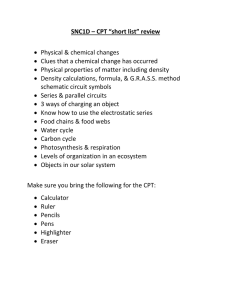
Modifiers Pertaining to Surgery or Services within
advertisement

NOTE: Should you have landed here as a result of a search engine (or other) link, be advised that these files contain material that is copyrighted by the American Medical Association. You are forbidden to download the files unless you read, agree to, and abide by the provisions of the copyright statement. Read the copyright statement now and you will be linked back to here. Modifiers Pertaining to Surgery or Services within the Global Period Modifiers assure that the carrier will give consideration to the special circumstances that may affect payment. Omitting modifiers may result in payment denials. If a review is requested on a denied service, the appropriate modifier must be included with the review. A description of the service will not be sufficient to change the original claim decision. Use of the modifiers in this section applies to both major procedures with a 90-day postoperative period and minor procedures with a 10-day postoperative period (and/or a zero day postoperative period in the case of CPT modifiers 22 and 25. CPT Modifier 22 – Unusual Procedural Services When the service(s) provided is greater than that usually required for the listed procedure, it may be identified by adding CPT modifier 22 to the usual procedure number. Use of this modifier requires additional documentation. Examples include an operative report and a concise statement specifying how the service differs from the usual. This information must be in the appropriate documentation record or sent via FAX for electronic claims. If paper claims are submitted, the information must be on an attachment to the CMS-1500 claim form. Failure to submit the documentation appropriately may result in payment for the surgical code only, based on the Medicare Physician Fee Schedule Database. CPT Modifier 24 – Unrelated Evaluation and Management Service by the Same Physician During a Postoperative Period The physician may need to indicate that an evaluation and management service was performed during a postoperative period for a reason(s) unrelated to the original procedure. This circumstance may be reported by adding the CPT modifier 24 to the appropriate level of E/M service. Additional documentation required with this modifier is: sufficient documentation to establish that the visit was unrelated to the surgery; an ICD-9 diagnosis code that clearly indicates that the reason for the encounter was unrelated to the surgery. The documentation to establish the visit was unrelated to the surgery must appear in the appropriate documentation record for electronic claims or on an attachment to the CMS-1500 claim form for paper claims. Failure to submit this documentation appropriately may result in services denied as part of the cost of the surgical procedure. 1 CPT Modifier 25 – Significant, Separately Identifiable Evaluation and Management Service by the Same Physician on the Same Day of the Procedure or Other Service The physician may need to indicate that on the day a procedure or service identified by a CPT code was performed, the patient's condition required a significant, separately identifiable E/M service above and beyond the other service provided or beyond the usual preoperative and postoperative care associated with the procedure that was performed. The E/M service may be prompted by the symptom or condition for which the procedure and/or service was provided. Different diagnoses are not required for reporting the E/M services on the same date. This circumstance may be reported by adding the CPT modifier 25 to the appropriate level of E/M service. Note: This modifier is not used to report an E/M service that resulted in a decision to perform surgery. See CPT modifier 57. CPT Modifier 50 – Bilateral Procedure Unless otherwise identified in the listings, bilateral procedures that are performed at the same operative session must be identified by adding the CPT modifier 50 to the appropriate five-digit code. Note: To prevent duplicate denials, surgical procedures billed bilaterally must be reported using the surgical code and the 50 CPT modifier billed on one detail. CPT Modifier 51 – Multiple Procedures When multiple procedures, other than Evaluation and Management Services, are performed at the same session by the same provider, the primary procedure or service may be reported as listed. The additional procedure(s) or service(s) may be identified by appending the CPT modifier 51 to the additional procedure or service code(s). Note: This modifier must not be appended to designated "add-on" codes. CPT Modifier 52 – Reduced Services Under certain circumstances a service or procedure is partially reduced or eliminated at the physician's discretion. Under these circumstances, the service provided can be identified by its usual procedure number and the addition of the CPT modifier 52 signifying that the service is reduced. This provides a means of reporting reduced services without disturbing the identification of the basic service. Note: For hospital outpatient reporting of a previously scheduled procedure and/or service that is partially reduced or cancelled as a result of extenuating circumstances or those that threaten the well-being of the patient prior to or after administration of anesthesia, see CPT modifiers 73 and 74 (see modifiers approved for ASC hospital outpatient use). 2 Use of this modifier requires additional documentation such as an operative report and a concise statement specifying how the service differs from the usual. This information must be indicated in the appropriate documentation record for electronic claims or sent via FAX. It may also be attached to the CMS-1500 claim form for paper claims. Failure to submit this documentation appropriately may result in services rejected as unprocessable. CPT Modifier 53 – Discontinued Procedure Under certain circumstances, the physician may elect to terminate a surgical or diagnostic procedure. Due to extenuating circumstances or those that threaten the well being of the patient, it may be necessary to indicate that a surgical or diagnostic procedure was started but discontinued. This circumstance must be reported by adding the CPT modifier 53 to the code reported by the physician for the discontinued procedure. Note: This modifier is not used to report the elective cancellation of a procedure prior to the patient's anesthesia induction and/or surgical preparation in the operating suite. For outpatient hospital/ambulatory surgery center (ASC) reporting of a previously scheduled procedure/service that is partially reduced or cancelled as a result of extenuating circumstances or those that threaten the well being of the patient prior to or after administration of anesthesia, see CPT modifiers 73 and 74 (see modifiers approved for ASC hospital outpatient use). Use of this modifier requires additional documentation such as a statement indicating why it was medically necessary to discontinue the procedure. The statement must be indicated in the appropriate documentation record for electronic claims. If paper claims are submitted, the statement must appear on an attachment to the CMS-1500 claim form. Failure to submit this documentation appropriately may result in services rejected as unprocessable. CPT Modifier 54 – Surgical Care Only When one physician performs a surgical procedure and another provides preoperative and/or postoperative management, surgical services must be identified by adding the CPT modifier 54 to the usual procedure number. CPT Modifier 55 – Postoperative Management Only 3 When one physician performs the postoperative management and another physician performs the surgical procedure, the postoperative component must be identified by adding the CPT modifier 55 to the usual procedure number. Use of this modifier requires additional documentation and includes both the number of days postoperative care is provided, and the assumed or relinquished dates of the postoperative care. The number of postoperative days and the assumed or relinquished dates must be indicated in the appropriate documentation record for electronic claims. 1. For paper claims, the number of postoperative days must be indicated in Item 24g and the assumed or relinquished dates must be indicated in Item 19 of the CMS-1500 claim form. 2. Failure to submit this documentation appropriately may result in the services rejected as unprocessable. Claims for postoperative management only should also show the surgery as the procedure code and the date of the surgery as the date of service and the number of postoperative days the patient was seen. CPT Modifier 56 – Preoperative Management Only When one physician performs the preoperative care and evaluation and other physician performs the surgical procedure, the preoperative component must be identified by adding the CPT modifier 56 to the usual procedure number. CPT Modifier 57 – Decision for Surgery An evaluation and management service that resulted in the initial decision to perform the surgery must be identified by adding the CPT modifier 57 to the appropriate level of E/M service. CPT Modifier 58 – Staged or Related Procedure or Service by the Same Physician during the Postoperative Period The physician may need to indicate that the performance of a procedure or service during the postoperative period was: a) planned prospectively at the time of the original procedure (staged); b) more extensive than the original procedure; or c) for the therapy following a diagnostic surgical procedure. This circumstance must be reported by adding the CPT modifier 58 to the staged or related procedure. Note: This modifier is not used to report the treatment of a problem that requires a return to the operating room. See CPT modifier 78. CPT Modifier 59 – Distinct Procedural Service 4 Under certain circumstances, the physician may need to indicate that a procedure or service was distinct or independent from other services performed on the same day. CPT modifier 59 is used to identify procedures/services that are not normally reported together, but are appropriate under the circumstances. This may represent a different session or patient encounter, different procedure or surgery, different site or organ system, separate incision/excision, separate lesion, or separate injury (or area of injury in extensive injuries) not ordinarily encountered or performed on the same day by the same physician. When another modifier is appropriate it should be used rather than CPT modifier 59. CPT Modifier 62 – Two Surgeons When two surgeons work together as primary surgeons performing distinct part(s) of a single reportable procedure, each surgeon must report his/her distinct operative work by adding the CPT modifier 62 to the single definitive procedure code. Each surgeon must report the co-surgery once using the same procedure code. If additional procedure(s), including add-on procedure(s), are performed during the same surgical session, separate code(s) may be reported without the CPT modifier 62 added. Note: If a co-surgeon acts as an assistant in the performance of additional procedure(s) during the same surgical session, those services may be reported using separate procedure code(s) with the CPT modifier 80 or CPT modifier 81 added, as appropriate. CPT Modifier 66 – Surgical Team Under some circumstances, highly complex procedures (requiring the concomitant services of several physicians, often of different specialties, plus other highly skilled, specially trained personnel, and various types of complex equipment) are carried out under the "surgical team" concept. Such circumstances must be identified by each participating physician with the addition of the CPT modifier 66 to the basic procedure number used for reporting services. CPT Modifier 76 – Repeat Procedure by Same Physician The physician may need to indicate that a procedure or service was repeated subsequent to the original procedure or service. This circumstance must be reported by adding the CPT modifier 76 to the repeated procedure/service. CPT Modifier 77 - Repeat Procedure by Another Physician 5 The physician may need to indicate that a basic procedure or service performed by another physician had to be repeated. This situation must be reported by adding CPT modifier 77 to the repeated procedure/service. 78 Return to the Operating Room for a Related Procedure During the Postoperative Period The physician may need to indicate that another procedure was performed during the postoperative period of the initial procedure. When this subsequent procedure is related to the first, and requires the use of the operating room, it must be reported by adding the CPT modifier 78 to the related procedure. For repeat procedures on the same day, see CPT modifier 76. CPT Modifier 79 Unrelated Procedure or Service by the Same Physician During the Postoperative Period The physician may need to indicate that the performance of a procedure or service during the postoperative period was unrelated to the original procedure. This circumstance must be reported by using the CPT modifier 79. For repeat procedures on the same day, see CPT modifier 76. CPT Modifier 80 – Assistant Surgeon Surgical assistant services may be identified by adding the CPT modifier 80 to the usual procedure number(s). Additional documentation required with this modifier includes a statement that no qualified resident was available to perform the service, or a statement indicating that no exceptional medical circumstances exist, or a statement indicating the primary surgeon has an across the board policy of never involving residents in the preoperative, operative or postoperative care of his/her patients. 1. If one of the above is not provided, the name and address of the hospital where the services were furnished must be indicated. The statement must be submitted in the appropriate documentation record for electronic claims and on an attachment to the CMS-1500 claim form for paper claims. 2. The name and address of the hospital where services were furnished must be indicated in the appropriate documentation record for electronic claims and in Item 32 of the CMS-1500 claim form for paper claims. 3. Failure to submit this documentation appropriately may result in services rejected as unprocessable. CPT Modifier 81 – Minimum Assistant Surgeon 6 Minimum surgical assistant services are identified by adding the CPT modifier 81 to the usual procedure number. Additional documentation is required with this modifier and includes a statement that no qualified resident was available to perform the service, or a statement indicating that no exceptional medical circumstances exist, or a statement indicating the primary surgeon has an across the board policy of never involving residents in the preoperative, operative or postoperative care of his/her patients. 1. If one of the above is not provided, the name and address of the hospital where the services were furnished must be indicated. The statement must be submitted in the appropriate documentation record for electronic claims and on an attachment to the CMS-1500 claim form for paper claims. 2. The name and address of the hospital where services were furnished must be indicated in the appropriate documentation record for electronic claims or in Item 32 of the CMS-1500 claim form for paper claims. 3. Failure to submit this documentation appropriately may result in services rejected as unprocessable. CPT Modifier 82 Assistant Surgeon (When Qualified Resident Surgeon is not Available) The unavailability of a qualified resident surgeon is a prerequisite for use of CPT modifier 82 appended to the usual procedure code number(s). CPT Modifier 99 – Multiple Modifiers Under certain circumstances, two or more modifiers may be necessary to completely delineate a service. In such situations, CPT modifier 99 must be added to the basic procedure, and other applicable modifiers must be listed as part of the description of the service. HCPCS Modifier AS – Assistant At Surgery Physician assistant, nurse practitioner, or clinical nurse specialist services for assistant at surgery are identified by adding the HCPCS modifier AS to the usual procedure code number. Additional documentation is required with this modifier and includes a statement that no qualified resident was available to perform the service, or a statement indicating that no exceptional medical circumstances exist, or a statement indicating the primary surgeon has an across the board policy of never involving residents in the preoperative, operative or postoperative care of his/her patients. 1. If one of the above is not provided, the name and address of the hospital where the services were furnished must be indicated. 7 The statement must be submitted in the appropriate documentation record for electronic claims or on an attachment to the CMS-1500 claim form for paper claims. 1. The name and address of the hospital where services were furnished must be indicated in the appropriate documentation record for electronic claims or in Item 32 of the CMS-1500 claim form for paper claims. 2. Failure to submit this documentation appropriately may result in services rejected as unprocessable. 8