Hemodiafiltration: principles and advantages over conventional HD
advertisement

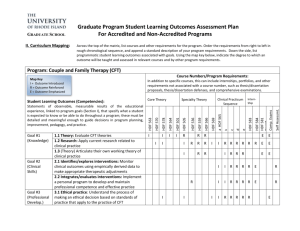
Hemodiafiltration: principles and advantages over conventional HD Rukshana Shroff Great Ormond Street Hospital for Children London, UK Effectiveness of RRT modalities Mcfarlane, Seminars in dialysis, 2009 No benefit from increased urea clearance HEMO study, NEJM, 2002 HDF – clearance by diffusion and convection Outline Mechanisms of hemodiafiltration (HDF) - theoretical advantages Clinical benefits of HDF vs conventional HD - lessons from adult studies - focus on growth and nutrition - in-centre nocturnal HDF Survey across EU Research study – effects of HDF vs HD on growth & cardiovascular outcomes in children Advantages of HDF 1. Clearance of uraemic solutes across a wide molecular weight range 2. Biocompatibility 3. Hemodynamic stability 1. Clearance on HDF vs HD β2microglobulin clearance HDF achieves 70 – 78% reduction in β2 microglobulin (vs 40 – 50% with high-flux HD) Thomas et al, Semin Dialy, 2009 No signs of amyloidosis after 8 yrs on HDF (vs 100% pts on HD have amyloid by 13 yrs) Canaud et al, NDT, 1998 82% reduced incidence of carpal tunnel syndrome and 67% reduced incidence of erosive arthritis Dember et al, Semin Dialy, 2006 For every 10 mg /l increase in predialysis ß2M there is a 11% increase risk of death (HEMO Study) Cheung et al, JASN 2000 β2-microglobulin levels (mg/L) β2-microglobulin in our HD vs HDF patients p = 0.02 • Significant association with convective volume (>15L/m2 β2-microglobulin < 25mg/L) Number ofwith children • No further reduction increasing time on HDF Pre-dialysis phosphate levels (mg/L) Phosphate levels in our HD vs HDF patients • No difference between HDF vs HD (p = 0.07) • 9/15 on HD vs 13/15 on HDF achieved KDOQI Number of children recommended levels FGF-23 levels in our HD vs HDF patients FGF-23 levels (RU/mL) p = 0.003 • 29% lower FGF-23 levels on HDF vs HD Number of children • Significant association with convective volume Other middle molecules cleared by HDF Parathyroid hormone Inflammatory cytokines (IL-6, IL-8, IL-12) Homocysteine Guanidine Polyamines Influence endothelial function: - Reduce nitric oxide production - Promote AGE formation - Affect cell cycle and cause senescence Appetite suppressants (leptin, cholecystokinin, tryptophan) 2. Reduced inflammation and oxidative stress 1. 2. 3. 4. reduces inflammation ( TNF, IL-6, IL-8, IL-12) suppresses oxidative stress ( reactive oxygen species and superoxide) improves antioxidant capacity reduces generation of AGEs Mechanisms 1. Biocompatible membranes 2. ‘Ultrapure’ dialysate 3. Removal of cytokines Chronic low-grade exposure to endotoxins Chronic inflammation Anorexia, poor nutrition and growth, catabolism, loss of lean body mass – cachexia Anaemia – poor ESA response Risk of atherosclerosis Malnutrition – inflammation – atherosclerosis complex Improved anaemia control on HDF Hemoglobin values and need for transfusions HD (12 months) HDF (12 months) 7.4 8.3 Number of transfusions for the whole group 32 (mean 5) 12 (mean 2) Membrane Cuprophane Polyacrylonitrile 3x5 h 3x3 h Hb g/dl Duration (sessions) Fischbach et al; Ped Nephrol 1984 3. Hemodynamic stability 1. 2. 3. 4. Fewer intra-dialytic hypotensive episodes Higher UF better tolerated by patient Reduced post-dialysis fatigue Overall better BP control Mechanisms: 1. Cooling of dialysate 2. Removal of vasodilating mediators 3. High Na content of infusion fluid Cardiovascular and survival advantage of HDF vs HD 1. Dutch HDF Study: CONTRAST 1,2 Hazard Ratio 1,0 0,8 p=0.016 0,6 0,4 0,2 0,0 lowflux HD < 15.5 L 15.5-20.3 L online HDF >20.3 L 2. Turkish HDF Study: High vs Low Efficiency HDF 3. Spanish HDF Study: High vs Low Efficiency HDF switching 8 patients from HD to HDF prevents one death / year Regression of LVH on daily HDF 2D Graph 33 2D Graph Interventricular Septum 14 14 12 12 12 10 10 10 8 8 8 6 Y Data 14 Y Data Y Data 2D Graph 3 Posterior Wall thickness 6 6 4 4 4 2 2 2 O 0 0 0 6M 12M 0 1 1 X Data O 6M 12M 0 0 2 2 1 1 X Data X Data Fischbach et al; NDT 2004 Growth on HDF Fischbach et al, NDT 2010 Nutrition & growth in children on dialysis Growth failure is a common end point of multiple CKD-related abnormalities : • • Malnutrition – anorexia and reduced energy intake Cachexia - protein energy wasting - due to chronic inflammation and inadequate dialysis 35 - 50 % of children with ESRD grow up to become short adults (final height <3rd centile) Growth study in children 15 children on daily HDF; mean age: 7.3 (2.8 – 16.7 yrs) 7 converted from PD & 5 from 3/week HD Vascular access: fistula (n=13) & catheter (n=4) Pre-dilution HDF; Qb & Qd adjusted to achieve a Kt/Vurea ≥1.4 per session x 18 hours per week Fischbach et al; NDT, 2010 Growth on daily HDF NOTE: - High convective volume - Daily HDF Height SDS start: -1.5 ± 0.3 - end: +0.2 ± 1.1 - target height relative to midparental height: +0.3 - Height velocity - before daily HDF: 3.8 ±1.1 cm/y - first year of daily HDF: 14.3 ± 3.8 cm/ - mean : 10.4 cm/y Fischbach et al; NDT, 2010 Dialysis efficiency & tolerance Mean weekly Kt/Vurea =10 - dialysis dose ~ 35% GFR Phosphate: 1.39 (1.65 - 0.63) mmol/l - despite high protein intake (>2 g/kg/day) - 2/15 child on chelators CRP – normal in 13/15 (2 children had chronic infections) β2 microglobulin 13.5 ± 3.5 mg/L Diet and medications Start of daily HDF (n= 12) Diet Antihypertensive drugs Potassium chelators After 1 year on daily HDF (n=12) Restricted Free (water, salt, proteins) 10/12 (>2 drugs/patient) 2/12 (1 drug/patient) 12/12 4/12 (only on dialysis free day) Phosphate chelators Post dialysis recovery time 12/12 6 to 15 min 1/12 No post-dialysis recovery time No sleep disturbances Improved appetite Improved physical activity Improved school attendance Dialysis dose and growth Daugirdas et al; Clin JASN 2010 Anabolic effect of daily HDF Stimulates appetite - removal of circulating satiety factors (leptin, cholecystokinin, tryptophan) Correction of metabolic acidosis. Acidosis can: - activate the ubiquitin-proteosome pathway & increase protein degradation - suppresses endogenous GH secretion Minimises inflammatory cytokine release ? Removal of somatomedin and gonadotropin inhibitors by HDF ? reverses rhGH resistance Schaefer et al, NDT 2010 HDF in an in-centre nocturnal dialysis programme n = 7 children Convective volume per session was > 30 liters Thumfart T, Muller D et al; Ped Nephrol 2014 Nocturnal HD vs HDF x 3/wk 120 100 80 60 Kt/V 40 20 HD NHD NHDF 0 NHD 450 HD NHD NHDF NHD 400 350 300 250 200 150 Phosphate 100 50 0 iPTH Paediatric HDF in Europe n=454 n=808 n=1281 n=2226 n=2494 % prevalent patients on RRT <18 yrs from 2007Percentage - 2012 of patients 100 Tx PD HD 80 60 40 20 144 cases of HDF in children in 2012 (~12% of all HD cases) 0 < 2 years 2-5 years 6-10 years 11-15 years > 15 years Age category ESPN/ERA-EDTA registry Survey on current dialysis practice across Europe 47 responses 4 5 6 1 3 4 2 8 3 13 16 1 1 2 19 19 13 11 2 HD – 210 children HDF – 125 children ESPN/ERA-EDTA registry ~144 children on HDF across Europe Choice of HD vs HDF Reasons for not doing HDF Total – 19 responses 43% Lack of machines Lack of ‘ultrapure’ water Cost Staff not trained HDF is not better / safe Vascular access does not permit HDF Multiple reasons Type of access (% patients per centre) Central line median 62 (IQR 0 – 84) % Fistula median 30 (IQR 0 – 60) % Potential limitations for setting up HDF 1. HDF machine X newer machines can all do HDF - one time installation cost, then 1-3 monthly monitoring - must use ultrapure water with all high flux membranes 2. Water quality 3. Staff training X provided by Fresenius / Gambro 4. Costs €40 /patient/month more than HD 5. No paediatric data We need a study! The effects of HDF vs conventional HD on growth and cardiovascular markers in children n 3H (HDF, Hearts and Height) study International Pediatric Hemodialysis Network Hypothesis Children on HDF compared with HD have improved: Cardiovascular risk profile Growth and nutritional status Quality of life Rukshana.Shroff@gosh.nhs.uk Primary outcome measures: Change in carotid artery intima-media thickness SDS over 1year Change in height SDS over 1-year Secondary outcome measures: Nutritional status, cardiovascular status and quality of life Inclusion criteria: All children 4 - 20 years age (incident and prevalent patients) Kt/v>1.2 in prevalent HDF and HD patients Exclusion criteria: if living donor kidney transplant is planned within 6-months Study design 1:1 study design Recruitment for 2 years, follow-up minimum 12-months Numbers needed 150 children (75 in each study arm) Standard prescriptions for HDF and HD Aim for target convection volume of 12-15L/m2 (post-dilution) Dialysate purity equivalent in HD & HDF Summary HDF offers many advantages over HD - improved clearance of uraemic toxins - biocompatibility - hemodynamic stability HDF is not widely practiced in children Ongoing study to examine effects of HDF on growth and cardiovascular outcomes Thank you! Participation in Clinical Trial Rukshana.Shroff@gosh.nhs.uk Participation in IPHN Registry Claus.Peter.Schmitt@med.uni-heidelberg.de International Pediatric Hemodialysis Network