From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
LYMPHOID NEOPLASIA
Deep-sequencing approach for minimal residual disease detection in acute
lymphoblastic leukemia
Malek Faham,1 Jianbiao Zheng,1 Martin Moorhead,1 Victoria E. H. Carlton,1 Patricia Stow,2 Elaine Coustan-Smith,3
Ching-Hon Pui,2 and Dario Campana3
1Sequenta Inc, South San Francisco, CA; 2Department of Oncology, St Jude Children’s Research Hospital, Memphis, TN; and 3Department of Pediatrics,
National University of Singapore, Singapore
The persistence of minimal residual disease (MRD) during therapy is the strongest adverse prognostic factor in acute
lymphoblastic leukemia (ALL). We developed a high-throughput sequencing
method that universally amplifies antigenreceptor gene segments and identifies all
clonal gene rearrangements (ie, leukemiaspecific sequences) at diagnosis, allowing monitoring of disease progression
and clonal evolution during therapy. In
the present study, the assay specifically
detected 1 leukemic cell among greater
than 1 million leukocytes in spike-in experiments. We compared this method with
the gold-standard MRD assays multiparameter flow cytometry and allele-specific
oligonucleotide polymerase chain reaction (ASO-PCR) using diagnostic and
follow-up samples from 106 patients with
ALL. Sequencing detected MRD in all
28 samples shown to be positive by flow
cytometry and in 35 of the 36 shown to
be positive by ASO-PCR and revealed
MRD in 10 and 3 additional samples that
were negative by flow cytometry and
ASO-PCR, respectively. We conclude that
this new method allows monitoring of
treatment response in ALL and other lymphoid malignancies with great sensitivity
and precision. The www.clinicaltrials.gov
identifier number for the Total XV study
is NCT00137111. (Blood. 2012;120(26):
5173-5180)
Introduction
The clinical management of patients with acute lymphoblastic
leukemia (ALL) relies on accurate prediction of relapse hazard to
determine the intensity of therapy and to avoid over- or undertreatment.1,2 Traditional prognostic factors include presenting clinical
and biologic features such as age, blast count at diagnosis,
immunophenotype, and genetic abnormalities.1,2 Based on a large
body of evidence involving thousands of patients, the measurement
of residual leukemia levels, “minimal residual disease” (MRD),
during therapy has now emerged as the most important predictor
of outcome in ALL.3,4 As a result, risk-classifications based on
MRD assessment are now a critical component of ALL clinical
treatment protocols.
Current methodologies to monitor MRD in ALL include flow
cytometric detection of aberrant immunophenotypes, which can
detect 1 leukemic cell among 10 000 (0.01%) normal cells, and
allele-specific oligonucleotide PCR (ASO-PCR) amplification of
immunoglobulin (Ig) and T-cell receptor (TCR) genes, which has a
sensitivity of 0.001%.3-5 Although these methods have proven to be
reliable in a clinical setting, they have limitations. Flow cytometry
requires a high level of expertise to interpret results proficiently.
ASO-PCR requires the development of reagents and assay conditions for each individual patient, which is laborious and timeconsuming. Moreover, these methods have limited or no capacity
to monitor the evolution of different leukemic subclones during
treatment, with the potential of false-negative results. Finally,
patients who achieve MRD⫺ status by standard criteria but have
very low levels of persistent leukemia have a higher risk of relapse
than those with no detectable MRD,6 suggesting that improvements
in sensitivity of MRD monitoring methods might improve precision in predicting relapse.
We developed a novel, sequencing-based method to identify
cells with specific molecular signatures. The method employs
consensus primers to universally amplify rearranged Ig and TCR
gene segments in a sample and relies on high-throughput sequencing and specifically designed algorithms to identify clonal gene
rearrangements in diagnostic samples and quantify these rearrangements in follow-up MRD samples. In the present study, we
assessed the suitability of this method to monitor MRD in ALL. We
determined its sensitivity and specificity, delineated the extent of
genetic diversity (including clonal evolution) present at diagnosis,
and compared its capacity to measure MRD with that of flow
cytometry and ASO-PCR in follow-up samples from more than
100 patients with ALL.
Submitted July 17, 2012; accepted September 29, 2012. Prepublished online
as Blood First Edition paper, October 16, 2012; DOI 10.1182/blood-2012-07444042.
The publication costs of this article were defrayed in part by page charge
payment. Therefore, and solely to indicate this fact, this article is hereby
marked ‘‘advertisement’’ in accordance with 18 USC section 1734.
The online version of this article contains a data supplement.
© 2012 by The American Society of Hematology
BLOOD, 20 DECEMBER 2012 䡠 VOLUME 120, NUMBER 26
Methods
Clinical samples
BM samples were collected at diagnosis and during treatment from
110 children with newly diagnosed B-lineage ALL, representing 22.1% of
the 498 patients enrolled in the Total XV study at St Jude Children’s
Research Hospital.7 The sample selection for this study was based on the
demonstrated presence of an immunoglobulin heavy chain locus (IGH@,
IgH) clonal rearrangement at diagnosis, ASO-PCR MRD data in a
follow-up sample, and abundant surplus DNA available. This study was
conducted in accordance with Declaration of Helsinki principles, was
5173
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
5174
BLOOD, 20 DECEMBER 2012 䡠 VOLUME 120, NUMBER 26
FAHAM et al
approved by the St Jude Institutional Review Board, and written informed
consent was obtained from the parents or guardians of each child (and
assent from the patients as appropriate).
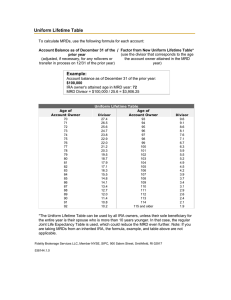
clones, we used the highest frequency index clone to calculate the
percentage of MRD in follow-up samples. This quantitation scheme is
illustrated schematically in Figure 1B.
MRD measurements by ASO-PCR and flow cytometry
Assessment of Sequenta LymphoSIGHT platform technical
performance
ASO-PCR MRD studies were performed as described previously, with
MRD quantification performed by limiting-dilution (n ⫽ 34) or real-time
PCR (n ⫽ 76). Briefly, we made 10-fold serial dilutions of diagnostic DNA
in pooled peripheral blood DNA extracted from mononuclear cells of
4-6 healthy donors and analyzed each dilution in duplicate (in quadruplicate
for the single-copy dilution). For the limiting dilution method, we used
either a 2-round (semi-nested or with the same patient-specific and
consensus primer in both rounds) or a 1-round PCR assay with an initial
touchdown phase and quantitated MRD using Poisson statistics. Real-time
PCR analysis was performed by a single PCR amplification with sequencespecific TaqMan hydrolysis probes on an ABI PRISM Sequence Detection
System 7700 (Applied Biosystems).6 MRD studies by flow cytometry were
performed using a combination of markers identified at diagnosis, as
described previously.8
Diagnostic samples from 12 ALL patients were used for technical assessment of the LymphoSIGHT platform. The selected samples had a
⬎ 95% clonal rearrangement frequency among B-lineage cells. In addition,
the samples were almost exclusively composed of leukemic B-lineage cells
based on equivalence between the total number of rearranged IgH
molecules and leukocytes in each sample.
Serial dilutions of the 12 selected samples were prepared in duplicate in
normal PBMCs at a range between 1 in 1 million and 1 in 1000 cells.
Dilutions were then subjected to amplification and sequencing in 2 replicate
experiments. Correction factors for sample purity and dilution preparations
were applied and RT-PCR based measurements of the sample concentration
were used for increased accuracy. We compared expected and measured
frequencies in log space. For correlation and slope, the lowest dilution was
excluded because some values were 0.
MRD measurements with the Sequenta LymphoSIGHT method
Genomic DNA, isolated using AllPrep DNA mini and/or micro kits
(QIAGEN), was amplified using locus-specific primer sets for IgH@ complete
(VHDJH), IgH@ incomplete (DJH), and TCRs including TRB@, TRD@, and
TRG@, which were designed to allow for the amplification of all known
alleles of the germline IgH and TCR sequences (for a description of the
primer design and amplification and sequencing reactions, see supplemental Methods, available on the Blood Web site; see the Supplemental
Materials link at the top of the online article).9 A clonotype was defined
when at least 2 identical sequencing reads were obtained (see supplemental
Methods).
The frequency of each clonotype in a sample was determined by
calculating the number of sequencing reads for each clonotype divided by
the total number of passed sequencing reads in the sample. To define
leukemic gene rearrangements in samples obtained at diagnosis, we used a
frequency threshold of 5% (ie, any clonotype present at a frequency
of ⬎ 5% was regarded as originating from the leukemic clone). In
preliminary studies, the frequency of individual clonotypes among normal
B-cell populations was consistently below this threshold.
We used the following criteria to identify any clonotypes present in the
same diagnostic sample that might have evolved from the leukemic clone
through VH replacement: (1) identical J and D segments, (2) identical
J segment deletion size, (3) identical D segment deletion size (the side next
to the J segment), (4) random N base insertions between the J and
D segments, and (5) different V segments.
The leukemia-derived sequences identified at diagnosis were used as a
target to assess the presence of MRD in follow-up samples. For MRD
quantitation, we generated multiple sequencing reads for each rearranged
B cell in the reaction. For example, in cells containing an IgH rearrangement (ie, B cells), the MRD assay was designed to achieve approximately
10⫻ coverage per B cell.
To determine the absolute measure of the total leukemia-derived
molecules present in the follow-up sample, we added a known quantity of
reference IgH sequence into the reaction and counted the associated
sequencing reads. The known quantity of reference IgH sequence was
derived from a pool of plasmids containing 3 unique IgH clonotypes
quantitated using standard RT-PCR methods. The resulting factor (ie, the
number of molecules per sequence read) was then applied to the leukemiaassociated clonal rearrangement reads to obtain an absolute measure of the
total leukemia-derived molecules in the reaction. A similar calculation can
be performed to assess the total number of rearranged IgH molecules or
B-lineage cells in the reaction. Finally, we calculated the total leukocytes in
the reaction by measuring the total DNA using standard PicoGreen methods
and RT-PCR using genomic markers such as -actin DNA.
These metrics were combined to calculate a final MRD measurement,
which is the number of leukemia-derived molecules divided by the total
leukocytes in the sample. In cases in which there were are multiple index
Results
Sensitivity, precision, and quantitative capacity of the immune
repertoire sequencing assay
Figure 1 provides an overview of the Sequenta LymphoSIGHT
method. Using universal primer sets, we first amplified IgH@ and
TCR sequences from genomic DNA in a 2-stage PCR. The
amplified product was sequenced to obtain a high number of reads
(eg, 106 reads; Figure 1A). Typically, the number of reads exceeded
the number of starting molecules, allowing every starting molecule
to be sampled. The sequence reads were analyzed to determine
similar sequences that form a clonotype. After clonotype determination, a standard quantitation scheme was used to calculate MRD
metrics (Figure 1B, “Methods”), including clonotype frequency,
number of leukemia-associated molecules in the reaction, number
of total leukocytes in the reaction, and MRD level.
We assessed the technical performance of the method using
diagnostic samples from 12 of the 110 ALL patients included in the
study who carried 13 leukemic IgH clonotypes. Serial dilutions of
leukemic cells in normal PBMCs, ranging from ⬍ 1 in 1 million
to ⬎ 1 in 1000 cells, were prepared and analyzed in duplicate. The
high precision of the assay was demonstrated by the low average
relative SDs (range, 4.1%-7.6%) at clonotype frequencies at or
above 3 ⫻ 10⫺5 (supplemental Table 1). Therefore, the assay is
highly quantitative for frequencies above 10⫺5. Random error
increased at clonotype frequencies below 10⫺5, as expected from
Poisson statistics with low number of input molecules in the
reaction (supplemental Table 1). For each clonotype, the assay
showed high r2 values with a range of 0.977 to 0.996 (mean
0.988 and median 0.991) between each of the expected and the
measured clonotype frequencies (Figure 2 and supplemental Table
2). The slopes ranged from 0.878 to 1.14 (mean 1.00 and median
0.977), illustrating the quantitative nature of the assay over at least
3 orders of magnitude.
The immune repertoire sequencing assay unequivocally detected leukemic signatures in all dilutions with expected concentration of at least 1 leukemic cell in 1 million leukocytes (a sensitivity
of 10⫺6; Figure 2). We also tested the sensitivity of the assay to
detect levels of leukemic cells below 1 in 1 million leukocytes
(Figure 2). We detected an average expected concentration of
7.4 ⫻ 10⫺7 and expected number of molecules of 5. We did not
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
BLOOD, 20 DECEMBER 2012 䡠 VOLUME 120, NUMBER 26
DEEP-SEQUENCING METHOD FOR MRD DETECTION
5175
Figure 1. Overview of the LymphoSIGHT method. (A) Schematic of the PCR primer strategy and sequencing assay. (B) Schematic of the MRD quantitation scheme.
detect leukemia signals in 2 cases with low expected concentrations (4.2 ⫻ 10⫺7 and 6.7 ⫻ 10⫺7 with 2 and 4 expected molecules,
respectively), a result that was likely caused by insufficient
leukemia-derived molecules in the reaction and is consistent with
Poisson sampling.
Analysis of all clonotypes together reflects multiple sources of
error, including error associated with quantitation of the original
leukemic DNA, pipetting error in the dilution preparations, error in
measurement of the original sample purity (ie, samples may not
have been composed of 100% leukemic B cells), and random and
systematic error associated with the assay. Despite these potential
sources of error, we measured an r2 value of 0.94 and a slope of
1.01 between the expected and measured clonotype frequencies.
Therefore, the cell dilution experiments clearly demonstrated the
immune repertoire sequencing assay to be precise and quantitative
with sensitivity levels at or below 1 leukemic cell per 1 million
leukocytes.
Detection of clonal rearrangements of multiple receptor genes
in diagnostic samples
We used the sequencing assay to detect rearrangements of immune
cell receptor genes, IgH@ complete (VHDJH), IgH@ incomplete
(DJH), TRB@, TRD@, and TRG@, in diagnostic BM samples from
100 of the 110 ALL patients known to have IgH rearrangements.
An additional 10 samples were only assayed for IgH VHDJH and
were not included in this clonal gene rearrangement analysis. As
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
5176
BLOOD, 20 DECEMBER 2012 䡠 VOLUME 120, NUMBER 26
FAHAM et al
10-2
10-2
A
C
10-3
10-3
10-4
10-4
10-4
10-5
10-5
10-5
10-6
10-6
10-6
10-7
10-7
10-7
10-6
10-5
10-4
10-3
10-2
10-2
10-7
10-6
10-5
10-4
10-3
10-2
10-2
D
10-7
10-7
10-3
10-4
10-4
10-4
10-5
10-5
10-5
10-6
10-6
10-6
10-7
10-7
10-7
10-7
10-5
10-4
10-3
10-2
10-6
10-5
10-4
10-3
10-2
10-2
G
10-7
10-7
H
10-3
10-4
10-4
10-4
10-5
10-5
10-5
10-6
10-6
10-6
10-7
10-7
10-7
10-7
10-4
10-3
10-2
10-2
10-6
10-5
10-4
10-3
10-2
10-2
J
10-7
10-7
10-3
10-4
10-4
10-4
10-5
10-5
10-5
10-6
10-6
10-6
10-7
10-7
10-5
10-4
10-3
10-2
10-6
10-5
10-4
10-3
10-2
10-6
10-5
10-4
10-3
10-2
10-6
10-5
10-4
10-3
10-2
L
10-3
10-6
10-2
10-2
K
10-3
10-7
10-3
I
10-3
10-5
10-4
10-2
10-3
10-6
10-5
F
10-3
10-6
10-6
10-2
E
10-3
10-2
Observed
frequency
10-2
B
10-3
10-7
10-6
10-5
10-4
10-3
10-2
10-7
10-7
Expected
frequency
Figure 2. Technical performance of immune repertoire sequencing assay. Diagnostic samples from 12 ALL patients containing 13 leukemic IgH clonotypes were used for
technical performance studies. Serial dilutions of leukemic cells in normal PBMCs, ranging from ⬍ 1 in 1 million to ⬎ 1 in 1000 tumor cells, were prepared and analyzed in
duplicate. The 7 duplicated dilutions were then subjected to amplification and sequencing in 2 replicate experiments. The expected and observed frequencies were compared
on a logarithmic scale. Replicate 1 is represented by circles and replicate 2 is represented by crosses in all panels. Panel G shows the results from 2 cancer clones that were
present in this tumor.
expected, all 100 diagnostic samples demonstrated a highfrequency clonal rearrangement for at least one receptor, herein
referred to as a “calibrating receptor.” The majority (n ⫽ 94) had at
least 2 calibrating receptors, with 51 having 3 or more.
The IgH complete VHDJH assay was the most frequent gene
rearrangement: at least one IgH VHDJH clonal rearrangement was
detected in 96 of the diagnostic ALL samples (Table 1). TRD@ was
the second most informative receptor, and at least one TRD@
clonal rearrangement was detected in 63 of the samples (Table 1).
In contrast, TRB@ clonal rearrangements were only identified in
16 samples (Table 1). Concomitant clonal rearrangements of IgH
(mature and/or immature) and at least 1 TCR gene were found in
86 of 100 samples collected at diagnosis.
Table 1. No. of patients by no. of calibrating clones in each receptor
No. of index clones
Receptor
IGH@-VDJ
0
1
2
3
4
1
4
51
35
9
IGH@-DJ
67
22
9
2
TRB@
84
13
3
TRD@
37
41
13
TRG@
47
29
24
0
2
18
All receptors
5
6
7
8
11
16
6
4
3
1
9
29
21
We also assessed the cumulative number of clonal gene
rearrangements that were present in each sample, because more
than one clonal rearrangement could be detected with one receptor.
Among the 100 diagnostic samples studied, 98, 80, and 51 had 2 or
more, 3 or more, and 4 or more clonal rearrangements across all
receptors, respectively (Table 1).
One advantage of our method is that all rearranged genes are
captured, enabling the comprehensive delineation of the landscape
of IgH genetic diversity and clonal selection that occurred during
the leukemogenic process.10 We analyzed 106 of the 110 diagnostic
ALL samples with complete IgH VHDJH gene rearrangements for
evidence of IgH clonal evolution because of ongoing secondary
recombination events during disease progression. The evolved
clonotypes were identified by virtue of their sequence relatedness
to the high-frequency clonal rearrangement. The number of evolved
clones per ALL sample varied widely from 0-6933 clonotypes.
Fifty-six of 106 samples (53%) demonstrated VHDJH to VHDJH
evolution, which is consistent with a VH replacement model.11-16
These samples could be categorized into 5 groups based on the
number of evolved clones present, with 39 patients (37%) having
1-50 evolved clones and 17 patients (16%) having a high degree of
evolution (⬎ 50 evolved clones; Figure 3). These data show that
the sequencing assay captured the extensive evolution that is
present in diagnostic samples, a potential cause of false-negative
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
BLOOD, 20 DECEMBER 2012 䡠 VOLUME 120, NUMBER 26
DEEP-SEQUENCING METHOD FOR MRD DETECTION
Table 2. Summary of discordant MRD results for the sequencing,
flow cytometry, and ASO-PCR methods
0.6
Fraction of samples
with (N) evolved clones
5177
% MRD
Patient ID
0.4
0.2
es
cl
on
00
cl
Number of evolved clones
Figure 3. Clonal evolution mechanisms at the IgH gene locus. Diagnostic
samples containing a clonal gene rearrangement, as determined using the VDJ
(n ⫽ 106) assay were categorized into 5 groups based on the number of evolved
clones present in the diagnostic sample. The fraction of all samples having a given
number of evolved clones is shown.
results during MRD monitoring by ASO-PCR focusing on selected
gene rearrangements.
Comparison of MRD results by immune repertoire sequencing
with those by standard MRD assays
Flow cytometry
9
248 496
0.00004
UD
UD
12
133 669
0.0027
UD
0.0017
25
142 310
0.0106
UD
0.0005
30
120 307
0.0032
UD
0.0076
31
1 109 253
0.0014
UD
UD
41
626 380
0.0005
UD
0.0051
58
171 326
0.0102
UD
0.0120
73
983 289
0.0004
UD
UD
98
162 217
0.0097
UD
0.0038
29
161 142
0.9607
UD
1.2000
36
1 070 242
UD
UD
0.0020
PCR
100
0
10
1
0.1
0.01
0.001
0.0001
We first analyzed concordance between MRD results obtained
by our assay and flow cytometry, which was used to monitor MRD
in 105 of the 106 cases. The sequencing test was performed without
knowledge of the results of flow cytometry testing. The 2 methods
gave concordant MRD⫹ or MRD⫺ results in 95 of 105 (90%)
samples (Figure 4A and supplemental Table 3). In 10 of 105 samples
(10%), MRD was positive by sequencing, but undetectable by flow
cytometry (Figure 4A and Table 2); 7 of these 10 samples were also
positive by ASO-PCR. Most of the discordance between the
sequencing assay and flow cytometry can be explained by the
sensitivity limitations of flow cytometry. For example, MRD levels
ranged between 0.00004% and 0.011% by sequencing in 9 of the
10 discordant samples (Table 2). MRD was undetectable by flow
cytometry and measured at 0.96% and 1.2% by sequencing and
ASO-PCR, respectively, in the final discordant sample (Table 2).
We next compared the MRD results obtained by immune
repertoire sequencing and ASO-PCR. Again, the sequencing test
was performed without knowledge of the previously collected
results by ASO-PCR. Results were concordant in 102 of 106 follow-up
samples (96%): 35 (33%) were MRD⫹ and 67 (63%) were MRD⫺
by both methods (Figure 4B and supplemental Table 3). In 3 of
106 samples, MRD was positive by sequencing (0.0014%, 0.0004%,
and 0.00004%), but undetectable by ASO-PCR (Figure 4B and
Table 2), a result that could be explained by the fact that these
levels of MRD would be outside of the quantitative range of
ASO-PCR.5 In the remaining sample, a faint signal corresponding
to 0.0020% MRD was detected by ASO-PCR (performed by a
limiting-dilution assay), but MRD was undetectable by sequencing
(Figure 4B and Table 2). The reason for this discrepancy is unclear.
28
ASO-PCR (%)
Flow cytometry (%)
We assessed MRD using the sequencing assay in follow-up
samples collected during therapy from 106 patients with newly
diagnosed B-lineage ALL and IgH VHDJH clonal gene rearrangements at diagnosis. In addition to the previously demonstrated
presence of IgH gene rearrangements at diagnosis, the main criteria
for inclusion in the study was the availability of abundant surplus
DNA collected during follow-up. In the Total XV trial, MRD was
measured by flow cytometry and ASO-PCR during and at the end
of remission induction therapy (on days 19, 26, and 46), during
continuation therapy (at weeks 7, 17 and 48), and at the end of
therapy (at week 120 for girls and week 146 for boys).7 Of the
106 samples studied, 45 were collected during induction therapy
(n ⫽ 18) or at the end of remission induction therapy (n ⫽ 27),
44 during continuation therapy, and 17 at the end of therapy
(supplemental Table 3), thus providing a full representation of the
different types of BM cellularity found during ALL treatment.
67
10
Sequencing (%)
100
1
10
1
0.1
0.01
0.001
0.0001
35
67
3
100
10
1
0.1
0.01
0.001
0.0001
100
10
1
0.1
0.01
0.001
0.0001
Figure 4. Comparison of MRD results obtained by
sequencing, flow cytometry, and ASO-PCR. MRD
results obtained using the sequencing method were
compared with flow cytometry results for 105 ALL patients (left) and with ASO-PCR results for 106 ALL
patients (right). In each panel, the numbers of concordant
measurements are shown in the lower left and upper
right and the number of discordant measurements are
shown in the upper left and lower right.
Sequencing
UD indicates undetectable.
>5
51
-5
00
50
6-
on
es
es
on
cl
cl
5
1-
0
cl
on
on
es
es
0.0
Input cells, n
Sequencing (%)
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
5178
BLOOD, 20 DECEMBER 2012 䡠 VOLUME 120, NUMBER 26
FAHAM et al
STEP 1: IDENTIFICATION OF LEUKEMIC CLONE IN DIAGNOSTIC SAMPLES
Sample collection
Clonality test for
all receptors
Identify leukemic clone based on frequency in
immune cell repertoire
10 0
IgH@ V-J
10
TRB@
Bone marrow aspirate
TRD@
TRG@
Clone frequency (%)
IgH@ D-J
1
0.1
0.01
0.001
0.0001
IgH@VJ IgH@DJ
TRB@
TRD@
TRG@
STEP 2: DETECTION OF LEUKEMIC CLONE IN FOLLOW-UP SAMPLES
Monitor MRD over time in serial follow-up samples
0.1
MRD detected
9 months after
end of therapy
0.01
0.001
0.0001
100000
10000
1000
100
10
1
12
9
M
on
th
6
M
on
th
M
on
th
3
0
0
TRB@
TRB@
1000000
M
on
th
Bone marrow aspirate
OR
Peripheral blood
Leukemic molecules/million leukocytes
IgH@VJ
IgH@ V-J
M
on
th
MRD test for
positive receptors
Clone frequency (%)
Serial follow-up
sample collection
Months after end of therapy
Figure 5. Schematic diagram of sequencing analysis and work flow for prospective sample collection.
The DNA analyzed by the sequencing test in this sample corresponded to 1.07 million input cells. Therefore, if the ASO-PCR
estimate was correct, DNA from approximately 20 ALL cells
should have been present in the sample and this number of clonal
rearrangements should have been easily detectable by the sequencing assay. However, MRD estimates by ASO-PCR can be inaccurate at such extremely low levels, and it is possible that the sample
analyzed by sequencing did not contain any leukemic DNA at all.
Alternatively, the ASO-PCR signal may have been an artifact. This
discrepancy notwithstanding, these comparisons with the gold
standard MRD assays provide strong evidence of the reliability and
sensitivity of the sequencing assay when applied to clinical
samples collected from patients undergoing chemotherapy.
When present in the detection range, MRD levels measured by
flow cytometry are typically accurate, because this method directly
counts leukemic cells among normal cells.4,17 In the 29 samples
with detectable MRD in all 3 platforms, MRD levels measured
by the sequencing assay were highly correlated with those of
flow cytometry. Specifically, the MRD level measured by the
2 platforms showed an r2 of 0.83 and a slope of 1.03, supporting the
quantitative accuracy of the sequencing assay. ASO-PCR versus flow
cytometry MRD results showed an r2 of 0.75 and a slope of 1.04.
We tested the concordance between MRD results using the IgH
VHDJH sequencing assay and other receptor rearrangement sequencing assays (ie, IgH DJH and TCR assays) in a subset of 9 samples
that had previously been identified as having non-IgH recombinations. In all cases, results were concordant with the previously
observed data. Specifically, 7 samples were MRD⫺ according to
both the IgH VHDJH and a second receptor, and 2 samples were
MRD⫹ according to the IgH VHDJH and a second receptor
(supplemental Table 4).
Discussion
We developed a novel approach to monitoring response to treatment in patients with leukemia. The method employs consensus
primers and high-throughput sequencing to universally amplify and
sequence all rearranged IgH and TCR gene segments present in a
leukemic clone. It also allows the identification of all clonal gene
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
BLOOD, 20 DECEMBER 2012 䡠 VOLUME 120, NUMBER 26
rearrangements in diagnostic samples and enables tracking of their
evolution during therapy. A previous study demonstrated the utility
of high-throughput sequencing for MRD quantitation in chronic
lymphocytic leukemia.18 In addition, while this manuscript was in
preparation, Wu et al reported the use of high-throughput sequencing to detect MRD in patients with T-lineage ALL; their results
compared favorably with those of flow cytometry, but no comparison was made with ASO-PCR.19 In the present study, we have
shown that the sequencing assay is precise, quantitative, and
sensitive when applied to BM samples collected throughout
treatment in patients with B-lineage ALL. Our method is quantitative at frequencies above 10⫺5 and the lower limit of detection is
below 10⫺6. Moreover, the technical performance data presented
herein demonstrate that the sequencing assay sensitivity is limited
only by the number of input cells and thus can detect residual
disease at levels well below 1 in 1 million leukocytes (0.0001%).
This represents at least 1-2 orders of magnitude higher sensitivity
than standard ASO-PCR and flow-cytometric methods, respectively.
Comparisons with gold standard MRD assays provide strong
evidence of the reliability and sensitivity of the sequencing assay
when applied to clinical samples collected from patients undergoing chemotherapy. Our assay offers potential advantages over
ASO-PCR, the standard method to target IgH and TCR genes for
MRD studies. First, it allows monitoring of all leukemic rearrangements regardless of their prevalence at diagnosis. This feature
should abrogate the risk of false-negative MRD results due to
clonal evolution during the course of the disease, in which
subclones representing a minority of antigen-receptor gene rearrangements might be neglected at diagnosis but become predominant at relapse.14,20-25 We observed that the majority of samples
studied at diagnosis already had a high degree of genetic diversity
at the IgH locus, which is in agreement with the results of another
study focusing on the immune repertoire sequencing method to
determine the prevalence of clonal evolution in diagnostic samples
from patients with B-lineage ALL.26 Second, current ASO-PCR
assays require the development of customized primer sets and
assay conditions for the detection of each individual clonal gene
rearrangement in each patient, a laborious and time-consuming
process that becomes increasingly so if multiple receptors and/or
clonal rearrangements are assayed. Because the sequencing assay
uses a set of universal primers, it can assess multiple clonal
rearrangements in every patient without the need for individualized
procedures. We currently estimate that the assay will have a
turnaround time of approximately 7 days for MRD detection.
A schematic diagram of the analysis and workflow of our method
when performed prospectively is shown in Figure 5. Finally, there
is evidence suggesting that MRD positivity below 0.01% has
prognostic implications,6 although it remains to be determined
whether the enhanced sensitivity of the immune repertoire sequencing approach will provide additional clinical information in the
context of current chemotherapy and allogeneic stem cell transplantation protocols for ALL. Conceivably, a high sensitivity of MRD
detection before transplantation could be useful in improving the
DEEP-SEQUENCING METHOD FOR MRD DETECTION
5179
timing of the procedure27; after transplantation, it should allow for
early intervention to avoid relapse.
Our approach relies on high-throughput sequencing to identify
leukemia-associated gene rearrangements at diagnosis and to
measure their prevalence during treatment. Although the costs of
the sequencing process were historically prohibitive for routine
application, they have been steadily decreasing by a factor of
approximately 20 000 over the past decade. The current sequencing
costs for rearranged antigen-receptor genes are comparable to those
of flow cytometry and ASO-PCR and are predicted to decrease
substantially with further advances in sequencing technology.
High-throughput sequencing data may be complex to interpret, but,
as shown by our results, the analytic algorithms that we designed
allow unequivocal detection and accurate quantitation of leukemiaderived sequences. The prognostic power of MRD during treatment
has been amply demonstrated in numerous correlative studies
performed in patients with newly diagnosed childhood and adult
ALL6,7,17,28-37 or relapsed ALL,38-40 and in patients undergoing
hematopoietic stem cell transplantation.27,41 Monitoring of MRD
has become a central component of the modern management of
patients with ALL7 and is beginning to be introduced as a criterion
for testing novel antileukemic agents.42 The sensitivity, universal
applicability, and capacity to capture clonal evolution of the
method described herein, together with the results of our comparison with standard MRD assays in clinical samples, strongly support
its potential as a next-generation MRD test for ALL. Although we
limited our study to the most common form of ALL, B-lineage, the
same approach could also be applied to T-lineage ALL or other
lymphoid malignancies such as chronic lymphocytic leukemia,
non-Hodgkin lymphoma, and multiple myeloma.
Acknowledgments
This work was supported in part by grants CA60419 and CA21765
from the National Cancer Institute, by the American Lebanese
Syrian Associated Charities, and by research funding from Sequenta Inc. (to M.F., J.Z., M.M., and V.E.H.C.).
Authorship
Contribution: M.F., J.Z., M.M., and V.E.H.C. performed the
sequencing assays and analyzed and interpreted the data; P.S. and
E.C.-S. provided the ASO-PCR and flow cytometry MRD data;
C.-H.P. led the clinical trial under which the samples were collected
for MRD studies; M.F. and D.C. designed the research, analyzed
and interpreted the data, and wrote the manuscript; and all authors
provided input on and approved the final version of the manuscript.
Conflict-of-interest disclosure: M.F., J.Z., M.M., and V.E.H.C.
are employees of and stockholders in Sequenta Inc. The remaining
authors declare no competing financial interests.
Correspondence: Malek Faham, MD, PhD, 400 E Jamie
Ct, Ste 301, South San Francisco, CA 94080; e-mail:
malek.faham@sequentainc.com.
References
1. Gökbuget N, Hoelzer D. Treatment of adult acute
lymphoblastic leukemia. Semin Hematol. 2009;
46(1):64-75.
2. Pui CH, Carroll WL, Meshinchi S, Arceci RJ. Biology, risk stratification, and therapy of pediatric
acute leukemias: an update. J Clin Oncol. 2011;
29(5):551-565.
3. Brüggemann M, Schrauder A, Raff T, et al. Standardized MRD quantification in European ALL
trials: proceedings of the Second International
Symposium on MRD assessment in Kiel, Germany, 18-20 September 2008. Leukemia. 2010;
24(3):521-535.
4. Campana D. Minimal residual disease in acute
lymphoblastic leukemia. Hematology Am Soc Hematol Educ Program. 2010;2010:7-12.
5. van der Velden VH, Cazzaniga G, Schrauder A,
et al. Analysis of minimal residual disease by Ig/
TCR gene rearrangements: guidelines for interpretation of real-time quantitative PCR data. Leukemia. 2007;21(4):604-611.
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
5180
FAHAM et al
6. Stow P, Key L, Chen X, et al. Clinical significance
of low levels of minimal residual disease at the
end of remission induction therapy in childhood
acute lymphoblastic leukemia. Blood. 2010;
115(23):4657-4663.
7. Pui CH, Campana D, Pei D, et al. Treating childhood acute lymphoblastic leukemia without cranial irradiation. N Engl J Med. 2009;360(26):
2730-2741.
8. Coustan-Smith E, Song G, Clark C, et al. New
markers for minimal residual disease detection in
acute lymphoblastic leukemia. Blood. 2011;
117(23):6267-6276.
9. Faham M, Willis T. Monitoring health and disease
status using clonotype profiles. US patent application 2011/0207134A1. August 25, 2011.
10. Greaves M, Maley CC. Clonal evolution in cancer. Nature. 2012;481(7381):306-313.
11. Rosenquist R, Thunberg U, Li AH, et al. Clonal
evolution as judged by immunoglobulin heavy
chain gene rearrangements in relapsing
precursor-B acute lymphoblastic leukemia.
Eur J Haematol. 1999;63(3):171-179.
12. Kitchingman GR. Immunoglobulin heavy chain
gene VH-D junctional diversity at diagnosis in patients with acute lymphoblastic leukemia. Blood.
1993;81(3):775-782.
13. Steenbergen EJ, Verhagen OJ, van Leeuwen EF,
von dem Borne AE, van der Schoot CE. Distinct
ongoing Ig heavy chain rearrangement processes
in childhood B-precursor acute lymphoblastic leukemia. Blood. 1993;82(2):581-589.
14. Choi Y, Greenberg SJ, Du TL, et al. Clonal evolution in B-lineage acute lymphoblastic leukemia by
contemporaneous VH-VH gene replacements
and VH-DJH gene rearrangements. Blood. 1996;
87(6):2506-2512.
15. Zhang Z, Burrows PD, Cooper MD. The molecular basis and biological significance of VH replacement. Immunol Rev. 2004;197:231-242.
16. Koralov SB, Novobrantseva TI, Konigsmann J,
Ehlich A, Rajewsky K. Antibody repertoires generated by VH replacement and direct VH to JH joining. Immunity. 2006;25(1):43-53.
17. Coustan-Smith E, Behm FG, Sanchez J, et al.
Immunological detection of minimal residual disease in children with acute lymphoblastic leukaemia. Lancet. 1998;351(9102):550-554.
18. Logan AC, Gao H, Wang C, et al. High-throughput
VDJ sequencing for quantification of minimal residual disease in chronic lymphocytic leukemia
and immune reconstitution assessment. Proc
Natl Acad Sci U S A. 2011;108(52):21194-21199.
19. Wu D, Sherwood A, Fromm JR, et al. Highthroughput sequencing detects minimal residual
disease in acute T lymphoblastic leukemia. Sci
Transl Med. 2012;4(134):134ra63.
20. Szczepański T, Willemse MJ, Brinkhof B, van
Wering ER, van der Burg M, van Dongen JJ.
Comparative analysis of Ig and TCR gene rearrangements at diagnosis and at relapse of child-
BLOOD, 20 DECEMBER 2012 䡠 VOLUME 120, NUMBER 26
hood precursor-B-ALL provides improved strategies for selection of stable PCR targets for
monitoring of minimal residual disease. Blood.
2002;99(7):2315-2323.
21. Li A, Zhou J, Zuckerman D, et al. Sequence analysis of clonal immunoglobulin and T-cell receptor
gene rearrangements in children with acute lymphoblastic leukemia at diagnosis and at relapse:
implications for pathogenesis and for the clinical
utility of PCR-based methods of minimal residual
disease detection. Blood. 2003;102(13):45204526.
22. de Haas V, Verhagen OJ, von dem Borne AE,
Kroes W, van den Berg H, van der Schoot CE.
Quantification of minimal residual disease in children with oligoclonal B-precursor acute lymphoblastic leukemia indicates that the clones that
grow out during relapse already have the slowest
rate of reduction during induction therapy. Leukemia. 2001;15(1):134-140.
23. Choi S, Henderson MJ, Kwan E, et al. Relapse in
children with acute lymphoblastic leukemia involving selection of a preexisting drug-resistant
subclone. Blood. 2007;110(2):632-639.
24. Konrad M, Metzler M, Panzer S, et al. Late relapses evolve from slow-responding subclones in
t(12;21)-positive acute lymphoblastic leukemia:
evidence for the persistence of a preleukemic
clone. Blood. 2003;101(9):3635-3640.
25. Henderson MJ, Choi S, Beesley AH, et al.
Mechanism of relapse in pediatric acute lymphoblastic leukemia. Cell Cycle. 2008;7(10):13151320.
26. Gawad C, Pepin F, Carlton V, et al. Massive evolution of the immunoglobulin heavy chain locus in
children with pediatric B precursor acute lymphoblastic leukemia [published online ahead of print
August 28, 2012]. Blood. doi:10.1182/blood2012-05-429811.
27. Leung W, Campana D, Yang J, et al. High success rate of hematopoietic cell transplantation
regardless of donor source in children with very
high-risk leukemia. Blood. 2011;118(2):223-230.
28. Cavé H, van der Werff ten Bosch J, Suciu S, et al.
Clinical significance of minimal residual disease
in childhood acute lymphoblastic leukemia. European Organization for Research and Treatment of
Cancer–Childhood Leukemia Cooperative Group.
N Engl J Med. 1998;339(9):591-598.
29. van Dongen JJ, Seriu T, Panzer-Grumayer ER, et
al. Prognostic value of minimal residual disease
in acute lymphoblastic leukaemia in childhood.
Lancet. 1998;352(9142):1731-1738.
30. Dworzak MN, Froschl G, Printz D, et al. Prognostic significance and modalities of flow cytometric
minimal residual disease detection in childhood
acute lymphoblastic leukemia. Blood. 2002;99(6):
1952-1958.
31. Brüggemann M, Raff T, Flohr T, et al. Clinical significance of minimal residual disease quantification in adult patients with standard-risk acute lym-
phoblastic leukemia. Blood. 2006;107(3):11161123.
32. Raff T, Gokbuget N, Luschen S, et al. Molecular
relapse in adult standard-risk ALL patients detected by prospective MRD monitoring during and
after maintenance treatment: data from the
GMALL 06/99 and 07/03 trials. Blood. 2007;
109(3):910-915.
33. Zhou J, Goldwasser MA, Li A, et al. Quantitative
analysis of minimal residual disease predicts relapse in children with B-lineage acute lymphoblastic leukemia in DFCI ALL Consortium Protocol 95-01. Blood. 2007;110(5):1607-1611.
34. Borowitz MJ, Devidas M, Hunger SP, et al. Clinical significance of minimal residual disease in
childhood acute lymphoblastic leukemia and its
relationship to other prognostic factors: a Children’s Oncology Group study. Blood. 2008;
111(12):5477-5485.
35. Bassan R, Spinelli O, Oldani E, et al. Improved
risk classification for risk-specific therapy based
on the molecular study of minimal residual disease (MRD) in adult acute lymphoblastic leukemia (ALL). Blood. 2009;113(18):4153-4162.
36. Conter V, Bartram CR, Valsecchi MG, et al. Molecular response to treatment redefines all prognostic factors in children and adolescents with
B-cell precursor acute lymphoblastic leukemia:
results in 3184 patients of the AIEOP-BFM ALL
2000 study. Blood. 2010;115(16):3206-3214.
37. Schrappe M, Valsecchi MG, Bartram CR, et al.
Late MRD response determines relapse risk
overall and in subsets of childhood T-cell ALL:
results of the AIEOP-BFM-ALL 2000 study. Blood.
2011;118(8):2077-2084.
38. Coustan-Smith E, Gajjar A, Hijiya N, et al. Clinical
significance of minimal residual disease in childhood acute lymphoblastic leukemia after first relapse. Leukemia. 2004;18(3):499-504.
39. Paganin M, Zecca M, Fabbri G, et al. Minimal residual disease is an important predictive factor of
outcome in children with relapsed ‘high-risk’ acute
lymphoblastic leukemia. Leukemia. 2008;22(12):
2193-2200.
40. Raetz EA, Borowitz MJ, Devidas M, et al. Reinduction platform for children with first marrow relapse of acute lymphoblastic Leukemia: A Children’s Oncology Group Study[corrected]. J Clin
Oncol. 2008;26(24):3971-3978.
41. Bader P, Kreyenberg H, Henze GH, et al. Prognostic value of minimal residual disease quantification before allogeneic stem-cell transplantation
in relapsed childhood acute lymphoblastic leukemia: the ALL-REZ BFM Study Group. J Clin Oncol. 2009;27(3):377-384.
42. Topp MS, Kufer P, Gokbuget N, et al. Targeted
therapy with the T-cell-engaging antibody blinatumomab of chemotherapy-refractory minimal residual disease in B-lineage acute lymphoblastic
leukemia patients results in high response rate
and prolonged leukemia-free survival. J Clin Oncol. 2011;29(18):2493-2498.
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
2012 120: 5173-5180
doi:10.1182/blood-2012-07-444042 originally published
online October 16, 2012
Deep-sequencing approach for minimal residual disease detection in
acute lymphoblastic leukemia
Malek Faham, Jianbiao Zheng, Martin Moorhead, Victoria E. H. Carlton, Patricia Stow, Elaine
Coustan-Smith, Ching-Hon Pui and Dario Campana
Updated information and services can be found at:
http://www.bloodjournal.org/content/120/26/5173.full.html
Articles on similar topics can be found in the following Blood collections
Clinical Trials and Observations (4395 articles)
Lymphoid Neoplasia (2381 articles)
Information about reproducing this article in parts or in its entirety may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests
Information about ordering reprints may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#reprints
Information about subscriptions and ASH membership may be found online at:
http://www.bloodjournal.org/site/subscriptions/index.xhtml
Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society
of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036.
Copyright 2011 by The American Society of Hematology; all rights reserved.