CLINICAL RESEARCH
Europace (2014) 16, 1787–1794
doi:10.1093/europace/euu079
Leads and lead extraction
Mechanical and electrical dysfunction of Riata
implantable cardioverter-defibrillator leads
Fatma Demirel, Ahmet Adiyaman, Peter Paul H.M. Delnoy,
Jaap Jan J. Smit, Anand R. Ramdat Misier, and Arif Elvan*
Department of Cardiology, Isala Klinieken, Dr. Van Heesweg 2, 8025 AB, Zwolle, The Netherlands
Received 9 January 2014; accepted after revision 24 March 2014; online publish-ahead-of-print 19 May 2014
Aim
----------------------------------------------------------------------------------------------------------------------------------------------------------Keywords
Intracardiac cardioverter-defibrillator † Lead failure † Externalization † Electrical lead failure
Introduction
In December 2011, the US food and drug administration classified
a device advisory regarding the poor performance of the Riata
intracardiac cardioverter-defibrillator (ICD) shock leads as a
Class I recall.1 The manufacturer (St. Jude Medical) stopped the
distribution of these defibrillation leads in 2010, of which the
total number sold worldwide is estimated to be 227.000 over a
period of 9 years.
Insulation abrasion is the most common cause of ICD lead
failure.2 Riata leads are prone to a unique form of failure mechanism with abrasions of the silicone insulation (inside-out abrasion).
The high- and/or low-voltage conductors wear through the silicone insulation resulting in externalization and possible electrical
dysfunction.3
The rates of conductor externalization have been noted to range
between 11 and 22% with a higher prevalence seen among the 8 Fr.
Riata leads.4 – 13 Moreover, in addition to structural failure, Riata leads
have been shown to have higher rates of electrical failure when compared with standard diameter ICD leads.14,15 Nowadays, the clinical
predictors and pattern in the time of the Riata lead for structural and
electrical failure are not well known. The consequences of externalization without electrical abnormalities remain uncertain. In this study, we
sought to:
(i) identify the clinical predictors of Riata lead failure (electrical
and/or structural).
(ii) determine the association between structural and electrical
failure of the Riata lead.
(iii) analyse the rates of structural and electrical failure over time.
* Corresponding author. Tel: +31 384242374; fax: +31 384243222. E-mail address: v.r.c.derks@isala.nl
Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2014. For permissions please email: journals.permissions@oup.com.
Downloaded from by guest on September 30, 2016
Riata implantable cardioverter-defibrillator leads are prone to failure by conductor externalization and/or electrical
dysfunction. The objectives of this study were to determine the predictors of the Riata lead failure, to assess the association of conductor externalization and electrical lead failure, and to analyse the rates of lead failure over time.
.....................................................................................................................................................................................
Methods
Of 273 implanted Riata leads in our centre, 197 were investigated according to the Riata recall protocol, including
electrical measurements by device interrogation and annually fluoroscopy. During a mean follow-up period of
and results
5.6 + 1.4 years, Riata lead failure was 18.8% (37 of 197) for externalization and 17.3% (34 of 197) for electrical
lead failure. Electrical lead failure was correlated with time after implant. Externalization and electrical dysfunction
co-existed in only 6 of 197 (3%) patients and were not related (Phi’s coefficient 20.013, P ¼ 0.85). During the second
annual screening, 145 (73.6%) patients underwent fluoroscopy and 9 patients had novel externalizations resulting in
an incidence of 6.72%/patient/year which was higher than expected based on cross-sectional analysis. Besides, there
was a significant increase in the extent of externalization (17.65 + 11.14 mm vs. 21.77 + 11.95 mm, P ¼ 0.001). In multivariate Cox regression analysis, non-ischaemic cardiomyopathy and impaired LVEF were independent predictors of
externalization, and 7 Fr lead was a predictor of electrical lead failure.
.....................................................................................................................................................................................
Conclusion
Riata leads show progressive and high externalization rates without correlation between externalization and electrical
lead failure. Non-ischaemic cardiomyopathy and impaired LVEF are independent predictors of structural lead failure in
cross-sectional analysis, whereas 7 Fr lead is a predictor of electrical lead failure.
1788
What’s new?
† We describe the results of longitudinal follow-up showing an
increase of externalization rate and an increase in the extent of
externalization over time and the lack of association between
externalization and electrical dysfunction.
† Identification of predictors for Riata lead failure, i.e. nonischaemic cardiomyopathy and impaired LVEF for structural
lead failure and 7 Fr for electrical lead failure.
Methods
Chest radiography and Fluoroscopy
Cine-fluoroscopy was performed in all patients using several projections
including anterior– posterior, left-anterior-oblique 458, and rightanterior-oblique 458, and additional projections as needed for optimal
identification of conductor externalization. The projections were examined at the time of image acquisition and reviewed by a team of cardiac
electrophysiologists with extensive experience in device implantation
and lead cine fluoroscopy.
Intracardiac cardioverter-defibrillator
interrogation
In all patients, ICD interrogation was performed with measurement of
low and high-voltage impedances, sensing and capture threshold
values. Furthermore, all measurements were repeated during manipulation of the pocket/device and during isometric arm exercise. The device
was additionally reviewed for inappropriate sensing events (noise and
oversensing). During follow-up, several device interrogations (outpatient
clinic visits with 6 months intervals or shorter when indicated, and
remote-monitoring) took place.
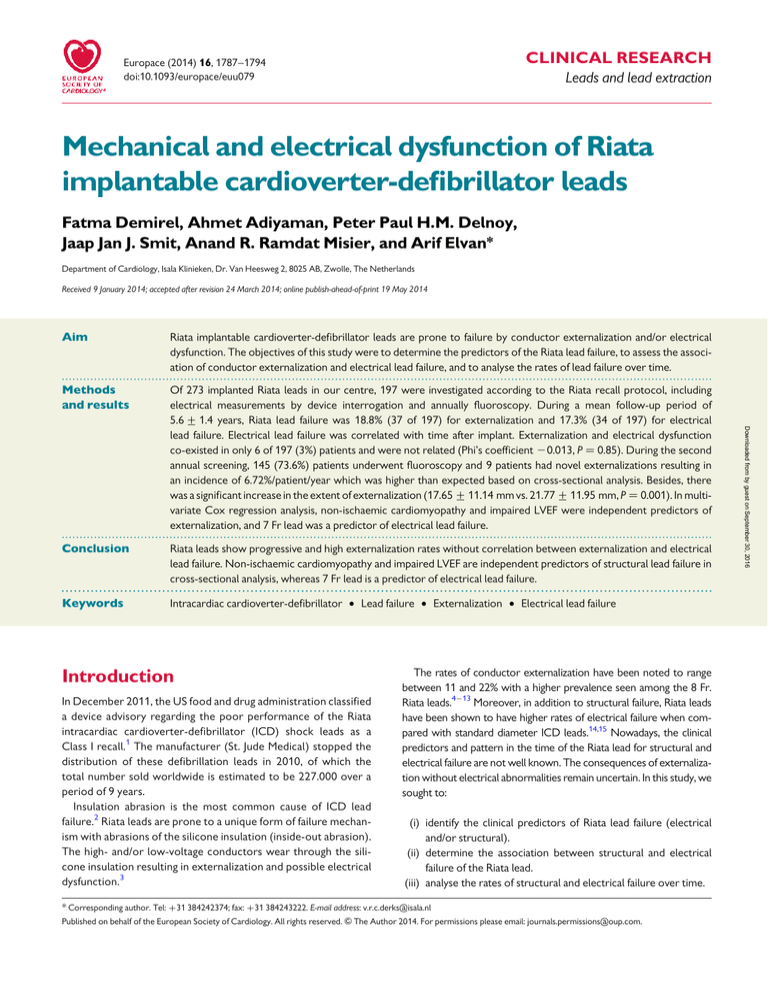
Definition of structural failure of the Riata lead
Externalization was defined as conductor(s) visible outside the lead body
on fluoroscopy in any of the projected views. The location of externalization was divided into four zones (Figure 1). The size of externalization was
described in length by mm fluoroscopically calibrated for the thickness
of the lead. The length of the externalization is measured on the projection with the largest visual length and controlled in the other available
projections.
Definition of electrical lead failure
Electrical lead failure was considered if it met one of the following criteria:
(i). presence of non-physiological signals on the intracardiac ventricular
electrogram, (ii) pacing impedance outside the interval 200 – 2000 V or
.100% increase or .50% decrease of the stable baseline impedance,
(iii) change in high-voltage impedance to .200 or ,25 V, (iv) pacing
threshold .5 V or .100% increase, (v) R-wave sensing ,3.0 mV or
.50% reduction. Lead dislodgment, T-wave oversensing, physiological
oversensing, and header problems were not considered as lead failures.
Adverse events were defined as an inappropriate shock or failure of
pacing or defibrillation, caused by lead dysfunction.
For survival analysis, the date of lead failure was identified using device
interrogation as the first occurrence of any lead abnormality fulfilling the
definition of lead failure as stated above.
Statistical analysis
Continuous variables are expressed as mean + SD and significant differences were analysed by Student’s t-test or Mann– Whitney U test.
Categorical data are expressed as number and percentages and compared with x2 test or Fischer’s exact test, when appropriate. We tested
the variables for normally distribution by skewness and kurtosis and
plotted with P– P and Q– Q plots. We used Spearman’s correlation for
continuous variables, when not normally distributed and Phi’s coefficient
for nominal binary variables. To identify the baseline characteristics associated with adverse outcome (electrical and/or structural lead failure),
univariate and multivariate Cox proportional hazards regression analysis
was performed. Before entering the covariates in the multivariate
Cox regression model, we assessed co-linearity between covariates.
We only entered covariates that were not significantly intercorrelated
(R: 0.06 20.23 and VIF: 1.000– 1.089).
Multivariate Cox regression analysis was performed with a forward
conditional model of variables and removal of variables at a P-value of
0.15, with externalization or electrical dysfunction as dependent
variables. Gender, lead size (7 or 8 French), type of cardiomyopathy
(ischaemic vs. non-ischaemic) and left ventricular ejection fraction
(LVEF) were used as covariates. Relative risk was expressed as hazard
ratio (HR) with associated 95% confidence interval (CI). Statistical
analysis was performed using SPSS version 20. A P-value of ,0.05 was
considered statistically significant.
Results
Clinical characteristics
At the time of recall we could analyse 197 patients, because 68
patients were deceased and 8 patients were lost to follow up (migration of the patient or inability of the patient to attend the check-up).
In the deceased patients, there were no reports of lead externalization or lead dysfunction in the medical records. The study population
consisted of 32 females (16.2%) and 165 males (83.8%), mean age
was 70.4 + 10.1 years. The median follow-up was 5.8 years (IQR,
5.1 –6.4 years) and the mean follow-up was 5.6 + 1.4 years. The
mean follow-up was significantly longer for the Riata 8 Fr than for
the 7 Fr Riata ST (6.6 + 1.2 years vs. 5.2 + 1.3 years; P , 0.0001).
The 7 Fr Riata ST lead was more prevalent (69%). The majority of
the screened leads had a single coil design (59%). Twenty-seven
of the 197 patients underwent lead revision prior to the formal
Riata recall due to several reasons, i.e. 15 patients had electrical
lead failure, 2 patients had lead dislocation, 2 patients had lead perforation, 7 patients had lead related infection, 1 patient had an isolation
Downloaded from by guest on September 30, 2016
On 4 January 2012, a recommendation was given by the Device Advisory
Committee of the Netherlands Heart Rhythm Association (NHRA) to
identify all patients with an functional Riata or Riata ST lead and to
perform fluoroscopic screening and electrical interrogation of these
leads.16 According to the NHRA recommendation, a first screening
with fluoroscopy took place in 2012 and a second annual screening in
2013. We investigated all 273 patients who underwent implantation of
a Riata lead in our centre. This current study involves partly known
data which is published by Theuns et al.10 This current study is an analysis
of both retrospectively and prospectively collected data on all Riata
(Model 1580, 1581, 1582) and Riata ST (Model 7000, 7001, 7002) leads
implanted between February 2005 and February 2008 at the Isala Klinieken, Zwolle, the Netherlands. This prospective registry was approved by
the Hospital board. The collected data include the lead model, date of implantation, date of screening, presence of externalized conductors, location of externalized conductors, extent of externalization, presence of
electrical dysfunction, type of electrical dysfunction, and adverse events.
F. Demirel et al.
1789
Mechanical and electrical dysfunction of Riata leads
A
C
D
B
A3
A
A2
A
A1
B
A
N (%)
N (%) of
externalization
1(2.8)
A1
N (%)
A2
N (%)
16(44.4) 12(33.3)
A3
N (%)
B
N (%)
5(13.9)
1(2.8)
C
N (%)
1(2.8)
D
N (%)
1(2.8)
p-value
<0.001
Figure 1 (A) Location of externalization divided into four zones; A: Distal to SVC-coil (dual coil), distal to superior vena cava (single coil), divided
into A1: proximal RVC-coil; A2: tricuspid valve annulus; A3: distal SVC-coil to tricuspid valve annulus (dual coil), right atrium (single coil), B: distal to
clavicle including SVC-coil (dual coil) superior vena cava (single coil), C: near clavicle, D: clavicle to CAN. (B) Table showing the rates of externalization per zone.
defect that was observed during upgrading to a CRT system with
placement of a LV-lead, and 1 patient underwent preventive lead replacement at the time of device replacement due to elective replacement interval. Riata leads were successfully extracted in 14 of 27
patients without adverse events. In the 13 patients without extraction, the Riata lead was capped in situ. At the time of revision or extraction fluoroscopy was available in all patients.
First formal Riata recall screening
During the formal Riata recall, 170 patients underwent fluoroscopic
screening and ICD interrogation. The mean follow-up at the time of
fluoroscopy was 5.0 + 0.7 years. In 26 patients Riata lead externalization was documented during fluoroscopic screening. Of these 26
patients, 25 patients underwent lead revision, i.e. a new shock lead
was implanted and the Riata lead was capped. During follow-up, a
total of 51 lead revisions were performed. Of these patients, 14
underwent preventive revision at ERI and in 2 patients Riata lead extraction was performed. Sixteen patients died during follow-up and
31 patients were lost to follow-up (migration, clinical condition prohibiting patients to adhere to the recall).
Second formal Riata recall screening
During the second annual screening, 1 year after the first screening,
134 patients underwent fluoroscopy of whom 90 patients had a
functional Riata lead and 44 had a non-functional Riata lead. The
mean follow-up at the time of fluoroscopy was 6.1 + 0.8 years. Additionally nine leads showed novel externalizations and five leads had
developed electrical lead failure over a period of 1 year. Thus, a total
of 37 structural lead failures and 34 electrical lead failures were found
at the time of the last follow-up (Figure 2).
Externalization
Table 1 shows externalization rates and characteristics of the Riata/
Riata ST leads screened in 2012 and 2013. The prevalence of externalization was 14.2% (28 of 197) in 2012 and 18.8% (37 of 197) in
2013. Cross-sectional analysis showed a total externalization rate
of 3.35%/patient/year. In the longitudinal follow-up, 6.72% (9 of
134) patients showed novel externalization, suggesting a higher
externalization rate than in the cross-sectional analysis.
Eighteen patients (64.3%) who had fluoroscopically documented
externalization of the Riata leads in 2012, underwent a second fluoroscopic as part of the regular annual screening and showed an increase
in the extent of externalization over a period of 1 year (17.65 +
11.14 mm vs. 21.77 + 11.95 mm, P-value ¼ 0.001). The four zones
of externalization are shown in Figure 1. The most common place
of externalization was in the A zone, proximal to the RVC coil in
the right atrium, near the tricuspid valve (75.7%).
Downloaded from by guest on September 30, 2016
Location of
externalization
1790
F. Demirel et al.
273 riata leads implanted
68 pt deceased
8 pt lost to FUP
197 pt able to analyze
subcutaneously implanted device (P ¼ 0.02) had significantly more
externalization rates.
In univariate and multivariate Cox regression analysis, nonischaemic cardiomyopathy (HR 6.33; 95% CI: 3.07 –13.03; P ≤
0.001) and LVEF (HR 0.94; 95% CI: 0.91 –0.98; P ¼ 0.02) were identified as independent predictors of externalization of the Riata leads
(Table 3).
27 pt revision before recall (14 lead extraction)
–15 electrical lead failures ; 2 externalizations
Electrical lead failure
National screening of riata recall 2012
170ICD interrogations
173 fluoroscopic screening
(3 screening while revision)
26 additional externalizations
14 additional electrical lead failures
51 lead revisions after recall (2 lead
extraction)
16 pt deceased during 2012
31 pt lost to FUP for fluoroscopic screening
National second screening of riata recall 2013
134 leads
(90 active leads)
(44 non-active leads)
Total
37 externalizations
34 electrical lead failure
Figure 2 Flowchart of patient follow-up.
Table 2 shows that women had higher externalization rates than
men (31.2 vs. 16.4%, P ¼ 0.05) and 8 Fr Riata leads had more externalization than 7 Fr Riata ST leads (34.4 vs. 11.8%; P , 0.001). Furthermore, patients with impaired LVEF (P ¼ 0.05), non-ischaemic
cardiomyopathy (P , 0.001), biventricular ICD (P ¼ 0.003), and a
Table 1 Rates of externalization in 2012 and 2013
Model
Coils
N (%)
EX in 2012
(% within lead model)
Dwell time 2012
(years + SD)
EX in 2013
(% within lead model)
Dwell time 2013
(years + SD)
...............................................................................................................................................................................
8 Fr Riata leads
Riata 1580
Riata 1581
Dual
Dual
28 (14.2)
12 (6.1)
5 (17.9)
5 (41.7)
6.1 + 0.3
5.5 + 0.9
7 (29.2)
5 (50.0)
7.2 + 0.4
6.4 + 1.2
Riata 1582
Single
21 (10.7)
6 (28.6)
5.3 + 1.3
9 (64.3)
6.0 + 1.6
7 Fr Riata ST leads
Riata ST 7000
Dual
28 (14.2)
3 (10.7)
4.6 + 0.8
4 (21.1)
5.5 + 1.1
Riata ST 7001
Dual
12 (6.1)
2 (16.7)
3.7 + 1.7
2 (25.0)
4.7 + 2.0
Single
96 (48.7)
197
7 (7.3)
28 (14.2)
4.2 + 1.2
10 (14.3)
37 (18.8)
4.9 + 1.3
Riata ST 7002
Total
Fr, French; EX, externalization.
Downloaded from by guest on September 30, 2016
9 additional externalizations
5 additional electrical lead failures
All functional Riata leads were monitored with device interrogation
(clinical and remote monitoring) during a median follow-up of 5.8
years. In Table 4, the rates of electrical lead failure are analysed per
lead type. In cross-sectional analysis, 34 (17.3%) of the leads
showed signs of electrical lead failure which resulted in an incidence
rate of 2.97%/patient/year and a significant correlation of dwell time
(Spearman’s correlation 0.99, P , 0.001, Figure 3). None of the baseline characteristics were significantly different between patients with
or without electrical lead failure. Of the 34 patients with electrical
lead failure, 8 (23.5%) had detection of lead noise, 18 (52.9%) had abnormal pace/sense impedance changes, 8 (23.5%) abnormal shock
impedance changes, 6 (17.6%) alteration in pacing threshold, and
1 (2.9%) patient had a drop in R-wave amplitude without dislocation
(Figure 4). Eight patients had more than one feature of electrical lead
failure. In the univariate and multivariate Cox regression analysis, only
7 Fr Riata lead (HR 3.89; 95% CI: 1.561 –9.708; P ¼ 0.004) was an independent predictor of electrical lead failure. Prospectively, between
2012 and 2013, 5 of the 107 functional Riata leads developed electrical lead failure which resulted in an incidence rate of 4.67%/year.
Overall 4 of 197 (2.0%) patients had inappropriate shocks due to
oversensing of non-physiological noise on the ventricular sensing
channel. None of these patients showed signs of externalization
and inappropriate shocks were not correlated to externalization
(Phi’s coefficient 20.07, P ¼ 0.33). All of the patients with inappropriate shocks showed electrical lead failure, with a significant correlation between electrical dysfunction and inappropriate shocks
(Phi’s coefficient 0.31, P , 0.001).
1791
Mechanical and electrical dysfunction of Riata leads
Table 2 Clinical characteristics for externalization and electrical lead failure
EX 2013
N 5 37 (18.8%)
No-EX 2013
N 5 160 (81.2%)
Male
27 (16.4)
138 (83.6)
Female
Mean age + SD (years)
10 (31.2)
71.4 + 8.4
24 (68.8)
70.6 + 10.1
21 (34.4)
16 (11.8)
40 (65.6)
120 (88.2)
32 (18.6)
5 (20.8)
3 (10.3)
11 (11.8)
P-value
ED 2013
N 5 34 (17.3%)
No-ED 2013
N 5 161 (82.7%)
P-value
...............................................................................................................................................................................
Gender
0.05
29 (17.6)
136 (82.4)
0.79
0.62
5 (15.6)
70.7 + 10.3
27 (84.4)
70.8 + 9.7
0.98
,0.001
10 (16.4)
24 (17.6)
51 (83.6)
112 (82.5)
0.83
140 (81.4)
19 (79.2)
0.79
30 (17.4)
4 (16.7)
142 (82.6)
20 (83.3)
0.93
26 (89.7)
82 (88.2)
0.003
6 (20.7)
15 (16.1)
23 (79.3)
78 (83.9)
0.85
Lead type
8 Fr
7 Fr
ICD indication
Primary
Secondary
Type ICD
1 Chamber
2 Chamber
Biventricular
LVEF + SD (%)
Type CMP
ICMP
23 (31.1)
51 (68.9)
13 (17.6)
61 (82.4)
25.7 + 8.5
28.9 + 9.0
0.05
28.2 + 6.2
28.4 + 9.4
0.91
,0.001
22 (17.6)
103 (82.4)
0.90
12 (16.9)
59 (83.5)
114 (91.2)
26 (36.6)
45 (63.4)
Subclavian
33 (18.6)
144 (81.4)
Cephalic
ICD pocket side
4 (26.7)
11 (73.3)
Left
Right
Type of pocket
35 (19.3)
146 (80.7)
2 (15.4)
11 (84.6)
Subcutaneous
33 (25.8)
95 (74.2)
Subpectoral
3 (8.1)
34 (91.9)
0.45
0.73
0.02
33 (18.6)
144 (81.4)
1 (6.7)
14 (93.3)
31 (17.1)
150 (82.9)
3 (23.1)
10 (76.9)
23 (18.0)
105 (82.0)
9 (24.3)
28 (75.7)
0.24
0.59
0.39
EX, externalization; CMP, cardiomyopathy; ICMP, ischaemic cardiomyopathy; DCMP, dilated cardiomyopathy; HCMP, hypertrophic cardiomyopathy; VF, ventricular fibrillation;
VT, ventricular tachycardia.
Table 3 Univariate and multivariate Cox regression analysis for externalization
Univariate HR
95% CI
P-value
Age (years)
0.99
0.97–1.04
0.962
Female gender
8 Fr
2.63
1.01
1.26–5.47
0.50–2.06
0.01
0.972
Primary indication
0.96
0.37–2.48
Non-ICMP
2/3-chamber device
5.35
1.39
2.63–10.87
0.43–4.54
Multivariate HR
95% CI
P-value
2.00
0.95– 4.20
0.07
6.33
3.07– 13.03
,0.001
0.94
0.91– 0.98
0.02
...............................................................................................................................................................................
0.935
,0.001
0.585
Left-sided pocket
1.08
0.26–4.51
0.916
Subcutaneous pocket
Subcutaneous entrance
2.59
2.08
0.79–8.51
0.73–5.91
0.115
0.169
LVEF (%)
0.95
0.91–0.99
0.018
EX, externalization; CMP, cardiomyopathy; ICMP, ischaemic cardiomyopathy; DCMP, dilated cardiomyopathy; HCMP, hypertrophic cardiomyopathy; VF, ventricular fibrillation;
VT, ventricular tachycardia.
Downloaded from by guest on September 30, 2016
11 (8.8)
Non-ICMP
Venous entrance
1792
F. Demirel et al.
Table 4 Rates of electrical lead failure and adverse
events
Model
Coils
N (%)
ED (% within
lead model)
N=7
(24%)
AD (%
within
lead
model)
N = 17
(59%)
................................................................................
N=2
(7%)
8 Fr Riata leads
Riata 1580
Dual
28 (14.2)
5 (17.9)
1 (3.6)
Riata 1581
Dual
12 (6.1)
0 (0.0)
0 (0.0)
21 (10.7)
5 (23.8)
1 (4.8)
Riata 1582
Single
7 Fr Riata ST leads
Riata ST 7000
Dual
28 (14.2)
8 (28.6)
1 (3.6)
Riata ST 7001
Riata ST 7002
Dual
Single
12 (6.1)
96 (48.7)
2 (16.7)
14 (14.6)
0 (0.0)
1 (1.0)
197
34 (17.3)
4 (2.0)
Total
impedance alteration
impedance alteration &
threshold alteration
N=3
(10%)
threshold alteration
noise/oversensing
Figure 4 Rates of different forms of electrical lead dysfunction.
Ten patients had decreased impedance; nine patients had increased
impedance, and one patient with varying impedance.
Fr, French; ED, electrical dysfunction; AD, adverse events.
Cumulative electrical lead failure (%)
20.00
Spearman’s rho 0.99, P<0.001
15.00
10.00
5.00
0
0
20
40
60
80
Time after implantation (months)
B
100
Time
0
20
40
60
80
100
N remaining cases
147
145
143
125
27
0
N cumulative events
0
2
4
10
27
34
Figure 3 (A) Cumulative incidence of externalization which rises
linearly between 47 and 80 months (10–90th percentile) of followup. (B) Cumulative incidence of electrical dysfunction which rises linearly between 47 and 90 months (10–90th percentile) of follow-up.
Association of externalization
and electrical lead failure
Only 6 (16.2%) of the 37 externalized leads had electrical lead failure,
whereas 28 (17.5%) of the 160 non-externalized leads had electrical
lead failure (Fischer’s exact test P ¼ 1.00). Structural and electrical
lead failure co-existed only in six patients (3.0% of the population),
and did not correlate (Phi’s coefficient 20.013, P ¼ 0.85).
Discussion
In this study, we found that (i) there is a significant increase in electrical dysfunction and externalization rates, with prospective incidence
Construction and mechanism of failure
of the Riata lead
Riata leads have a silicone insulation with a unique multilumen construction.17 The hollow multilumen design results in the fact that
movement of internal conductors can occur, which increases the
risk of externalization through the silicone insulation (e.g. ‘inside-out
abrasion’) or conductor fracture. The inner pace-sense conductor is
encased in polytetrafluoroethylene and the outer lumens contain
conductors covered with ethylene tetrafluoroethylene (ETFE). The
Riata lead contains, depending on the specific subtype, two to four
conductors that operate as reinforcement for the lead and are electrically non-functional.
Structural lead failure
In our current report, a significant proportion of the Riata leads had
signs of externalization, with a higher incidence rate in prospective
longitudinal analysis (6.72%/year), compared with the suggested
rate by cross-sectional analysis (3.35%/year).
Current available data by the manufacturer (St. Jude Medical)
and others reported comparable rates of externalization.1,10 – 13
However, the prevalence of externalization has been reported to
range from 10 to 33% when systematic fluoroscopy was performed.7,9
Several reports showed that fluoroscopy should be considered as
the golden standard for the diagnosis of externalization and both the
NHRA and the FDA recommend systematic fluoroscopy.16,18,19
Downloaded from by guest on September 30, 2016
rates higher than suggested by cross-sectional analysis. Furthermore,
the extent of externalization increased during follow-up. (ii) Based on
cross-sectional analysis externalization and electrical lead failure
were not related. Impaired LVEF and non-ischaemic cardiomyopathy
were independent predictors of lead externalization and the 7 Fr lead
was an independent predictor of electrical lead failure. These crosssectional data should, however, be interpreted with caution. For the
best of our knowledge, this is the first study with both cross-sectional
and longitudinal analysis of both externalization and electrical lead
failure.
A
1793
Mechanical and electrical dysfunction of Riata leads
Electrical lead failure
Riata leads showed high electrical failure rates, with prospective
longitudinal incidence numbers higher (4.67%/year) than the linearly
increasing rates suggested by cross-sectional analysis (2.97%/year).
In previous studies, although the definition of failure has varied significantly, the rates of electrical lead failure ranged from ,1 to 57%.
The most common form of electrical dysfunction was alteration in
impedance, of which approximately half was abnormally low impedance, which can be caused by insulation abrasion. Other reports concluded that noise/oversensing was the main cause of electrical
dysfunction.7,11,15
It should be stated that most of the groups investigated the association between electrical and structural lead failure, only few groups
investigated the relationship with other factors.7,24,25 Cheungh
et al.24 showed that female gender and younger age as independent
predictors for electrical lead failure and showed a linear increase of
electrical lead failure. Parkash et al. found a higher rate of electrical
failure in 8 Fr Riata leads. In our report, 7 Fr lead was the only independent predictor for electrical lead failure.
While controversy exists regarding the association between
electrical and structural failures of the Riata lead, it is still unclear
if externalization without electrical lead failure could be dangerous.8,9,11 Several reports have investigated the association of electrical lead failure with externalization in detail, which is the most
important question in assessing the exact meaning and consequences of externalization.7 – 13,15,24,25 Longitudinal follow-up of
patients with externalization without electrical dysfunction seems
essential to answer this question. Liu et al.26 partially assessed this
issue, by analysing electrical failure rates in the externalized leads,
which was as high as 6.4% per year. Therefore, frequent electrical
follow-up and where possible, home-monitoring, is mandatory in
patients with externalization.
We observed that only in a small proportion of patients with lead
externalization (16.2%), electrical lead failure is present. Furthermore, we found no association of electrical lead failure with externalization. Our report is in line with previously published studies and the
multicentre, prospective Riata Lead Evaluation study.4,8,9,13,23 In controversy, the national registry of the Netherlands Heart Rhythm
Association found a significantly higher rate of electrical abnormalities in externalized leads than in non-externalized leads.10 Parvathaneni et al.7 did not see significant differences, but concluded that
‘serious’ electrical dysfunctions (noise, high threshold, lead fracture,
high voltage short) were more likely to be present in leads with externalization. Conductor externalization without electrical dysfunction
could be due to externalization of electrically non-functional conductors which are present in Riata leads or due to the intact ETFE coating
of functional conductors which could have prohibited electrical abnormalities. It is not known whether the ETFE coating in externalized
conductors can withstand high-voltage shocks, when low-voltage
tests are normal.9
Adverse events due to Riata leads are rare, but we found a significant association with electrical lead failure and no association with
externalization that is in line with previous studies.7,10,11 Previous
studies found an accelerating or a linear increase of lead failure
over time. In our analysis, we identified a higher incidence rate in
the prospective analysis compared with the cross-sectional analysis,
emphasizing the need for prospective data regarding this topic. This
pattern of lead failure is also seen for Sprint Fidelis leads.27 It is likely
that this pattern may be representative for most of the ICD leads and
most leads require a minimum of dwell time before the failures occur.
Limitations
The partly cross-sectional design of the study could prohibit us to
draw definite conclusions regarding the exact time of externalization
and time dependency of lead failure, therefore the cross-sectional
data should be interpreted cautiously. The longitudinal phases of
the study provide additional insight on the time course of externalization and electrical failure. However, even in the longitudinal phase the
exact time of externalization remains uncertain. Furthermore, like in
most of the present reports, we did not have any information regarding deceased patients.
Clinical implications
This study demonstrates high rates of structural and electrical failure
of the Riata lead. Despite the high rates, there was no relation
between structural and electrical failure. Inconsistency exists about
Downloaded from by guest on September 30, 2016
All studies are in line with the fact that externalization rates
increase over time. In our follow-up, all functional and non-functional
Riata leads were screened by fluoroscopy and seemed to show a significant correlation with dwell time. These results should be interpreted cautiously, since the exact time of externalization is
unknown. However, this accounts for both prospective and crosssectional analysis, as also in the prospective study the exact time
point of externalization remains unknown. We performed univariate
and multivariate Cox regression analysis to determine predictors for
externalization. Although we realize that this has limitations for
retrospective data, of which partially the exact incidence dates are
unclear, we believe that the analysis provides additive information
and is hypothesis generating. These results remain to be confirmed
in prospective analysis.
Externalization is common; however, the amount of externalization seems to be very modest (virtually all ,2 cm).7 In our report
we see small extents of externalization, except for one patient
with extreme externalization without electrical dysfunction.20 Interestingly, a significant increase in the extent of externalization is seen
during follow-up of both functional and non-functional Riata leads.
This supports the current recommendation to perform serial followup with device interrogation and fluoroscopy in patients with a functional Riata lead and also in patients with non-functional Riata leads
that were not extracted.
Factors that have been associated with externalization in previous
analyses are time since implantation, non-ischaemic cardiomyopathy,
multiple leads, a higher percentage of RV pacing, lower LVEF, single
coil leads, 8 Fr leads, lower age, apical lead position, and hypertrophic
cardiomyopathy.7,9 – 11,21 – 23 In our present univariate and multivariate analysis, also non-ischaemic cardiomyopathy and impaired LVEF
were associated with externalization. 8 Fr was not an independent
predictor of externalization, while most of the large studies
showed a significant association.10,11,22 This could be due to the
larger amount (69%) of 7 Fr leads in our analysis compared with
the large multicentre studies 53% (Theuns et al.), 33.4% (Hayes
et al.), and 28.2% (Steinberg et al.), respectively.10,11,23
1794
the relationship between structural and electrical failure and routine
fluoroscopic screening. How to handle leads with electrical dysfunction is clear. However, the key question is how to handle the leads
that have externalized conductors without electrical dysfunction?
Because of lack of correlation between structural and electrical
failure, an appropriate individualized management should be taken
for each patient by considering the risk of revision and or
extraction vs. the risk of careful follow-up.
Conclusion
Riata leads show progressive and high rates of electrical and structural
failure with progressive extent of externalization during follow-up.
Based on the cross-sectional analysis, there was no association
between externalization and electrical lead failure. Furthermore,
we identified impaired LVEF and non-ischaemic cardiomyopathy as
independent predictors for externalization and 7 Fr leads for electrical lead failure in the cross-sectional analysis.
Acknowledgement
The authors thank Vera Derks for her skillful secretarial assistance.
Conflict of interest: none declared.
1. Carlson M, Tsung P. Medical device advisory. Sylmar, CA: St Jude Medical; 2011.
2. Kleemann T, Becker T, Doenges K, Vater M, Senges J, Schneider S et al. Annual rate of
transvenous defibrillation lead defects in implantable cardioverter-defibrillators
over a period of .10 years. Circulation 2007;115:2474 –80.
3. Hauser RG, McGriff D, Retel LK. Riata implantable cardioverter-defibrillator lead
failure: analysis of explanted leads with a unique insulation defect. Heart Rhythm
2012;9:742 –9.
4. Erkapic D, Duray GZ, Bauernfeind T, De Rosa S, Hohnloser SH. Insulation defects of
thin high-voltage ICD leads: an underestimated problem? J Cardiovasc Electrophysiol
2011;22:1018 – 22.
5. Kodoth VN, Hodkinson EC, Noad RL, Ashfield KP, Cromie NA, McEneaney DJ
et al. Fluoroscopic and electrical assessment of a series of defibrillation leads:
prevalence of externalized conductors. Pacing Clin Electrophysiol 2012;35:
1498 – 504.
6. Liu J, Rattan R, Adelstein E, Barrington W, Bazaz R, Brode S et al. Fluoroscopic
screening of asymptomatic patients implanted with the recalled Riata lead family.
Circ Arrhythm Electrophysiol 2012;5:809 –14.
7. Parvathaneni SV, Ellis CR, Rottman JN. High prevalence of insulation failure
with externalized cables in St. Jude Medical Riata family ICD leads: fluoroscopic grading scale and correlation to extracted leads. Heart Rhythm 2012;
9:1218 – 24.
8. Schmutz M, Delacretaz E, Schwick N, Roten L, Fuhrer J, Boesch C et al. Prevalence of
asymptomatic and electrically undetectable intracardiac inside-out abrasion in
silicon-coated Riata(R) and Riata(R) ST implantable cardioverter-defibrillator
leads. Int J Cardiol 2013;167:264–257.
9. Shen S, Bhave P, Giedrimas E, Patel T, Arora R, Chicos AB et al. Prevalence and
predictors of cable extrusion and loss of electrical integrity with the Riata defibrillator lead. J Cardiovasc Electrophysiol 2012;23:1207 –12.
10. Theuns DA, Elvan A, de Voogt W, de Cock CC, van Erven L, Meine M. Prevalence
and presentation of externalized conductors and electrical abnormalities in Riata
defibrillator leads after fluoroscopic screening: report from the Netherlands heart
rhythm association device advisory committee. Circulation Arrhythm Electrophysiol
2012;5:1059 –63.
11. Steinberg C, Sarrazin JF, Philippon F, Bouchard MA, O’Hara G, Molin F et al. Detection of high incidence of Riata lead breaches by systematic postero-anterior and
lateral chest X-ray in a large cohort. Europace 2013;15:402 –8.
12. Larsen JM, Riahi S, Nielsen JC, Videbaek R, Haarbo J, Due KM et al. Nationwide
fluoroscopic screening of recalled Riata defibrillator leads in Denmark. Heart
Rhythm 2013;10:821 –7.
13. Hauser RG, Abdelhadi RH, McGriff DM, Kallinen Retel L. Failure of a novel
silicone-polyurethane copolymer (OptimTM ) to prevent implantable cardioverterdefibrillator lead insulation abrasions. Europace 2013;15:278 –83.
14. Sung RK, Massie BM, Varosy PD, Moore H, Rumsfeld J, Lee BK et al. Long-term
electrical survival analysis of Riata and Riata ST silicone leads: National Veterans
Affairs experience. Heart Rhythm 2012;9:1954 –61.
15. Abdelhadi RH, Saba SF, Ellis CR, Mason PK, Kramer DB, Friedman PA et al. Independent multicenter study of Riata and Riata ST implantable cardioverter-defibrillator
leads. Heart Rhythm 2013;10:361 –5.
16. Inspectie voor de Gezondheidszorg - Patiënten met ICD-lead merk St. Jude
Medical type Riata opgeroepen voor controle. http://www.igz.nl/actueel/nieuws/
patintenmeticdleadmerkstjudemedicaltyperiataopgeroepenvoorcontrole.aspx.
17. Epstein AE, Baker JH, Beau SL, Deering TF, Greenberg SM, Goldman DS.
Performance of the St. Jude Medical Riata leads. Heart Rhythm 2009;6:204 – 9.
18. Safety Communications . FDA Safety Communication: Premature Insulation
Failure in Recalled Riata Implantable Cardioverter Defibrillator (ICD) Leads
Manufactured by St. Jude Medical, Inc. http://www.fda.gov/MedicalDevices/Safety/
AlertsandNotices/ucm314930.htm.
19. Lorvidhaya P, Mendoza I, Sehli S, Atalay MK, Kim MH. Prospective evaluation of
cinefluoroscopy and chest radiography for Riata lead defects: implications for
future lead screening. J Interv Card Electrophysiol 2013;38:131 – 5.
20. Demirel F, Adiyaman A, Delnoy PP, Elvan A. Extreme externalization of Riata intracardiac cardioverter defibrillator leads: a new peril of a troublesome lead. J Cardiovasc
Electrophysiol 2014;25:216.
21. Moorman LP, Moorman JR, Dimarco JP, Malhotra R, Darby A, Bilchick K et al. Increasing lead burden correlates with externalized cables during systematic fluoroscopic
screening of Riata leads. J Interv Card Electrophysiol 2013;37:63–8.
22. Valk SD, Theuns DA, Jordaens L. Long-term performance of the St Jude Riata
1580 –1582 ICD lead family. Neth Heart J 2013;21:127 –34.
23. Hayes D, Freedman R, Curtis AB, Niebauer M, Neal Kay G, Dinerman J et al.
Prevalence of externalized conductors in Riata and Riata ST silicone leads: results
from the prospective, multicenter Riata Lead Evaluation Study. Heart Rhythm
2013;12:1778 –82.
24. Cheung JW, Al-Kazaz M, Thomas G, Liu CF, Ip JE, Bender SR et al. Mechanisms,
predictors, and trends of electrical failure of Riata leads. Heart Rhythm 2013;10:1453–9.
25. Parkash R, Exner D, Champagne J, Mangat I, Thibault B, Healey JS et al. Failure rate of
the Riata lead under advisory: a report from the CHRS Device Committee. Heart
Rhythm 2013;10:692 –5.
26. Liu J, Qin D, Rattan R, Bazaz R, Adelstein E, Jain S et al. Longitudinal follow-up of
externalized Riata leads. Am J Cardiol 2013;10:1616 –8.
27. Cheung JW, Tobin-Hess A, Patel A, Slotwiner DJ, Goldner BG. Trends in Fidelis lead
survival: transition from an exponential to linear pattern of lead failure over time.
Circ Arrhythm Electrophysiol 2012;5:906 –12.
Downloaded from by guest on September 30, 2016
References
F. Demirel et al.