Get Started with ENA`s FAQs - Emergency Nurses Association
advertisement

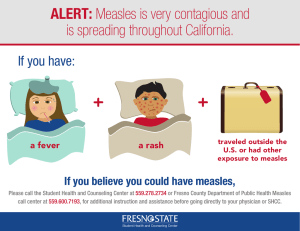
Measles Frequently Asked Questions 1. What are the signs and symptoms of measles? Symptoms of measles include high fever, cough, runny nose, and red, watery eyes that generally occur 7–14 days after a person is infected. Koplik spots (tiny white spots) may appear inside the mouth 2 or 3 days after symptoms begin. A rash typically develops 3–5 days after the onset of symptoms.1 2. How long after exposure does it take to show signs of measles? It typically takes an average of 10–12 days from exposure to the first symptom, which generally is a high fever.1 The measles rash will usually appear approximately 14 days after exposure, which is about 3–5 days after the fever begins.1 3. What does the measles rash look like? The measles rash is a maculopapular eruption that usually lasts 5–6 days.2 The rash generally begins as flat red spots that develop on the face at the hairline and spread downward to the neck, trunk, arms, legs, and feet.2 Initially, the lesions will blanch with fingertip pressure, but by day 3–4, most do not blanch with pressure at all.2 Small, raised bumps or maculopapular lesions are generally discrete but can also appear on top of the flat red spots and become confluent as they spread from the head to the rest of the body.2 It is important to note that immunocompromised individuals may not always develop a rash.3 Visit this CDC webpage to view photographs of people with measles. 4. How is measles transmitted from person to person? Measles is spread through the air by infectious droplets produced from the coughing, sneezing, or talking of infected individuals. The droplets can remain infectious in the air and on surfaces for up to 2 hours.4 5. How contagious is measles? Measles is a highly contagious airborne virus than can survive for up to 2 hours on surfaces or in airspace that has been exposed to an infected person.4 If others who are not immune breathe contaminated air or touch infected surfaces and subsequently touch their eyes, nose, or mouth, they have a 90% probability of becoming infected with measles.4 6. How long is measles contagious for? Infected individuals with measles can spread the virus to others from 4 days before the rash is visible to 4 days after it appears.2 7. Who is at high risk for measles and complications? Individuals at high risk for complications and severe illness from measles include3: • Infants and children less than 5 years of age • Individuals who have not been vaccinated • Adults older than 20 years of age • Pregnant women • Individuals with compromised immune systems 8. What is evidence of immunity from measles? How do I know if I am protected against measles? It is acceptable presumptive evidence of immunity and you are considered protected from measles if you meet at least one of the following criteria:3 • • • • Born in the U.S. before 1957 Laboratory evidence of immunity to measles, mumps, and/or rubella Laboratory confirmation of actually having had the disease at some point Written documentation of adequate vaccination that includes: o One or more doses of a measles-containing vaccine administered on or after the first birthday for preschool-age children and adults not at high risk o Two doses of measles-containing vaccine for school-age children and adults at high risk, including college students, healthcare personnel, and international travelers 9. How is measles confirmed? Measles diagnosis is confirmed by the patient’s symptoms and laboratory tests. Detection of measles-specific IgM antibody or of measles RNA by reverse transcription polymerase chain reaction (RT-PCR) are the most common methods for confirming measles infection.3 Healthcare providers should obtain serum samples and a throat or nasopharyngeal swab from individuals suspected of having measles.3 Urine samples may also contain the measles virus. When feasible, collecting both respiratory and urine samples can increase the likelihood of detecting measles virus. However, some facilities may not have laboratory capabilities for testing the measles virus; it is therefore important to review individual laboratory policies and procedures to know how and where testing will be conducted. For more information, review the CDC’s measles lab tools. 10. What should I be asking during triage assessment to better identify measles? First, assess every patient presenting to your emergency department triage or via ambulance for a potential exposure history: Ask if they have had any recent international travel, contact with foreign visitors, transit through an international airport, or possible exposure to a measles patient within the 3 weeks prior to the onset of their symptoms. Identify if the patient has any signs or symptoms consistent with measles (high fever, cough, runny nose, and red, watery eyes, Koplik spots, or rash).1 11. After I have identified a suspected measles patient in triage, what should I do next? If measles is suspected, immediately mask the patient. For infants and children, place a blanket loosely over their heads as a practical means for containment while they are being transported from common areas to an isolation room. Suspected measles patients should not be allowed to remain in the waiting area or other common areas; it is critical to immediately isolate these individuals in an airborne infection isolation room (AIIR).3 Simultaneously, notify the appropriate personnel, which may include your nurse manager, hospital infection control, and other medical staff. Notify the local health department immediately of any suspect measles patients and arrange for measles testing at a public health laboratory.3 Be sure to review your individual hospital policies and procedures for more information. 12. What other steps need to be taken once a suspected measles patient is taken from triage to an airborne isolation room? It is important to document the names and contact information of all staff, visitors, and other patients who were in the triage area, who cared for, or who were in contact with the suspected measles patient during the time the patient was in the facility and for the two hours after the patient departed the area. If measles is confirmed in the suspected case, the exposed individuals will need to be assessed for measles immunity. 13. What personal protective equipment is necessary when caring for suspected or confirmed measles patients? According to CDC recommendations, personal protective equipment (PPE) for measles in healthcare settings should follow respiratory precautions, regardless of presumptive immunity status.3 All healthcare staff entering a suspected/confirmed measles patient’s room should use respiratory protection consistent with airborne infection control precautions, including the use of a National Institute for Occupational Safety and Health (NIOSH) N95 respirator or one with similar effectiveness in preventing airborne transmission.3 While the possibility of MMR vaccine failure is low for healthcare providers exposed to measles-infected patients, providers should still observe all airborne precautions in caring for these patients.3 CDC recommends the placement of patients who require airborne precautions in single-patient airborne infection isolation rooms (AIIR).3 14. Should suspected or confirmed measles patients be allowed visitors in their rooms while in the ED? Family presence can provide emotional support and comfort, and there are also benefits for the nurses.5 If possible, however, susceptible family members or visitors should not be allowed in the patient’s room for risk of further disease transmission. 15. What should I do for post-exposure prophylaxis for staff in the ED? Notification of the exposure should be communicated according to your hospital or facility’s policies and procedures, which may include follow-up with your employee health services. Individuals who have not been vaccinated and those for whom contracting measles would be particularly dangerous, such as pregnant women with no evidence of immunity, or individuals with severely compromised immune systems, should receive immune globulin (IG) within 72 hours of exposure.3,6 Immune globulin (IG) may prevent or lessen the severity of measles if administered within six days of exposure and should be given when available.3,6 16. As a healthcare provider, if I have chosen not to be vaccinated or do not have evidence of immunity to measles and was exposed to the disease, can I continue to work? According to the CDC, in healthcare settings, it is recommended to exclude healthcare personnel with no evidence of immunity from duty from day 5 after first exposure to day 21 after last exposure, regardless of post-exposure vaccination.3 Review your individual institutional policies and procedures for more information. 17. If I cared for a patient with confirmed measles or was exposed to measles but I have evidence of immunity, will I need a booster vaccine? No. Individuals who have received two doses of measles vaccine as children are considered immune for life and do not require a booster dose.7 However, healthcare personnel working in settings that pose a high risk for measles transmission should ensure they have had two doses separated by at least 28 days.3,6 18. If I cared for a suspected or confirmed measles patient in my ED, what postexposure isolation or quarantine measures should I take to protect my family, friends, caregivers, or anyone else close to me, especially if they haven’t been vaccinated or are considered high risk? Consult with your hospitals infectious disease professional or your personal healthcare provider for direction. References: 1. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. (2015). Signs and symptoms of measles. Retrieved from http://www.cdc.gov/measles/about/signs-symptoms.html 2. Centers for Disease Control and Prevention. (2011). Chapter 12: Measles. In W. Atkinson, S. Wolfe, & J. Hamborsky (Eds.). Epidemiology and prevention of vaccinepreventable diseases (12th ed.). Washington, DC: Public Health Foundation. 3. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. (2014). Measles (rubeola): For healthcare professionals. Retrieved from http://www.cdc.gov/measles/hcp/index.html 4. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. (2014). Measles (rubeola): Transmission of measles. Retrieved from http://www.cdc.gov/measles/about/transmission.html 5. Lowry, E. (2012). “It's just what we do”: A qualitative study of emergency nurses working with well-established family presence protocol. Journal of Emergency Nursing, 38(4), 329–334. doi:10.1016/j.jen.2010.12.016 6. McLean, H. Q., Fiebelkorn, A. P., Temte, J. L., & Wallace, G. S. (2013). Prevention of measles, rubella, congenital rubella syndrome, and mumps, 2013: Summary recommendations of the Advisory Committee on Immunization Practices (ACIP). Morbidity and Mortality Weekly Report, 62(4), 1–34. 7. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. (2014). Frequently asked questions about measles in the U.S. Retrieved from http://www.cdc.gov/measles/about/faqs.html