Non−caregiver - Kantar Health
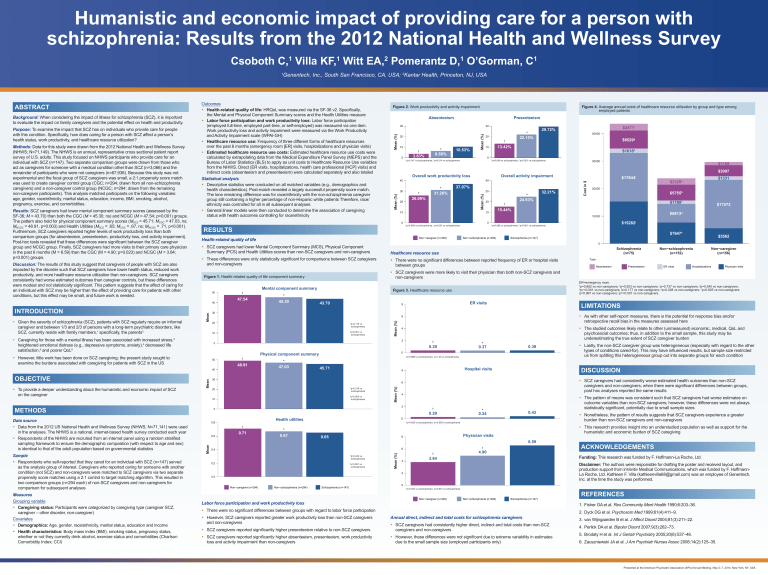
advertisement
Humanistic and economic impact of providing care for a person with schizophrenia: Results from the 2012 National Health and Wellness Survey Csoboth C, Villa KF, Witt EA, Pomerantz D, O’Gorman, C 1 Discussion: The results of this study suggest that caregivers of people with SCZ are also impacted by the disorder such that SCZ caregivers have lower health status, reduced work productivity, and more healthcare resource utilization than non-caregivers. SCZ caregivers consistently had worse estimated outcomes than caregiver controls, but these differences were modest and not statistically significant. This pattern suggests that the effect of caring for an individual with SCZ may be higher than the effect of providing care for patients with other conditions, but this effect may be small, and future work is needed. 40 30 20 3.83% Mean (%) 0 *p=0.147 vs schizophrenia; †p=0.014 vs schizophrenia Overall work productivity loss * 31.26% † 26.09% $1618h *p=0.049 vs schizophrenia; †p<0.001 vs schizophrenia 30 20 * 24.93% † 32.21% 47.54 0 *p=0.069 vs schizophrenia; p=0.001 vs schizophrenia † Mean 43.70 † 10 p=0.001 vs schizophrenia Non−schizophrenia (n=294) Mean 45.71 *p=0.218 vs schizophrenia p=0.003 vs schizophrenia Mean † Absenteeism Presenteeism ER visits Hospitalizations Physician visits LIMITATIONS * 0.37 0.39 • S CZ caregivers had consistently worse estimated health outcomes than non-SCZ caregivers and non-caregivers; when there were significant differences between groups, post hoc analyses reported the same results 4 † * 0.24 0.43 *p=0.428 vs schizophrenia; †p=0.555 vs schizophrenia 0.65 6.59 6 *p=0.244 vs schizophrenia 0.2 † p=0.001 vs schizophrenia † 4 * 4.90 Schizophrenia (n=147) Labor force participation and work productivity loss ACKNOWLEDGEMENTS Disclaimer: The authors were responsible for drafting the poster and received layout, and production support from inVentiv Medical Communications, which was funded by F. HoffmannLa Roche, Ltd. Kathleen F. Villa (kathleenvilla68@gmail.com) was an employee of Genentech, Inc. at the time the study was performed. 0 *p=0.023 vs schizophrenia; †p=0.001 vs schizophrenia Non−caregiver (n=294) Non−schizophrenia (n=294) Schizophrenia (n=147) REFERENCES 1. Fisher GA et al. Res Community Ment Health 1990;6:203–36. • There were no significant differences between groups with regard to labor force participation • However, SCZ caregivers reported greater work productivity loss than non-SCZ caregivers and non-caregivers • N onetheless, the pattern of results suggests that SCZ caregivers experience a greater burden than non-SCZ caregivers and non-caregivers Funding: This research was funded by F. Hoffmann-La Roche, Ltd. 3.84 2 0.0 • T he pattern of means was consistent such that SCZ caregivers had worse estimates on outcome variables than non-SCZ caregivers; however, these differences were not always statistically significant, potentially due to small sample sizes • T his research provides insight into an understudied population as well as support for the humanistic and economic burden of SCZ caregiving Physician visits 8 0.4 • L astly, the non-SCZ caregiver group was heterogeneous (especially with regard to the other types of conditions cared-for). This may have influenced results, but sample size restricted us from splitting this heterogeneous group out into separate groups for each condition DISCUSSION 0 Health utilities Non−schizophrenia (n=294) Type negative symptoms with health outcomes Hospital visits 0.29 Non−caregiver (n=294) Non−caregiver (n=156) • T he studied outcomes likely relate to other (unmeasured) economic, medical, QoL and psychosocial outcomes; thus, in addition to the small sample, this study may be underestimating the true extent of SCZ caregiver burden 2 0 0.71 Non−schizophrenia (n=152) 4 8 10 0.6 $5562 ER=emergency room. a p=0.882 vs non-caregivers; bp=0.503 vs non-caregivers; cp=0.737 vs non-caregivers; dp=0.540 vs non-caregivers; e p=<0.001 vs non-caregivers; fp=0.177 vs non-caregivers; gp=0.028 vs non-caregivers; hp=0.825 vs non-caregivers; i p=0.997 vs non-caregivers; jp=<0.001 vs non-caregivers. *p=0.898 vs schizophrenia; †p=1.00 vs schizophrenia 20 * 0.67 $7647e Schizophrenia (n=75) 6 † $15282j Schizophrenia (n=147) 0 Physical component summary 30 0.8 $6813d • A s with other self-report measures, there is the potential for response bias and/or retrospective recall bias in the measures assessed here 0.39 † METHODS $17573 6 2 0 48.91 $1180c *p=0.086 vs schizophrenia; p<0.001 vs schizophrenia ER visits 8 *p=0.172 vs schizophrenia * 47.03 $5755b † Figure 3. Healthcare resource use 20 50 20000 $2329 $1331 a 0 30 † $17644i • SCZ caregivers were more likely to visit their physician than both non-SCZ caregivers and non-caregivers Mental component summary * 45.30 $3997 10000 Non−caregiver (n=294) Figure 1. Health-related quality of life component summary † $1189 15.44% 10 • There were no significant differences between reported frequency of ER or hospital visits between groups 50 30000 Overall activity impairment 40 37.07% 10 13.42% 10 Cost in $ 0 40000 $6529g • T hese differences were only statistically significant for comparisons between SCZ caregivers and non-caregivers and caregivers across psychosocial, SCZ treatment and medical outcomes Measures Grouping variable • Caregiving status: Participants were categorized by caregiving type (caregiver SCZ, caregiver – other disorder, non-caregiver) Covariates • Demographics: Age, gender, race/ethnicity, marital status, education and income • Health characteristics: Body mass index (BMI), smoking status, pregnancy status, whether or not they currently drink alcohol, exercise status and comorbidities (Charlson Comorbidity Index; CCI) † 10.53% † Healthcare resource use symptoms, specifically, on treatment/service use and medical outcomes in these groups Sample • Respondents who self-reported that they cared for an individual with SCZ (n=147) served as the analysis group of interest. Caregivers who reported caring for someone with another condition (not SCZ) and non-caregivers were matched to SCZ caregivers via two separate propensity score matches using a 2:1 control to target matching algorithm. This resulted in two comparison groups (n=294 each) of non-SCZ caregivers and non-caregivers for comparison for subsequent analyses * 6.58% * 22.15% 20 $2471f 29.72% • S CZ caregivers had lower Mental Component Summary (MCS), Physical Component Summary (PCS) and Health Utilities scores than non-SCZ caregivers and non-caregivers 40 Data source • Data from the 2012 US National Health and Wellness Survey (NHWS; N=71,141) were used in the analyses. The NHWS is a national, internet-based health survey conducted each year • Respondents of the NHWS are recruited from an internet panel using a random stratified sampling framework to ensure the demographic composition (with respect to age and sex) is identical to that of the adult population based on governmental statistics 10 Health-related quality of life • H owever, little work has been done on SCZ caregiving; the present study sought to examine the burdens associated with caregiving for patients with SCZ in the US • T o provide a deeper understanding about the humanistic and economic impact of SCZ on the caregiver 30 20 RESULTS • C aregiving for those with a mental illness has been associated with increased stress,3 heightened emotional distress (e.g., depressive symptoms, anxiety),4 decreased life satisfaction,5 and poorer QoL6 OBJECTIVE Presenteeism 30 0 schizophrenia caregivers. • G iven the severity of schizophrenia (SCZ), patients with SCZ regularly require an informal caregiver and between 1/3 and 2/3 of persons with a long-term psychiatric disorders, like SCZ, currently reside with family members,1 specifically, the parents2 Absenteeism negative symptoms with health outcomes 40 INTRODUCTION Figure 4. Average annual costs of healthcare resource utilization by group and type among employed patients Mean (%) Results: SCZ caregivers had lower mental component summary scores (assessed by the SF-36; M = 43.70) than both the CGC (M = 45.30; ns) and NCGC (M = 47.54; p=0.001) groups. The pattern also held for physical component summary scores (MSCZ = 45.71; MCGC = 47.03, ns; MNCGC = 48.91, p=0.003) and Health Utilities (MSCZ = .65; MCGC = .67, ns; MNCGC = .71, p<0.001). Furthermore, SCZ caregivers reported higher levels of work productivity loss than both comparison groups (for absenteeism, presenteeism, productivity loss, and activity impairment). Post-hoc tests revealed that these differences were significant between the SCZ caregiver group and NCGC group. Finally, SCZ caregivers had more visits to their primary care physician in the past 6 months (M = 6.59) than the CGC (M = 4.90; p=0.023) and NCGC (M = 3.84; p<0.001) groups. Statistical analysis • Descriptive statistics were conducted on all matched variables (e.g., demographics and health characteristics). Post-match revealed a largely successful propensity score match. The lone remaining difference was for race/ethnicity with the non-schizophrenia caregiver group still containing a higher percentage of non-Hispanic white patients Therefore, race/ ethnicity was controlled for all in all subsequent analyses • General linear models were then conducted to determine the association of caregiving status with health outcomes controlling for race/ethnicity Figure 2. Work productivity and activity impairment Mean (%) Methods: Data for this study were drawn from the 2012 National Health and Wellness Survey (NHWS; N=71,149). The NHWS is an annual, representative cross sectional patient report survey of U.S. adults. This study focused on NHWS participants who provide care for an individual with SCZ (n=147). Two separate comparison groups were drawn from those who act as caregivers for someone with a medical condition other than SCZ (n=3,066) and the remainder of participants who were not caregivers (n=67,936). Because this study was not experimental and the focal group of SCZ caregivers was small, a 2:1 propensity score match was used to create caregiver control group (CGC; n=294; drawn from all non-schizophrenia caregivers) and a non-caregiver control group (NCGC; n=294; drawn from the remaining non-caregiver participants). This analysis matched participants on the following variables: age, gender, race/ethnicity, marital status, education, income, BMI, smoking, alcohol, pregnancy, exercise, and comorbidities. Outcomes • Health-related quality of life: HRQoL was measured via the SF-36 v2. Specifically, the Mental and Physical Component Summary scores and the Health Utilities measure • Labor force participation and work productivity loss: Labor force participation (employed full-time, employed part-time, or self-employed) was measured via one item. Work productivity loss and activity impairment were measured via the Work Productivity and Activity Impairment scale (WPAI-GH) • Healthcare resource use: Frequency of three different forms of healthcare resources over the past 6 months (emergency room [ER] visits, hospitalizations and physician visits) • Estimated healthcare resource use costs: Estimated healthcare resource use costs were calculated by extrapolating data from the Medical Expenditure Panel Survey (MEPS) and the Bureau of Labor Statistics (BLS) to apply as unit costs to Healthcare Resource Use variables from the NHWS. Direct (ER visits, hospitalizations, health care professionsl [HCP] visits) and indirect costs (absenteeism and presenteeism) were calculated separately and also totaled Mean (%) Purpose: To examine the impact that SCZ has on individuals who provide care for people with this condition. Specifically, how does caring for a person with SCZ affect a person’s health status, work productivity, and healthcare resource utilization? 1 Genentech, Inc., South San Francisco, CA, USA; 2Kantar Health, Princeton, NJ, USA Mean (%) Background: When considering the impact of illness for schizophrenia (SCZ), it is important to evaluate the impact on family caregivers and the potential effect on health and productivity. 1 Mean (%) ABSTRACT 2 Mean (%) 1 1 Annual direct, indirect and total costs for schizophrenia caregivers • SCZ caregivers reported significantly higher presenteeism relative to non-SCZ caregivers • SCZ caregivers had consistently higher direct, indirect and total costs than non-SCZ caregivers and non-caregivers • SCZ caregivers reported significantly higher absenteeism, presenteeism, work productivity loss and activity impairment than non-caregivers • However, these differences were not significant due to extreme variability in estimates due to the small sample size (employed participants only) 2. Dyck DG et al. Psychosom Med 1999;61(4):411–9. 3. van Wijngaarden B et al. J Affect Disord 2004;81(3):211–22. 4. Perlick DA et al. Bipolar Disord 2007;9(3):262–73. 5. Brodaty H et al. Int J Geriatr Psychiatry 2005;20(6):537–46. 6. Zauszniewski JA et al. J Am Psychiatr Nurses Assoc 2008;14(2):125–35. Presented at the American Psychiatric Association (APA) Annual Meeting, May 3–7, 2014, New York, NY, USA