106 drug handbook. Philadelphia, PA: Wolters Kluwer Hegerl,U., Bottner, A.C., Holtschmidt-Taschner, B., Born, C., Seemuller, F., Scheunemann, W., Schutze, M., Grunze, H., Henkel, V., Mergl, R., & Angst, J. (2008, July). Onset of depressive episodes is faster in patients with bipolar versus unipolar depressive disorder: evidence from a retrospective comparative study. Journal of Clinical Psychiatry, 69(7), pp1075-1080 Le Bano, L. (2015, July). How to differentiate bipolar disorder from unipolar depression. Psych Congress Network. Retrieved from http://www.psychcongress.com/article/how-differentiate-bipolardisorder-unipolar-depression-12483. O’Donovan, C., Garnham, J., Hajeck, T., & Alda. (2008, April). Antidepressant monotherapy in prebipolar depression; Predictive value and inherent risk. Journal of Affective Disorders, 107(1-3) pp293-298 Papolos, D., Mattis, S., Golshan, S., & Molay, F.(@009, November). Fear of harm, a possible phenotype of pediatric bipolar disorder: A dimensional approach to diagnosis for genotyping a psychiatric syndromes. Journal of Affective Disorders, 118(1-3) pp28-38 Rosa, A., Andreazza, A., Kunz, M., Gomes, F., Santin, A., Sanchez-Moreno, J., Colom, F., Vieta, E., & Kapczinski, F. (2008, April). Predominant polarity in bipolar disorder: Diagnostic implications. Journal of Affective Disorders, 107(1-3) PP45-51 Smith, D., Griffiths, E., Kelly, M., Hood, K., Craddock, N., & Simpson, S. (2001, July). Unrecognized bipolar disorder in primary care patients with depression. British Journal of Psychiatry, 199(1) pp 49-56 Soreff, S., (2015). Bipolar affective disorder. Medscape. Retrieved from http://emedicine.medscape.com/article/286342-overview#a5 Stahl, S.M. (2013). Mood Disorders. In S. M. Stahl, Stahl’s essential psychopharmacology, Neuroscientific basis and practical application (pp 237-283). New York, NY: Cambridge University Press. Stensland, M., Schultz, J. & Frytak, J. (2008, May), Diagnosis of unipolar depression following initial identification of bipolar disorder: A common and costly misdiagnosis. Journal of Clinical Psychiatry, 69(5), pp749-758 Vieta,E., Sanchez-Moreno, J., Lahuerta, J., Zaragoza, S., (2008, April) Subsyndromal depressive symptoms in patients with bipolar and unipolar disorder during clinical remission. Journal of Affective Disorders, 107(1-3) 169-174. Zimmerman, M., Ruggero, C.J., Chelminski, I., & Young, D. (2008, June). Is bipolar overdiagnosed?. Journal of Clinical Psychiatry, 69(6) 935-940. Images CACNA1C Gene- Bipolar Network News October 30, 2012 SPECT scans of the brain-Brain Matters Imaging Centers 2007