Hospice Fraud Takes Advantage of People at the End of Life
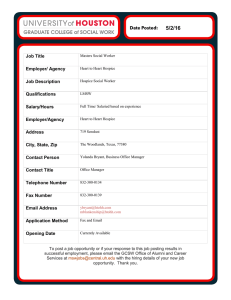
advertisement

The Sentinel, a publication of the SMP Resource Center www.smpresource.org November 2014 Hospice Fraud Takes Advantage of People at the End of Life By Nancy Aldrich and Jolie Crowder Health Benefits ABCs A woman in her 90s moved into an assisted living facility (ALF) in early March. A few weeks later the ALF told the new resident’s daughter that her mother might be a good candidate for hospice. The daughter was surprised because her mother’s doctor had not said she was near the end of life and she was only admitted to the ALF for help with her daily care. The assisted living director told the daughter that going on hospice does not mean that an individual is terminal and her mother would get more care at no cost. Meeting with a hospice representative, the daughter was told her mother could get a new wheelchair, walker, bed, commode, and padded floor mats, even though the daughter said her mother’s current wheelchair and walker were just fine. Hospice ordered the new equipment anyway. The hospice also ordered a breathing machine – something the mother had never needed before – and medication to ease a recurring backache. The daughter said her mother became overmedicated. She requested the medicine be stopped, but hospice continued the medicine. Her mother became unable to leave the room and died in mid-April. The Texas SMP referred this allegation to the U.S. Department of Health and Human Services Office of Inspector General (OIG). Can you identify possible fraud in the case highlighted above? Two red flags are: The hospice benefit does not appear to have been offered to a beneficiary who had been certified by a physician to be terminally ill with a life expectancy of six months or less. The hospice provider appears to have ordered redundant and/or unnecessary equipment and medication. According to the OIG, other common areas of hospice fraud include: Paying incentives to referral sources (such as physicians and nursing homes) Billing for a higher level of care than was actually provided Failing to obtain physician certification on plans of care Falsifying records to fake eligibility or physician certification High-pressure marketing of hospice services to ineligible beneficiaries Providing inadequate or incomplete services “The decision to provide hospice services should be prompted by a patient’s terminally ill medical condition and desire for palliative care, not a hospice provider’s desire to boost its profits,” said OIG Special Agent in Charge Gerald T. Roy. continued Did You Know? Regulating bodies are working to improve hospice care and reduce waste and fraud. 1. Effective Oct. 1, 2014, new Medicare Conditions of Participation gave hospice patients more rights, including the right to choose their own attending physician instead of a doctor provided by the hospice. 2. Signed into law Oct. 6, 2014, The Improving Medicare Post-Acute Care Transformation Act of 2014 (IMPACT Act) requires hospice surveys to be conducted every three years. Currently inspections are sporadic and might take place once every six to eight years, due to budget constraints. The new law also authorizes more funds to do surveys. Understanding the Medicare Hospice Benefit Medicare makes generous hospice payments to cover much-needed family support, necessary services, medications, and durable medical equipment for terminally ill patients. But the system is ripe for fraud. The Medicare hospice benefit is designed for Part A beneficiaries who have been diagnosed as terminally ill, meaning the patient is expected to live six months or less if the illness runs its normal course. Hospice covers palliative and support services including personal care, medical equipment, therapy, and other services. Beneficiaries are entitled to receive hospice care for two 90-day periods, followed by an unlimited number of 60day periods. The periods need not be consecutive. At the start of each period of care, an attending physician must certify that the beneficiary is terminally ill and has a life expectancy of six months or less. For care to be covered under Part A, hospices must be certified by Medicare. The Medicare hospice benefit has four levels of care, each with an all-inclusive daily rate paid through Part A. The rate is paid to the hospice for each day that a beneficiary is in hospice care, regardless of the number of services furnished. Rates are adjusted geographically. About 96 percent of hospice care is considered “Routine Home Care,” where the patient receives hospice care at his/her residence. The three other levels of hospice care are: 1) Continuous Home Care, furnished during brief periods of crisis to maintain the terminally ill patient at home; 2) General Inpatient Care, providing pain control or acute/complex symptom management in an inpatient facility; and 3) Inpatient Respite Care at an approved facility on a short-term basis as respite for the family caregiver. Medicare Spent Almost $15 Billion on Hospice Care in 2012 There’s a lot of money at stake. In 2011, there were 3,585 Medicare-certified hospices, according to a May 3, 2013, OIG memorandum. Of these, 2,071 were for-profit, 1,237 were nonprofit, and 185 were government-owned. In an Aug. 29, 2013, memorandum, the OIG also said the number of Medicare facilities increased by 43 percent from 2005 to 2011, and Medicare paid the bill for 84 percent of all hospice services provided nationally. There were 1.2 million Medicare beneficiaries receiving hospice care in 2011. Medicare expenditures for the hospice benefit have increased from $10.1 billion in 2007 to an estimated $14.9 billion in 2012, according to the Centers for Medicare & Medicaid Services (CMS). CMS said the growth in expenditures reflects many factors, including more beneficiaries utilizing the benefit, beneficiaries utilizing the benefit for longer lengths of time, and increases in the base payment rate for hospice services. Role for SMPs SMPs interviewed for this story said they don’t get many hospice fraud cases. This is probably because the fraud is hard to identify and it is a difficult time for a grieving family to review MSNs, let alone identify fraud. Hospice and end-of-life care is a topic fraught with emotion. Barbara McGinity, LMSW, program director of the Texas SMP, explains that beneficiaries and their families are told that Medicare will pay for hospice regardless of whether it’s true or the care is inappropriate. “You’re in the situation where you don’t know what to do, and so you continued are really relying on the professionals to tell you things that are correct. How do you differentiate what is appropriate and not appropriate?” she said. McGinity said her SMP developed a fact sheet to help beneficiaries understand hospice fraud. SMP Resource Library users can find it by doing an advanced search and selecting “Texas” for origin and “fact sheets” for type. In one SMP case, a senior building’s social service coordinator referred a Medicare beneficiary for hospice because of a diagnosis of a low hemoglobin level (anemia). After the patient’s death, the family received an MSN that showed several claims for nurse and aide services. The beneficiary’s daughter contacted the SMP and questioned the need for a hospice service that was providing breakfast each day and a bath once a week. The daughter claimed the beneficiary was, in fact, able to do those tasks, according to Jason Echols, SMP-Health Care Consumer Protection Coordinator with AgeOptions in Oak Park, IL. In another case cited by Echols, a Medicare hospice patient’s family called to complain that a catatonic patient was being force fed peanut butter and jelly sandwiches despite a living will stating that she did not want to be fed if she could not feed herself. The family felt the hospice was keeping her alive so it could continue to bill Medicare (the patient had a terminal illness for nine years). The hospice also billed Medicare for a wheelchair that the beneficiary previously purchased directly from a nursing home. Both of these cases were referred by the SMP to the proper authorities, Echols said. SMPs are in a unique position to provide help and information to families and patients at a difficult time. Reviewing health care bills and MSNs usually isn’t a priority as a loved one faces the end of life. When families wade through the piles of paperwork, SMPs can serve as a valuable resource in explaining what’s legitimate and what’s not. “Hospice care plays a critical role in our health care system, providing for end-of-life care as opposed to curative life care,” according to U.S. Attorney John Walsh for the District of Colorado. “When companies systematically overbill Medicare by keeping people in hospice when they don’t need to be there, it jeopardizes this important benefit for others under the program. We will not tolerate such conduct.” Resources Hospice Center website Medicare.gov Booklet: Medicare Hospice Benefits Hospice Payment System: Payment System Fact Sheet Series National Hospice and Palliative Care Organization NHPCO Booklet: Facts and Figures: Hospice Care in America continued Cases Below are examples of hospice fraud cases reported in recent months by the U.S. Department of Justice. As you can see, fraud occurs in a variety of venues: hospice facilities; home hospice businesses; and entities that provide hospice care for residents of nursing homes, assisted living facilities, hospitals, and private homes. Colorado. The Department of Justice has partially intervened against defendants in two whistleblower lawsuits in U.S. District Court for the District of Colorado. It reported Aug. 28, 2014, that the lawsuits allege that Evercare Hospice and Palliative Care (now known as Optum Palliative and Hospice Care) submitted false claims for the Medicare hospice benefit. The lawsuits, filed by former Evercare employees, allege that defendants violated the False Claims Act by knowingly submitting false claims for hospice benefits for patients who did not have a life expectancy of six months or less. The complaints include allegations that management pressured employees and physicians to admit and retain patients who were not terminally ill and challenged or disregarded physicians’ decisions that patients should be discharged. Illinois. An owner and three former employees of an Illinois hospice company, Passages Hospice, LLC , as well as the company itself, were indicted on federal health care fraud charges for allegedly engaging in an extensive scheme to obtain higher Medicare and Medicaid payments by fraudulently elevating the level of hospice care for patients, the U.S. Attorney, Northern District of Illinois, reported May 27, 2014. In many instances, the level of hospice care allegedly exceeded what was medically necessary or actually provided, including for some patients who did not have terminal illnesses or who were enrolled far longer than the required life expectancy of six months or less. Pennsylvania. U.S. Attorney Zane David Memeger reported on May 27, 2014, that Matthew Kolodesh of Churchville, PA, was sentenced to more than 14 years in prison and ordered to pay $16.2 million in restitution to Medicare and $16.2 million in forfeiture money for a scheme to defraud Medicare through his home hospice business. From 2003 to 2008, Kolodesh’s business, Home Care Hospice Inc. (HCH), submitted false claims to Medicare totaling approximately $16.2 million for patients that were not eligible for hospice services and for patients that never received the level of hospice services billed by HCH. Oklahoma. A federal grand jury in Oklahoma City returned an indictment charging two individuals and Prairie View Hospice Inc. of Chandler, OK, with 39 counts relating to Medicare fraud, announced Sanford C. Coats, United States Attorney for the Western District of Oklahoma, on April 17, 2014. The indictment alleges that from July 2010 through July 2013, the defendants conspired to conceal the true medical condition of Prairie View Hospice’s patients and the true quality and quantity of health care services they were receiving in order to “pass” a Medicare audit and to fraudulently obtain money from Medicare. The indictment alleges that certain medical documents were falsified to make it appear that nurses had visited patients or conducted necessary assessments when such visits and assessments had not, in fact, been made. Also, nursing notes were falsified to make it appear that patients were in worse health than they actually were in order to justify to Medicare the patient’s continued hospice care. This newsletter was supported in part by a grant (No. 90NP0003) from the Administration for Community Living (ACL), U.S. Department of Health and Human Services (DHHS). Grantees carrying out projects under government sponsorship are encouraged to express freely their findings and conclusions. Therefore, points of view or opinions do not necessarily represent official ACL or DHHS policy.