When do NHS Bodies have a legal duty of consultation?
advertisement

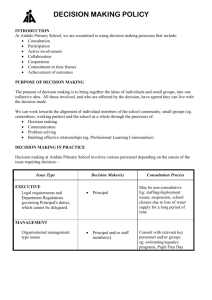
When do NHS Bodies have a legal duty of consultation? Introduction ........................................................................................................................... 2 What are the core statutory duties?.................................................................................... 2 A duty to consult the public................................................................................................. 2 New reporting duty ............................................................................................................... 3 Guidance on the section 242 consultation duty ................................................................ 3 Changes in the personnel providing existing services..................................................... 4 A duty to consult Overview and Scrutiny Committees ..................................................... 4 What does consultation involve?........................................................................................ 5 What does consultation mean?........................................................................................... 6 The role of the Local Involvement Networks...................................................................... 6 What is the consequence of failing to consult? ................................................................ 8 What about changes based on financial pressures? ........................................................ 8 What about “temporary” closures or changes in service which are driven by clinical safety concerns? .................................................................................................................. 8 What about changes made to comply with Department of Health policy decisions?.... 9 Contacts................................................................................................................................. 9 Legislation ............................................................................................................................. 9 Cases ..................................................................................................................................... 9 Useful links.......................................................................................................................... 10 appendix 4 - legal advice (2) 1 Introduction As we head into a new round of controversial changes to the way that local health services are delivered, we are also seeing an increasing number of legal challenges based on alleged failures by local health bodies to consult their local populations before taking action. High profile decisions by NHS bodies in cases such as Trafford Healthcare NHS Trust and South West Strategic Health Authority have been the subject to challenge by Judicial Review. This briefing gives general advice about NHS duties to consult. However the law is evolving and NHS bodies are urged to seek specific advice if they are involved in reconfigurations or receive threats of Judicial Review. What are the core statutory duties? NHS bodies have two separate legal duties to consult about the way that the NHS is operating and about proposed changes. The duties focus on: • consulting patients and the public, and • consulting the local authority Overview and Scrutiny Committee. A duty to consult the public Section 242(1B) of the National Health Service Act 2006 (“2006 Act”), as amended by the Local Government and Public Involvement in Health Act 2007 (“2007 Act”), provides as follows: “Each relevant English body must make arrangements, as respects health services for which it is responsible, which secure that users of those services, whether directly or through representatives, are involved (whether by being consulted or provided with information, or in other ways) in-(a) the planning of the provision of those services, (b) the development and consideration of proposals for changes in the way those services are provided, and (c) decisions to be made by that body affecting the operation of those services.” Subsections (b) and (c) need only be observed if the proposals would have an impact on: (a) the manner in which the services are delivered to users of those services; or (b) the range of health services available to those users. appendix 4 - legal advice (2) 2 The NHS bodies to whom the section applies are as follows: • Strategic Health Authorities; • Primary Care Trusts; • NHS trusts; and • NHS Foundation Trusts. This duty was previously contained in section 11 of the Health and Social Care Act 2001, so in documents prior to 2006 it is referred to as “the section 11 duty”. The legal duty to consult both patients and the wider public falls both on the commissioner of health services and on to those providing services. New reporting duty Section 234 of the 2007 Act inserts sections17A and 24A into the 2006 Act. These sections impose a new duty on Primary Care Trusts and Strategic Health Authorities, at times directed by the Secretary of State, to prepare a report: • on the consultation carried out (or proposed to be carried out) before making its commissioning decisions; and • on the influence that the results of the consultation have on its commissioning decisions. Details in relation to the duties to report will be set out in the Directions to Strategic Health Authorities about reports on Consultation with regard to Commissioning Decisions 2008 and the Directions to Primary Care Trusts about reports on Consultation with regard to Commissioning Decisions 2008 (but at the time of publication of this briefing these are not yet publicly available). Guidance on the section 242 consultation duty The Department has recently published Guidance on the section 242 consultation duty called “Real Involvement: Working with people to improve health services” (“the Guidance”). The Guidance consists of two parts, the first is statutory guidance which must be followed, the second contains recommendations only. The first part of the Guidance sets out the principles of involvement. The involvement must be clear, accessible and transparent, open, inclusive, responsive, sustainable, proactive and focused on improvement. It also suggests different methods of involvement such as focus groups, storytelling, shadowing, blogs, interviews, leaflets and formal consultation. The Guidance confirms that it is for the NHS body to decide which is the best method for the proposal in question and its community. appendix 4 - legal advice (2) 3 The Guidance states that the involvement is only effective if the NHS body has correctly identified the people who should be consulted. In many cases it may be necessary to undertake a health impact assessment and stakeholder analysis to establish who should be involved. The Guidance also places emphasis on the need to involve hard to reach groups such as young people and faith groups. The second part of the Guidance explains and gives guidance on the reporting duties of Strategic Health Authorities and Primary Care Trusts. The duty to consult the public about the health services they receive is a wide, continuing and onerous duty. The amended legislation and the Guidance widen the scope for fulfilling the duty to consult to include providing the public with the information or using ‘other ways’. The Guidance itself positively encourages an NHS body to develop its own methods of consultation. However one thing is clear: there must be consultation unless there is a good reason and therefore the methods to be used or any decision not to consult must be documented with good reasons to avoid the threat of legal challenge. Changes in the personnel providing existing services A change in the identity of the service provider of a health service (such as a local GP service) does not normally attract a duty to consult. Recruiting or replacing a consultant at a local hospital does not normally give rise to a duty to consult. However if the issue is the subject of substantial local controversy where, for example, a GP practice is being replaced by a private company, then a duty under section 242 to consult the public may arise. A duty to consult Overview and Scrutiny Committees The Health and Social Care Act 2001 extended the scope of the local authority Overview and Scrutiny Committees (“OSC”) to review and give opinions on the health services in their area. This provision is now contained in Section 244 of the National Health Service Act 2006. Regulation 4 of the Local Authority (Overview and Scrutiny Committees Health Scrutiny Functions) Regulations 2002 provides that where a local NHS body has under consideration any proposal for a “substantial development of the health service” in the area of a local authority, or for a “substantial variation in the provision” of such service, it shall consult the overview and scrutiny committee of that authority. The meaning of the phrase “substantial development of the health service” has not yet been tested in court but what is substantial must depend on the circumstances. The Guidance suggests that major changes in any of the following may lead to a duty to consult the OSC: • outdated buildings and facilities; • new standards (such as National Service Frameworks); appendix 4 - legal advice (2) 4 • evidence of what works; • workforce pressures; • advances in technology and technique; • new thinking about how services are designed; and • the needs of local people. What does consultation involve? There are many varieties of consultation depending on the extent of a proposed set of changes. The Guidance states that: “What is important is that involvement and consultation is adequate both in terms of time and content and appropriate to the scale of the issue being considered”. It seems clear that a proposal to close a redundant hospital would require a full public consultation in accordance with the guidelines published by the Cabinet Office including: • a detailed consultation document setting out the options; • a summary version for the public; • a dedicated website explaining the issues; • 13 weeks or more of formal consultation; • a public engagement strategy involving public meetings, working with the media and affected local organisations; • engagement with MPs, councillors and the Overview and Scrutiny Committees; and • a report to the PCT or other body on the outcome of consultation. However, other more minor changes require a much lower investment in seeking the views of those affected. Neither the duty to consult the public or an OSC consultation requires a full “cabinet office” style consultation on all issues. The legal duty to consult could be satisfied by some or all of the following depending on the extent of the changes: • a letter to the OSC inviting views (with sufficient time for a response); • advertisements in a local newspaper inviting comments; • a public meeting to discuss the plans in the affected area; • letters to the public who are affected by the decision explaining the options and inviting them to give their views; • website publication and documents placed in local libraries. One method of consulting the public is for plans to be advertised in advance to be discussed at a Board Meeting and for there to be opportunity at the public session of the Board for patients and the public to ask questions and express views. If this is supported by appendix 4 - legal advice (2) 5 publication of minutes of the meeting (on the web site and with copies in public buildings such as libraries) then this will add to the public engagement and thus reduce the chance of a successful legal challenge to the process. As a rule of thumb, the more general consultation an NHS body does with patients and the public about its forward plans, the less consultation is required on the specific implementation of those plans. What does consultation mean? If a legal duty to consult arises, in practice it means that: • The public (and OSC) must be informed of the issues when the plans are at a formative stage; • The options must be put to the public (though it is permissible only to put up one option for change if, on the facts, the NHS body considers that there is only one viable option for change, but remains open to other suggestions. It is always better to put up multiple options if possible. A final option for formal consultation will be strengthened if there is some prior consultation on other possible ways of implementing change); • The views of the public and those affected by the changes must be sought on the proposals and their impact; • There must be a genuine consultation where the views of the public are taken into account when making the decision; • The NHS body must be open to objections being put up to the proposals and/or to other plans being put forward even if not included in the consultation options; • No final decisions – even decisions in principle – must be taken until the public has been consulted and the results of the consultation have been considered by the NHS body. The role of the Local Involvement Networks Until 1 April 2008 Patient and Public Involvement Forums (PPI Forums) existed in NHS trusts (including foundation trusts) to bring to trusts and PCTs the views and experiences of patients, their carers and families. However Section 230 of the Local Government and Public Involvement in Health Act 2007 abolishes PPI Forums and replaces them with Local Involvement Networks (‘LINks’). LINks are gradually being set up throughout the country to replace and broaden the role of Patient Forums. The role of LINks is to give communities a stronger voice in how their health and social care is delivered. They cover all publicly funded health and social care services in an area, irrespective of who provides them. £84m have been allocated over 3 years to fund LINks. Local councils were expected to employ an independent organisation to set up and advise and support the LINk by appendix 4 - legal advice (2) 6 September 2008. The NHS Centre for Involvement also provides advice and support to the establishment of LINks. Section 221 of the Local Government and Public Involvement Act 2007 provides that each local authority must make contractual arrangements to ensure that there are means by which the following activities can be carried out in their area: • promoting, and supporting, the involvement of people in the commissioning, provision and scrutiny of local care services; • enabling people to monitor for the purposes of their consideration the standard or provision of local care services and whether and how local care services could/ought to be improved, and to review for those purposes, the commissioning and provision of local care services; • obtaining the views of people about their needs for, and their experiences of, local care services; • making the views of peoples needs and experiences of local services known to persons responsible for commissioning, providing, managing or scrutinising local care services; and • making reports and recommendations about how local care services could or ought to be improved to persons responsible for commissioning, providing, managing or scrutinising local care services. As a result of the Local Involvement Network Regulations 2008, additional obligations are placed on those commissioning and providing health and social care. Where a service provider, defined as a NHS Trust, Foundation Trust, PCT or local authority, receives a request for information or a report or recommendation from a LINk they must within 20 days of receipt, acknowledge and provide an explanation of actions the service provider intends to take in light of the request or report. If no action is to be taken they must explain why this is the case. Even if the recipient is not the relevant service provider and not responsible for commissioning the service there is a statutory obligation on the NHS body to send a copy of the report or recommendation to the relevant organisation. If the LINk is not satisfied that the issue has been resolved they have the power to escalate the matter to the local council Overview & Scrutiny Committee. In addition, the Local Involvement Networks (Duty of Services-Providers to Allow Entry) Regulations 2008 impose a duty on services providers to allow entry by authorised persons of LINks to certain premises owned or controlled by service providers so that the activities carried on there can be observed. ‘Service provider’ in relation to this power is a wider definition than in relation to reports and recommendations and, in addition to the bodies listed above, includes anyone providing primary medial, primary dental, primary ophthalmic and pharmaceutical services. There are various exclusions where this right does not apply including where operation of the right would compromise service delivery or the privacy or dignity of individuals, private appendix 4 - legal advice (2) 7 part of residential homes and where the LINks representative is not acting reasonably or proportionately. Once LINks are up and running in certain areas, NHS bodies will need to ensure they have in place a procedure for dealing with requests for information, reports or recommendations within the timescales laid down in the legislation and for allowing entry to authorised representatives. Also, where certain health and social care services are provided under contract to an NHS body, it will be essential to ensure that provision is included in these contracts ensuring assisting the NHS body in fulfilling its obligations under the relevant legislation. What is the consequence of failing to consult? A public body which fails to consult leaves itself open to a challenge by way of Judicial Review and may not lawfully be able to takes decisions and thus implement the changes until consultation has occurred. The courts may also award legal costs against the NHS body. What about changes based on financial pressures? The duty to consult arises whether the changes in health service provision are brought to a head by financial pressures, clinical requirements or other reasons, or a combination of two or more factors. It is important to explain within the consultation process which parts of the proposed changes are driven solely by financial considerations and which are driven by clinical or other considerations. In most cases changes will arise from a mixture of financial and non-financial considerations, and this must be explained carefully so that the public understand the mix of factors driving the decision making If financial considerations were omitted from a consultation process as a reason leading to change, but were a factor in driving the proposed changes, or the financial consequences of proposed changes were omitted, the whole consultation exercise could be struck down by the courts. What about “temporary” closures or changes in service which are driven by clinical safety concerns? There have been very different views in the past as to whether the consultation requirements under the 2001 Act (and now the 2006 Act) apply to temporary changes to health services. Following a series of cases including R (on the application of Morris) v. Trafford Healthcare Trust [2006] EWHC 2334 (Admin) it now seems clear that NHS bodies must consider whether they need to consult, even if a change is only temporary or is driven by genuine clinical concerns. Equally there needs to be a sense of proportion, and public consultation is not required for every minor or temporary change in the way a hospital functions or in the way community services are provided. appendix 4 - legal advice (2) 8 If there is any significant change in the way that local health services are provided, even if that change only applies for a few months, it is possible for patients to argue that there was a duty to consult the public and patients under section 242 before the changes are brought into effect. In the Trafford case, Mr Justice Hodge said that the duty to consult was “of high importance” and criticised an NHS Trust that delayed consultation for an extended period and then implemented changes prior to consultation thus predetermining the outcome of the consultation. The Trust were also criticised because the Judge felt that the factual clinical basis on which the decision made was not wholly accurate. However in that case the Judge held there was a duty to consult even where the closure was only intended to be on a temporary basis. What about changes made to comply with Department of Health policy decisions? Most recently in the case of R (on the application of Fudge) v. South West Strategic Health Authority [2007] it was held that the duty to consult arose even when implementing a policy decision of the Department of Health. Even though the Department of Health’s decisions were not the responsibility of the Primary Care Trust, the Primary Care Trust was still responsible for the provision of services and so was subject to the duty. The law is a state of flux at present but the maxim must be – “if in doubt, consult your lawyers to see if you need to consult”. Contacts Julie Jordan, Associate. Tel: 01223 222478. Email: Julie.jordan@mills-reeve.com Fiona Boyse, Senior Solicitor. Tel: 0121 456 8302. Email: Fiona.boyse@mills-reeve.com Legislation The Health and Social Care Act 2001 Local Authority (Overview and Scrutiny Committees Health Scrutiny Functions) Regulations 2002 National Health Service Act 2006 Local Government and Public Involvement in Health Act 2007 Local Involvement Networks Regulations 2008 The Local Involvement Networks (Amendment) Regulations 2008 Local Involvement Networks (Duty of Services-Providers to Allow Entry) Regulations 2008 The National Health Service (Directions by Strategic Health Authorities to Primary Care Trusts Regarding Arrangements for Involvement) Regulations 2008 Cases R (on the application of Morris) v. Trafford Healthcare Trust 2006] EWHC 2334 (Admin) appendix 4 - legal advice (2) 9 R (on the application of Fudge) v. South West Strategic Health Authority [2007] All ER (D) 485 Court of Appeal Useful links Guidance: “Real Involvement: Working with people to improve health services” "Overview and Scrutiny of Health - Guidance" Directions to Strategic Health Authorities about reports on Consultation with regard to Commissioning Decisions 2008 (not yet publicly available) Directions to Primary Care Trusts about reports on Consultation with regard to Commissioning Decisions 2008. (not yet publicly available) Local involvement networks (LINks) The contents of this document are copyright © Mills & Reeve. All rights reserved. This document contains general advice and comments only and therefore specific legal advice should be taken before reliance is placed upon it in any particular circumstances. Where hyperlinks are provided to third party websites, Mills & Reeve is not responsible for the content of such sites. appendix 4 - legal advice (2) 10 Formatted: Normal