Cross-sectional Echocardiography
advertisement

Cross-sectional Echocardiography
II.
Analysis of Mathematic Models for Quantifying Volume
of the Formalin-fixed Left Ventricle
H. L. WYATT, PH.D., MING K. HENG, M.D., SAMUEL MEERBAUM, PH.D., PASCAL GUERET, M.D.,
JOHN HESTENES, PH.D., EUGENE DULA, B.S., AND ELIOT CORDAY, M.D.
SUMMARY Cross-sectional echocardiography was used to quantify volume in 21 canine left ventrides that
were fixed in formalin and immnersed in mineral oil. Area, length and diameter measurements were obtained
from short- and long-axis cross-sectional images of the left ventricle and volume was calculated by seven
mathematic models. Calculated volume was then compared, by linear regression and percent error analyses,
with fluid volume of the left ventricle, obtained by filling the chamber with a known amount of fluid. Volumes
ranged from 13-146 ml. Mathematic models using short-axis area and long-axis length gave higher correlation coefficients (r 0.982 and r = 0.969) and lower mean errors (10-20%) than standard formulas previously
used with M-mode echo and angiography. Thus, short-axis area analysis with cross-sectional echocardiography is well-suited for quantifying left ventricular volumes in dogs.
=
Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016
were compared with standard formulas for angiography and M-mode echocardiography.
ALTHOUGH several studies1'- have indicated that
left ventricular (LV) volume determined by crosssectional echocardiography in patients correlates with
angiography, true echocardiographic quantification
requires validation against an absolute standard and
study of specifically applicable models. Investigation
in this laboratory5 has shown that cross-sectional
echocardiographic measurements of left ventricular
mass in the closed-chest dog correlated well with
anatomic LV mass. Particularly good correlations
were observed with new mathematic models using
short-axis cross-sectional areas of the left ventricle.
The application of these echocardiographic models to
LV volume quantification was therefore tested in the
present study.
The plastic casts of ventricular chambers frequently
used in angiographic validation studies are not
suitable for ultrasonic visualization. In the present
study, formalin-fixed canine left ventricles served as
a known standard for comparing echocardiographic
volume determinations using mathematic models described previously.5 The echocardiographic crosssectional images of the formalin-fixed left ventricle
were similar to those available in the left ventricle of
the closed-chest dog.5 Several mathematic models
were tested, including those requiring multiple shortaxis sections and simplified reconstructions based on
double- or single-section images. These new models
Methods
Cross-sectional echocardiographic studies were performed with an electronic, phased-array sector
scanner (Varian Associates, Palo Alto, California)
with a real-time, high-resolution, 32-element transducer, an 840 sector angle and a videotape recording
rate of 30 frames/sec. The 84° sector angle enables
the recording of entire cross sections of the left ventricle, using either short- or long-axis orientations.
Twenty-one dogs were killed with an overdose of
anesthetic, their hearts removed, and the atria dissected at the atrioventricular grooves. The left ventricles were stuffed with gauze to avoid shrinkage of
the chambers and subsequently fixed in formalin for
at least 3 days. Formalin-fixed left ventricles were
immersed in mineral oil and viewed with the phasedarray sector scanner to obtain left ventricular crosssectional images similar to those described for closedchest dogs.5 Mineral oil was chosen as a medium for
this study because of its ready availability and its
similarity to castor oil, the standard medium used for
calibration procedures. The velocity of ultrasound
transmission in mineral oil is about 1.4% higher than
in aqueous solutions such as water or blood; however,
differences in ultrasound transmission velocity should
not affect myocardial boundary delineation measurements with cross-sectional echocardiography. Six to
10 short-axis cross sections were obtained from base
to apex by moving the transducer in the mineral oil
over the left ventricle. Long-axis cross sections were
obtained by rotating the transducer 900. All views
were recorded on videotape and played back later for
analysis. After the echocardiographic procedures, the
left ventricle was removed from the mineral oil, rinsed
thoroughly with water, blotted dry with paper towels,
and filled to the mitral and aortic valve rings with a
known amount of mineral oil from a graduated
cylinder. This procedure was performed three times
From the Department of Cardiology, Cedars-Sinai Medical
Center, and the Department of Medicine, UCLA School of
Medicine, Los Angeles, California.
Supported in part by grant HL-17651-04 from the NHLBI, NIH,
Bethesda, Maryland; the American Heart Association, Greater Los
Angeles Affiliate; Mrs. Anna Bing Arnold; Mrs. Lorena Mayer
Nidorf; the Jules Stein Foundation; and the Florence P. Hamilton
Foundation, Los Angeles, California. Partial support from NASA
7-100 from the California Institute of Technology Jet Propulsion
Laboratory is also acknowledged.
Address for correspondence: Dr. Eliot Corday, Cedars-Sinai
Medical Center, Halper Building, Room 301, 8700 Beverly
Boulevard, Los Angeles, California 90048.
Received February 2, 1979; revision accepted December 7, 1979.
Circulation 61, No. 6, 1980.
1119
1120
CIRCULATION
VOL 61, No 6, JUNE 1980
and an average was obtained for fluid volume of the
LV chamber. This fluid volume then provided the
known standard for comparison with echocardiographic volume measurement. Anatomic length was
measured in all ventricles by inserting a rod through
the mitral opening and measuring the distance from
the LV apex to the mitral-aortic valve junction.
Determination of LV Volume
Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016
Using cross-sectional echocardiographic images,
seven mathematic models were tested by comparing
calculated LV volume with true volume. Endocardial
outlines were traced from projections of short-axis
and long-axis cross sections during videotape stopmotion replay. Linear measurements were obtained
from the cross-sectional outlines and areas enclosed
within the outlines were derived by planimetry. Twodimensional echocardiographic short-axis images in
formalin-fixed canine ventricles are characterized by
strong circumferential echoes at the endocardial interfaces (fig. 1). By tracing at the inner border of circumferential echoes, the thickness of the endocardial
echo is excluded from endocardial area. This procedure was used to reduce potential errors. LV diameter and long-axis cross-sectional area were also
measured from the inner borders of endocardial
echoes, taken at appropriate locations. The length of
the ventricle was measured in the long-axis section
(fig. 2) as the distance from apex to the mitral ring at
the base. Seven mathematic models for quantifying
LV volume from cross-sectional echocardiographic
measurements were described in detail in the previous
quantitative study in dogs.5 The same models are used
in the present study. Volume formulas and geometric
models from which they were derived are illustrated in
figures 3A-G, along with the results.
In this study, model 1 (Simpson's rule, fig. 3A) used
the LV endocardial area (A) of six to 10 short-axis
sections from base to apex and LV length (L) from a
long-axis section. The height (h) of each short-axis
section was determined arbitrarily by dividing length
by the number of sections available. Volume was
calculated generally by summating the product A.h
for all sections. In the previous study in dogs,5 single
measurements of left ventricular short-axis diameter
and area were obtained from a section at the high
papillary muscle level for use in models 2-6 (figs.
3B-F). As a result of formalin-fixation methods in the
present study, LV geometry deviated from normal
because the LV chamber was constricted toward its
base. To avoid this constriction, a short-axis section at
the low papillary muscle region, two-thirds of the distance from base to apex, was used for diameter and
area measurements (models 2-6). Models 2-4 are
represented in figures 3B-D by the formula LVV =
K * AL, where K - I for the cylindrical geometry of
model 2, K = 2/3 for the ellipsoidal geometry of
model 3 and K = 5/6 for the half-cylinder, halfellipsoid geometry of model 4. Model 5 is represented
in figure 3E by the formula LVV = ir/6 (D1 D, L);
model 6 (fig. 3F) is the standard cube method, LVV =
0
Endocardium
m
Anterior
Lateral
B
±
Septal
Posterior
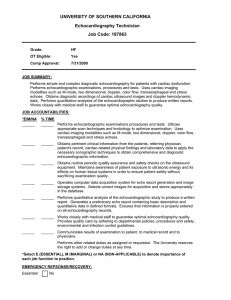
FIGURE 1. A) Polaroid photographs of typical echocardiographic short-axis images from aformalin-fixed ventricle
at the low papillary muscle level, two-thirds of the distance
from base to apex. B) A diagram of the orientation of this
left ventricular echocardiographic short-axis image.
Diameters are measured as shown, from septal to lateral
(D,) and from anterior to posterior (DJ. The approximate
endocardial border is outlined by the broken line.
D3, and model 7 (fig. 3G) is the long-axis area-length
method, LVV - 0.85 A2/L. Models 5-7 are derived
from ellipsoid geometry.
Calibration of cross-sectional echocardiographic
measurements was performed from scales along the
CROSS-SECTIONAL ECHOCARDIOGRAPHY/Wyatt et al.
1121
tion may occur with changes in gain settings and
variation in calibration may also occur over the range
of the screen. Calibrations were measured during
videotape motion replay to allow better visualization
of the scale and then applied to each volume calculation.
Data Analysis
In 21 formalin-fixed left ventricles, the chamber
volume, calculated from seven mathematic models,
Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016
was compared with the fluid volume of the left ventricle. Linear regression analysis was performed and the
standard error of estimate was calculated. For seven
models, calculated LV volume on the y-axis was
plotted against true LV volume on the x-axis (figs.
3A-G). Percent errors were determined for echocardiographic LV volume vs true LV volume according to
the following formula:
calculated LV volume - fluid LV volume X 100
fluid volume
Mean percent errors were calculated as an average of
absolute percent errors for the 21 left ventricles and
served to indicate the variability of data about the
identity line. Reproducibility of left ventricular shortaxis area and left ventricular long-axis length
measurements was assessed by determining percent
error from the average of duplicate measurements by
two observers (interobserver reproducibility); the
mean percent error was then calculated. Echocardiographic length was compared with directly measured
anatomic length for the 21 ventricles, using both linear
regression and percent error analyses.
Endocardium
Anterior
Apex
Base
B
Posterior
FIGURE 2. A) Polaroid photograph of a typical echocardiographic long-axis imagefrom aformalin-fixed left ventricle. B) A diagram of the orientation of this left ventricular
echocardiographic long-axis image. Length (L) is measured
from apex to base, as indicated. The approximate endocardial border is outlined by the broken line.
horizontal and vertical axes of the images. These
calibration scales were predetermined in the system
used (Varian, Inc.) from precise fixed-distance objects
immersed in castor oil and imaged with the echocardiographic system. The calibration, subsequently
determined in our laboratory with objects immersed in
water, was found to be accurate.
The calibration scale was remeasured for each
echocardiographic measurement because some varia-
Results
The results of testing seven mathematic models are
illustrated in figures 3A-G. Points are plotted for
calculated volume vs fluid volume in 21 left ventricles.
From a linear regression analysis of these data, a
regression equation, correlation coefficient, standard
error of estimate and mean percent error are illustrated for each model. LV volume was 13-146 ml.
Excellent correlations were observed for models using
short-axis area measurement. The multisection Simpson's rule reconstruction procedure (model 1, fig. 3A)
gave the highest correlation coefficient (0.982), the
lowest mean percent error (9.6%) and a generally even
distribution of points about the identity line, with a
regression intercept (0.7) near zero and a slope of one.
Models 2, 3 and 4 (figs. 3B-D) are based on one shortaxis section and are derived from the same basic formula: V = kAL, where k = constant, A = short-axis
LV length. These model formulas,
area and L
differing only in a constant, exhibit equally high correlation coefficients (0.969), but different mean percent errors. Of the three, model 4 has the lowest mean
percent error (17.9 ± 4.6% [± SEM]), model 3 has the
intermediate value (22.4 ± 4.7%) and model 2 has the
highest value (31.9 + 4.3%); however, the difference
between mean percent errors for models 3 and 4 was
VOL 61, No 6, JUNE 1980
CIRCULATION
1122
LVV= 2/3 AL
A
A1 A2 A3
200
+ -TT6 h3
LVV:(AiA2eA3)h+ A2h
2
(Simpson's rule)
W
re
L
A
a
y= 1.00 x - 8.9
r= 0.969
SEE= 8.6
M PE= 22.4 ± 4.7
-200
-J
LLI
0
4
0
100
-J
W4
o
-JA-
- 100
AJ
Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016
y= 1.00x - 0.7
r =0. 982
SEE= 6.6
MPE= 9.6 + 1.9
0
c
100
200
FLUID VOLUME (ml)
C)
0
A
100
200
FLUID VOLUME (ml)
LVV= 5/6 AL
LVV = AL
3j - - - 0 X3
E 200
A
A
%
-
W
-
* * //
A
0-
100
-I
L
{=1.49x- 13.4
= 0.969
C~
3EE = 12.8
MPE= 31.9 ± 4.3
W
-J
c.)
200
.
2
_j
4
100
-J
y= 1.25x -11.1
r=0.969
SEE= 10.9
MPE = 17.9 + 4.6
C-)
0
B
100
200
FLUID VOLUME (ml)
not statistically significant. Model 2 generally
overestimates LV volume, model 3 generally underestimates, and model 4 results in a relatively even distribution of points close about the identity line (figs.
3B-D). An excellent correlation coefficient (0.956)
was also obtained with model 5 (V = ir/6 [D1 D2 L]),
which uses two short-axis diameters in lieu of shortaxis area (fig. 3E). However, if only one short-axis
diameter is used and length is assumed to be twice the
diameter, as with the M-mode LV volume model 6 (V
= D,3 fig. 3F), the correlation coefficient is substantially poorer (0.828). When the angiographic formula
of model 7 (V = 0.85 AL'/L, fig. 3G) was tested using
0
D
100
200
FLUID VOLUME (ml)
long-axis area (AL) and length (L), a good correlation
coefficient resulted (r = 0.903). Only model 1 (Simpson's rule) and model 4 (half-cylinder, half-ellipsoid
geometry) showed a generally even distribution of
points close about the identity line; models 3, 5 and 7
(ellipsoid geometry) showed a generally underestimated LV volume and model 2 (cylindrical
geometry) generally overestimated LV volume.
By multiplying the formula of model 3 by 1.25, the
ellipsoid figure of model 3 was converted to the halfellipsoid, half-cylinder figure of model 4. Similarly, by
multiplying the formulas of models 5, 6 and 7 by 1.25,
the ellipsoid figures may be converted to the half-
CROSS-SECTIONAL ECHOCARDIOGRAPHY/Wyatt et al.
LVV=
r
Di
E
"
W
Di D2L
LVV =.85 A2/ L
E 200
3 L
A
L
-
200
DI
0
0
0
J
0
w
1123
a
W-4
^<100
y -0.87x 8.5
r = 0.956
SEE- 8.7
-
0
_i
4
100
y= .58x + 0.25
r= 0.903
SEE =9.5
MPE= 428 + 3.7
-J
C.)
-J
MPE= 31.4 ± 3.4
0
0
Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016
E
200
100
FLUID VOLUME (ml)
G
100
200
FLUID VOLUME (ml)
LVV = D3
11
L=2D
D
:
.
F- 200
S
W
-
J
0
W
I-
y= 1.80x - 28.0
r= 0.837
SEE = 40.4
MPE= 49.9±9.9
100
-J
CL)
_J
49
CL)
0
F
100
200
FLUID VOLUME (mi)
cylinder, half-ellipsoid figure of model 4. Correlation
coefficients are not changed by this procedure, but
mean percent errors are reduced and the distribution
of points about the identity line is improved for
models 3, 5 and 7.
Interobserver reproducibility was determined for
short-axis area, long-axis area and LV length using
linear regression and percent error analyses. For
short-axis area from 33 sections, the correlation
coefficient is 0.993 and the mean percent error is 5.5%.
For long-axis area from 15 sections, the correlation
coefficient is 0.986 and the mean percent error is 6.6%.
For LV length from 15 long-axis sections, the correla-
FIGURE 3. Comparison of volume in 21 formalin-fixed
canine left ventricles, with cross-sectional echocardiographic
quantification on the abscissa vs fluid volume on the ordinate. Geometric models and mathematic formulas are illustrated for the calculation of left ventricular volume
(L VV) from cross-sectional echocardiographic images. A =
area of either short-axis (panels A-D) or long-axis (panel G)
cross section, L = L V length, D = L V diameter. Linear
regression analyses were performed with seven models for
calculated vs fluid L VV. The identity line is shown. The
regression equation is represented by y = mx + b, MPE =
mean percent error (see text for formula). A) Serial shortaxis reconstruction by Simpson's rule (model 1). B) Single
short-axis area-length method derived from cylindrical
geometry (model 2). C) Single short-axis area-length
method derived from ellipsoid geometry (model 3). D)
Single short-axis area-length method using a half-ellipsoid,
half-cylinder geometry (model 4). E) Short-axis diameterlength method using ellipsoid geometry (model 5). F) Shortaxis diameter cube method using ellipsoid geometry (model
6). G) Long-axis area-length method using ellipsoid
geometry (model 7).
tion coefficient is 0.979 and the mean percent error is
3.0%. A comparison of LV echocardiographic length
vs anatomic length in 21 left ventricles shows a 0.912
correlation coefficient and a 7.2% mean error.
Discussion
With fluid volume of formalin-fixed left ventricles
as a standard, LV volume was accurately quantified
with cross-sectional echocardiography utilizing
mathematic models developed for closed-chest dogs.5
Although previous clinical studies1-4 of LV volume
quantification indicate good correlations for crosssectional echocardiography vs cineangiography, both
1124
CIRCULATION
Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016
techniques involve calculations based on long-axis
models of the left ventricle. Preliminary reports of
more recent in vitro studies from this6 and other
laboratories7' 8 have suggested reliable quantification
of LV volume with cross-sectional echocardiography
by comparison with directly measured LV fluid
volume.
The findings of this in vitro study on LV volume
were similar to the findings of a recent in vivo study on
LV mass by two-dimensional echocardiography in
closed-chest dogs.5 Although the strongest correlation
was obtained with model 1, excellent correlations were
also obtained with models 2-4. Models 1-4 use shortaxis areas of the left ventricle; thus models 1-4, unlike
models 5-7, do not require any assumption of shortaxis geometric symmetry because the short-axis area
incorporates endocardial irregularities due to trabeculae carnae and papillary muscle invaginations. A
very good correlation was also obtained with model 5,
but less reliable results were obtained with model 6
(cube method) and model 7 (long-axis area-length
method), probably because they require the assumption of geometric symmetry about the short axis.
Despite the generally strong correlations of all
models, only model 1 (Simpson's rule reconstruction
procedure) and model 4 (half-cylinder, half-ellipsoid
geometry) resulted in low mean percent errors and a
generally even distribution of points about the identity
line. Models 3, 5 and 7 (ellipsoid geometry) generally
underestimated the LV volume, whereas model 2
(cylindrical geometry) generally overestimated LV
volume. The fact that these findings are consistent for
studies of both volumes and mass5 of the left ventricle
lends credibility to the observation that the geometry
of the left ventricle is best represented by a halfcylinder, half-ellipsoid model5 or by a truncated ellipsoid.9 Thus, experimental quantification of LV
volumes in dogs might best be performed by either
model 1 or model 4, depending upon the nature of the
contemplated study. However, the feasibility of applying these models clinically cannot be determined from
this study.
Correlation coefficients for linear regression
analysis were slightly higher for each mathematic
model in the present study of LV volume than in the
former study of LV mass,5 probably due to the simpler
calculation of chamber volume. The only critical discrepancy between in vitro volume and in vivo mass
results was the substantial difference between correlation coefficients for model 7, the area-length method (r
= 0.903 and 0.744, respectively). The poor correlation
for LV mass by this method was probably due to the
sometimes incomplete area and length information of
in vivo long-axis sections.
Although the cross-sectional echocardiographic
techniques and models of the present in vitro study
were patterned after previous in vivo work,5 obvious
differences exist between the two applications. The
foremost of these relates to orientation of the
transducer with respect to the heart. To obtain shortaxis sections of the in vitro left ventricle, the
VOL 61, No 6, JUNE 1980
transducer is moved from base to apex in a plane
parallel to the long-axis so that the ultrasonic beams
intersect the left ventricle in a plane perpendicular to
the long-axis and the myocardial wall of the left ventricle. In contrast, for the closed-chest dog5 or the
human being, the exact orientation of the left ventricle
with respect to the transducer is not known; short-axis
sections are obtained from base to apex both by moving the transducer along the chest wall and by changing the angle of the transducer direction. Perpendicular intersection of the ultrasonic beam with the
LV long axis is judged by the circularity of the shortaxis section during late diastole.5 The exact location or
exact height for each short-axis section is not known
for in vitro or in vivo studies.
Cross-sectional images of the formalin-fixed left
ventricle are qualitatively different from those of the
beating left ventricle,5 but endocardial definition is
sharp for both preparations; this subjective judgment
is confirmed by the comparable interobserver
reproducibility for short-axis area from both studies
(mean percent error less than 6%). Qualitative
differences in endocardial outlines may result from
several factors: 1) in vitro left ventricles are not moving; 2) in vitro endocardial surfaces are smooth after
formalin fixation; and 3) the in vitro left ventricle
differs further from the beating ventricle in that the
shape of the chamber is formed by the gauze sponges
instead of by normal blood flow. Thus, the method of
filling the chamber with gauze is important in determining its shape. Because of the method used, in vitro
ventricular chambers tend to be constricted toward the
mitral and aortic valve rings, and the short-axis section at the high papillary level is not representative of
the remaining left ventricle. To avoid any constriction
toward the base of the left ventricle, a section was
chosen arbitrarily at the low papillary muscle level,
two-thirds of the distance from base to apex;
measurements from this section were then used to
compute LV volume with models 2-6. Results of this
study should be considered in light of the minor
differences in shape and texture of the in vitro vs the in
vivo left ventricle. Because of these factors, specific
regression equations for LV volume determined from
this study should not be applied to the beating heart.
Nevertheless, reliability of the mathematic models
alone for quantifying LV volume in vitro should also
be representative of the canine beating heart. Support
for this hypothesis has been demonstrated in a recent
preliminary study in this laboratory, some of the
results of which were published previously;10 quantification of LV volumes in closed-chest dogs
demonstrated very good correlations between crosssectional echocardiography and cineangiography.
In summary, results of the present study show that
LV volume may be accurately quantified in vitro by
cross-sectional echocardiography using seven mathematic models, the best of which use short-axis area
analysis. These results support and confirm similar
findings of a previous study on LV mass by crosssectional echocardiography in dogs.5
RVPEP/RVET IN VSD/Silverman et al.
Acknowledgment
We gratefully acknowledge the technical assistance of Olga
Diner, the secretarial assistance of Barbara J. Voigt, and the
assistance of Lance Laforteza in preparing the illustrations. We
thank Jeanne Bloom for her editorial assistance.
5.
6.
References
Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016
1. King DL, Jaffee CC, Schmidt DH, Ellis K: Left ventricular
volume determination by cross-sectional cardiac ultrasonography. Radiology 104: 201, 1972
2. Gehrke J, Leeman S, Raphael M, Pridie RB: Noninvasive left
ventricular volume determination by two-dimensional echocardiography. Br Heart J 37: 911, 1975
3. Schiller N, Drew D, Acquatella H, Boswell R, Botvinick E,
Greenberg B, Carlsson E: Noninvasive biplane quantitation of
left ventricular volume and ejection fraction with a real-time
two-dimensional echocardiography system. (abstr) Circulation
54 (suppl Il): II-234, 1976
4. Schiller N, Botvinick E, Cogan J, Greenberg B, Acquatella H,
Glantz S: Noninvasive methods are reliable predictors of con-
7.
8.
9.
10.
1125
trast angiographic left ventricular volumes. (abstr) Circulation
56 (suppl III): 111-221, 1977
Wyatt HL, Heng MK, Meerbaum S, Hestenes JD, Cobo JM,
Davidson RM, Corday E: Cross-sectional echocardiography. I.
Analysis of mathematic models for quantifying mass of the left
ventricle in dogs. Circulation 59: 1104, 1979
Wyatt HL, Heng MK, Meerbaum S, Davidson R, Corday E:
Evaluation of models for quantifying ventricular size by 2dimensional echocardiography. (abstr) Am J Cardiol 41: 369,
1978
Kohn MS, Schapira JW, Beaver WL, Popp RL: In vitro estimation of canine left ventricular volumes by phased array sector scan. (abstr) Clin Res 26: 244A, 1978
Eaton LW, Maughan WL, Shoukas AA, Weiss JL: Accurate
volume determination in the isolated ejecting canine left ventricle by two-dimensional echocardiography. Circulation 60: 320,
1979
Geiser EA, Bove KE: Calculation of left ventricular mass and
relative wall thickness. Arch Pathol 97: 13, 1974
Gueret P, Lang TW, Wyatt HL, Heng MK, Meerbaum S, Corday E: Validation of cross-sectional echocardiography
measurement of left ventricular volumes. Clin Res 27: 172A,
1979
Evaluation of Pulmonary Hypertension
by M-mode Echocardiography in Children
with Ventricular Septal Defect
NORMAN H. SILVERMAN, M.D., A. REBECCA SNIDER, M.D., AND ABRAHAM M. RUDOLPH, M.D.
SUMMARY We evaluated the ratio of the right ventricular preejection period to the right ventricular ejection time (RVPEP/RVET) as a predictor of pulmonary hypertension in 16 children with ventricular septal
defects (VSD) (group 1). The children ranged in age from 5 months to 18 years. The RVPEP/RVET was
measured at the time of cardiac catheterization by M-mode echocardiography from the pulmonary valve
echogram and from a simultaneously displayed pulmonary arterial pressure signal obtained with a microtip,
manometric catheter. The RVPEP/RVET measured by both methods was comparable (r = 0.91). The
RVPEP/RVET was compared with the pulmonary artery diastolic pressure (PADP) (r = 0.54). The
RVPEP/RVET ratio correlated less well with the pulmonary arterial mean pressure and pulmonary vascular
resistance.
In a second group of 51 children with VSD, echocardiographic measurement of the right ventricular systolic
time intervals was performed within 24 hours before cardiac catheterization. The same variables of pulmonary
arterial pressure as for group 1 were compared with the RVPEP/RVET ratio, and the results were similar.
These data indicate that, although there is a relationship between the RVPEP/RVET and pulmonary
hypertension, the ratio alone is not accurate enough to avoid cardiac catheterization in patients considered at
risk for pulmonary vascular disease.
PERSISTENT ELEVATION of the pulmonary
arterial pressure in children with ventricular septal
defects may lead to irreversible pulmonary vascular
disease.' Currently, the only reliable method for
detecting alterations in the pulmonary arterial
From the Department of Pediatrics and the Cardiovascular
Research Unit, University of California, San Francisco, California.
Supported by grant 6-144 from the National Foundation, March
of Dimes, White Plains, New York.
Address for correspondence: Norman H. Silverman, M.D., 1403HSE, University of California, San Francisco, California 94143.
Received October 15, 1979; revision accepted December 12, 1979.
Circulation 61, No. 6, 1980.
pressure in the course of the disease is through
repeated cardiac catheterization. Recently, M-mode
echocardiographic measurement of the ratio of the
right ventricular preejection period (RVPEP) to the
right ventricular ejection time (RVET) has been used
to detect pulmonary hypertension. The RVPEP/
RVET ratio has been reported to predict pulmonary
arterial hypertension in children with left-to-right
shunts2-4 and in infants with pulmonary hypertension
complicating noncardiac neonatal problems.5-7 If
the ratio of RVPEP/RVET accurately predicted
pulmonary arterial hypertension in children with ventricular septal defects, the need for repeated cardiac
Cross-sectional echocardiography. II. Analysis of mathematic models for quantifying
volume of the formalin-fixed left ventricle.
H L Wyatt, M K Heng, S Meerbaum, P Gueret, J Hestenes, E Dula and E Corday
Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016
Circulation. 1980;61:1119-1125
doi: 10.1161/01.CIR.61.6.1119
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1980 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on
the World Wide Web at:
http://circ.ahajournals.org/content/61/6/1119
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally
published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further
information about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/