6-Integrin Subunit Plays a Major Role in the Proangiogenic
advertisement
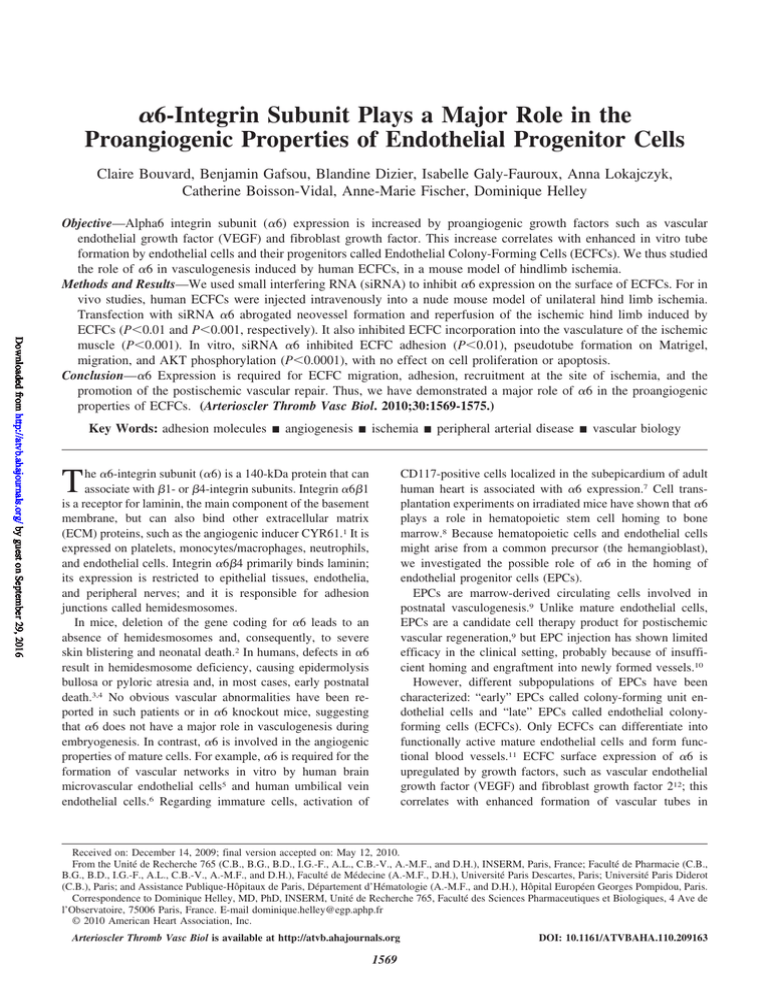
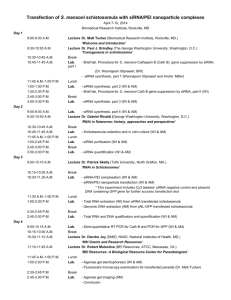
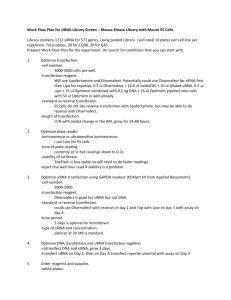
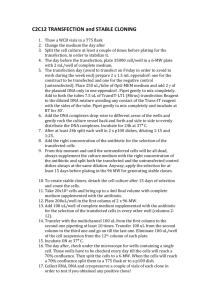
␣6-Integrin Subunit Plays a Major Role in the Proangiogenic Properties of Endothelial Progenitor Cells Claire Bouvard, Benjamin Gafsou, Blandine Dizier, Isabelle Galy-Fauroux, Anna Lokajczyk, Catherine Boisson-Vidal, Anne-Marie Fischer, Dominique Helley Downloaded from http://atvb.ahajournals.org/ by guest on September 29, 2016 Objective—Alpha6 integrin subunit (␣6) expression is increased by proangiogenic growth factors such as vascular endothelial growth factor (VEGF) and fibroblast growth factor. This increase correlates with enhanced in vitro tube formation by endothelial cells and their progenitors called Endothelial Colony-Forming Cells (ECFCs). We thus studied the role of ␣6 in vasculogenesis induced by human ECFCs, in a mouse model of hindlimb ischemia. Methods and Results—We used small interfering RNA (siRNA) to inhibit ␣6 expression on the surface of ECFCs. For in vivo studies, human ECFCs were injected intravenously into a nude mouse model of unilateral hind limb ischemia. Transfection with siRNA ␣6 abrogated neovessel formation and reperfusion of the ischemic hind limb induced by ECFCs (P⬍0.01 and P⬍0.001, respectively). It also inhibited ECFC incorporation into the vasculature of the ischemic muscle (P⬍0.001). In vitro, siRNA ␣6 inhibited ECFC adhesion (P⬍0.01), pseudotube formation on Matrigel, migration, and AKT phosphorylation (P⬍0.0001), with no effect on cell proliferation or apoptosis. Conclusion—␣6 Expression is required for ECFC migration, adhesion, recruitment at the site of ischemia, and the promotion of the postischemic vascular repair. Thus, we have demonstrated a major role of ␣6 in the proangiogenic properties of ECFCs. (Arterioscler Thromb Vasc Biol. 2010;30:1569-1575.) Key Words: adhesion molecules 䡲 angiogenesis 䡲 ischemia 䡲 peripheral arterial disease 䡲 vascular biology he ␣6-integrin subunit (␣6) is a 140-kDa protein that can associate with 1- or 4-integrin subunits. Integrin ␣61 is a receptor for laminin, the main component of the basement membrane, but can also bind other extracellular matrix (ECM) proteins, such as the angiogenic inducer CYR61.1 It is expressed on platelets, monocytes/macrophages, neutrophils, and endothelial cells. Integrin ␣64 primarily binds laminin; its expression is restricted to epithelial tissues, endothelia, and peripheral nerves; and it is responsible for adhesion junctions called hemidesmosomes. In mice, deletion of the gene coding for ␣6 leads to an absence of hemidesmosomes and, consequently, to severe skin blistering and neonatal death.2 In humans, defects in ␣6 result in hemidesmosome deficiency, causing epidermolysis bullosa or pyloric atresia and, in most cases, early postnatal death.3,4 No obvious vascular abnormalities have been reported in such patients or in ␣6 knockout mice, suggesting that ␣6 does not have a major role in vasculogenesis during embryogenesis. In contrast, ␣6 is involved in the angiogenic properties of mature cells. For example, ␣6 is required for the formation of vascular networks in vitro by human brain microvascular endothelial cells5 and human umbilical vein endothelial cells.6 Regarding immature cells, activation of T CD117-positive cells localized in the subepicardium of adult human heart is associated with ␣6 expression.7 Cell transplantation experiments on irradiated mice have shown that ␣6 plays a role in hematopoietic stem cell homing to bone marrow.8 Because hematopoietic cells and endothelial cells might arise from a common precursor (the hemangioblast), we investigated the possible role of ␣6 in the homing of endothelial progenitor cells (EPCs). EPCs are marrow-derived circulating cells involved in postnatal vasculogenesis.9 Unlike mature endothelial cells, EPCs are a candidate cell therapy product for postischemic vascular regeneration,9 but EPC injection has shown limited efficacy in the clinical setting, probably because of insufficient homing and engraftment into newly formed vessels.10 However, different subpopulations of EPCs have been characterized: “early” EPCs called colony-forming unit endothelial cells and “late” EPCs called endothelial colonyforming cells (ECFCs). Only ECFCs can differentiate into functionally active mature endothelial cells and form functional blood vessels.11 ECFC surface expression of ␣6 is upregulated by growth factors, such as vascular endothelial growth factor (VEGF) and fibroblast growth factor 212; this correlates with enhanced formation of vascular tubes in Received on: December 14, 2009; final version accepted on: May 12, 2010. From the Unité de Recherche 765 (C.B., B.G., B.D., I.G.-F., A.L., C.B.-V., A.-M.F., and D.H.), INSERM, Paris, France; Faculté de Pharmacie (C.B., B.G., B.D., I.G.-F., A.L., C.B.-V., A.-M.F., and D.H.), Faculté de Médecine (A.-M.F., D.H.), Université Paris Descartes, Paris; Université Paris Diderot (C.B.), Paris; and Assistance Publique-Hôpitaux de Paris, Département d’Hématologie (A.-M.F., and D.H.), Hôpital Européen Georges Pompidou, Paris. Correspondence to Dominique Helley, MD, PhD, INSERM, Unité de Recherche 765, Faculté des Sciences Pharmaceutiques et Biologiques, 4 Ave de l’Observatoire, 75006 Paris, France. E-mail dominique.helley@egp.aphp.fr © 2010 American Heart Association, Inc. Arterioscler Thromb Vasc Biol is available at http://atvb.ahajournals.org 1569 DOI: 10.1161/ATVBAHA.110.209163 1570 Arterioscler Thromb Vasc Biol August 2010 vitro.13 To our knowledge, the role of ␣6 expression by ECFCs in adult vasculogenesis has not been investigated. Therefore, we examined the influence of ␣6 expression on the proangiogenic properties of ECFCs and especially on its possible involvement in ECFC recruitment to sites of ischemia. We used small interfering RNA (siRNA) duplexes to inhibit ␣6 expression at the surface of human ECFCs and then examined the effect of this inhibition on adhesion, migration and pseudotube network formation in vitro, and revascularization in a nude mouse model of hind limb ischemia. Methods ECFC Isolation and Culture and RNA Interference Downloaded from http://atvb.ahajournals.org/ by guest on September 29, 2016 ECFCs were isolated, cultured, and characterized as previously described13 and as detailed in supplemental Figure I (available online at http://atvb.ahajournals.org). The ECFCs were transfected as described in the Supplemental Data. Mouse Model of Unilateral Hind Limb Ischemia All the protocols were approved by the Regional Ethics Committee on Animal Experimentation (ref P2.CBV.031.07), and all experiments conformed to European Community guidelines for the care and use of laboratory animals. Male athymic nude Foxn-1 mice (Harlan, Gannat, France), aged 7 weeks and weighing 20 to 30 g, were anesthetized by isoflurane inhalation; the left femoral artery was ligatured. Five hours after the onset of ischemia, the mice received an intravenous injection of 100 L of vehicle (PBS), 105 transfected ECFCs, or 105 untransfected ECFCs. Cells were transfected 96 hours before being injected into the animals. After 2 weeks, mice were anesthetized with pentobarbital and placed on a heating pad at 37°C; laser Doppler perfusion imaging was used to assess leg tissue perfusion, as previously described.14 The results are expressed as the ratio of perfusion in the ischemic (left) leg to perfusion in the nonischemic (right) leg. Ischemic and nonischemic gastrocnemius muscles were then collected and slowly frozen in isopentane solution cooled in liquid nitrogen, before being stored at ⫺80°C until histological analysis. Capillary Density Determination Frozen 10-m-thick sections of the distal part of the gastrocnemius muscle were fixed in ice-cold acetone for 10 minutes and incubated for 1 hour with a rat anti–mouse CD31 monoclonal antibody (clone MEC 13.3; BD Biosciences, Franklin Lakes, NJ) and with a goat anti–rat secondary antibody coupled to fluorescein isothiocyanate (Abcam, Cambridge, Mass). Sections were observed by a blinded observer (C.B.) with a confocal microscope (TCS SP2; Leica, Wetzlar, Germany). Ten fields were analyzed per section, and vessels number was quantified with computer software (Histolab; Microvision Instruments, Evry, France). The results are expressed as the ratio of the ischemic (left) leg to the nonischemic (right) leg. Histomorphometric Analysis Frozen 10-m-thick sections of ischemic gastrocnemius were fixed in acetone and stained with hematoxylin-eosin; a blinded observer (C.B.) analyzed the sections under a microscope linked to a computer. Necrotic areas were circled, and the areas of the selected surfaces were calculated with Histolab software. The results are expressed as the ratio of the necrotic surface area to the total surface area of the section. Human ECFC Detection in Mouse Muscles To evaluate ECFC incorporation into the vasculature of ischemic muscles, 1 million human ECFCs in 100 L of PBS were injected intravenously 5 hours after the onset of ischemia. Four days later, the gastrocnemius muscles were collected as previously described. To detect ECFCs, frozen tissue sections (10 m) were fixed in ice-cold acetone, immunostained with a biotinylated anti– human CD31 antibody (clone JC70A; DAKO, S-32355, Glostrup, Denmark), and incubated with streptavidin-Alexa 555 (Invitrogen, Carlsbad, Calif). The mouse vasculature was stained with a rat anti–mouse CD31 monoclonal antibody. Nuclei were stained with TOPRO3 iodide. Incorporated ECFCs were detected with a confocal microscope, and the results were expressed as the number of incorporated ECFCs per section. In Vitro Assay 72 Hours After Transfection of ECFCs Adhesion Assay Plates (with 96 wells) were coated with Matrigel, and nonspecific binding sites were saturated with BSA in PBS for 1 hour at room temperature. The wells were then washed 3 times with adhesion buffer (10-mmol/L Hepes; 140-mmol/L NaCl; 5.56 mmol/L glucose; 1% BSA; 5.4 mmol/L potassium chloride; 2 mmol/L calcium chloride; and 1 mmol/L magnesium chloride, pH 7.4) and then ECFCs suspended in adhesion buffer were distributed (30 000 cells per well). After 20 minutes at 37°C with 5% CO2, nonadherent cells were removed and the wells were washed 3 times. The number of adherent cells was determined by a p-nitrophenyl phosphate colorimetric assay. The results were normalized to the untransfected ECFC group. Migration Assay For the Boyden chamber migration assay, cell culture inserts (8.0 m pore size) were placed in 24-well plates and coated with laminin. Endothelial basal medium (EBM)-2– containing 5% FCS, with or without 40-ng/mL VEGF, was placed in the lower compartment of the Boyden chamber. ECFCs suspended in EBM-2 containing 5% FCS were placed in the upper compartment (15 000 cells per well). After 6 hours at 37°C with 5% CO2, cells adhering to the lower surface of the inserts were counted in 10 different fields per well using a microscope with a grid eyepiece. Results are expressed as the difference between experiments with and without VEGF and are normalized to the untransfected ECFC group. Matrigel Tube Formation Assay ECFCs suspended in EBM-2 containing 5% FCS were distributed (30 000 per well) on 48-well plates coated with growth factor– reduced Matrigel. They were allowed to form pseudotubes for 18 hours at 37°C with 5% CO2. The total length of the pseudotubes was quantified with computer software (Videomet; Microvision Instruments) and normalized to the untransfected ECFC control group. Proliferation Assay ECFCs were detached and seeded (10 000 per well) on 48-well laminin-coated plates (1 g/cm2). After 48 hours of proliferation, the number of cells was determined by a p-nitrophenyl phosphate colorimetric assay. The results were normalized to the untransfected ECFC group. Evaluation of AKT Phosphorylation After 96 hours of transfection with siRNA, ECFCs were detached and seeded on laminin-coated plates. One hour later, wells were washed with PBS and cells were lysed in lysis buffer (NuPAGE). Equal amounts of protein from each group were resolved by SDS-PAGE on an 8% acrylamide gel and probed by immunoblotting using anti–phosphorylated AKT and anti-AKT antibodies (Cell Signaling, Danvers, Mass). Densitometric readings were obtained using computer software (ImageJ). Results are expressed as the ratio of phosphorylated AKT to total AKT, normalized to the untransfected ECFC group. Statistical Analysis Results are expressed as mean⫾SEM of at least 3 experiments. Data were analyzed by ANOVA, followed by the Fisher protected least Bouvard et al Endothelial Progenitor Cells and ␣6-Integrin Subunit 1571 Downloaded from http://atvb.ahajournals.org/ by guest on September 29, 2016 Figure 2. Capillary density: ␣6 knockdown in ECFCs abrogates their beneficial effect in postischemic neovessel formation. Representative photomicrographs of ischemic gastrocnemius muscle sections stained for mouse CD31 and quantitative analysis of capillary density 14 days after ischemia onset. Five hours after the onset of ischemia, mice were injected intravenously with PBS (n⫽8) or with 105 cells suspended in PBS, as follows: ECFCs (n⫽6), ECFCs transfected with scramble siRNA (n⫽10), or ECFCs transfected with siRNA ␣6 (n⫽12). Data are given as mean⫾SEM. **P⬍0.01 and ***P⬍0.001. versus untransfected ECFCs and P⬍0.01 versus ECFCs transfected with scrambled siRNA) (Figure 1). Figure 1. Laser Doppler perfusion imaging: ECFC transfection with siRNA ␣6 reduces ischemic hind limb reperfusion. Representative photomicrographs and quantitative analysis of blood perfusion evaluated by laser Doppler perfusion imaging 14 days after the onset of ischemia. Five hours after the onset of ischemia, mice were injected intravenously with PBS (n⫽8) or with 105 cells suspended in PBS, as follows: ECFCs (n⫽8), ECFCs transfected with scramble siRNA (n⫽10), or ECFCs transfected with siRNA ␣6 (n⫽11). Data are given as mean⫾SEM. *P⬍0.05, **P⬍0.01 and ***P⬍0.001. significant difference post hoc test, and implemented with computer software (StatView). Differences were assumed to be significant at P⬍0.05. Results Evaluation of siRNA Efficiency and Specificity As described in the supplemental Data, siRNA ␣6 efficiently inhibited ␣6 expression (supplemental Figure II) and did not affect the expression of other integrins (supplemental Figure III). Loss of ␣6 Expression on ECFCs Reduces Postischemic Hind Limb Vascular Repair Laser Doppler Perfusion Imaging A single intravenous injection of control ECFCs (n⫽8) increased the ischemic to nonischemic leg blood flow ratio relative to PBS-treated mice by 60% (P⬍0.001). ECFCs transfected with scramble siRNA (n⫽10) also enhanced the perfusion in the ischemic hind limb, with no significant difference from untransfected ECFCs. In contrast, ECFCs transfected with siRNA ␣6 (n⫽11) did not improve reperfusion, with an ischemic to nonischemic leg blood flow ratio as low as PBS-injected mice (n⫽8). Thus, the inhibition of ␣6 expression significantly inhibited the ability of ECFCs to promote the reperfusion of the ischemic hind limb (P⬍0.001 Capillary Density A single injection of untransfected ECFCs (n⫽6) or ECFCs transfected with scramble siRNA (n⫽10) increased capillary density in the ischemic gastrocnemius muscle by a factor of 2 relative to PBS-injected mice (P⬍0.01). Once again, for the group injected with ECFCs transfected with siRNA ␣6 (n⫽12), the ratio of ischemic to nonischemic leg capillary density was as low as PBS-injected mice (n⫽8). The inhibition of ␣6 expression by the siRNA cancelled the beneficial effects of ECFCs on capillary density (P⬍0.01 versus untransfected ECFCs, and P⬍0.001 versus ECFCs transfected with scramble siRNA) (Figure 2). Histomorphometric Analysis The left gastrocnemius was more severely necrotic in animals injected with PBS (n⫽4) or with ECFCs transfected with siRNA ␣6 (n⫽6) than in animals injected with untransfected ECFCs (n⫽4) or ECFCs transfected with scramble siRNA (n⫽5). Quantitative analysis showed that the injection of ECFCs transfected with scramble siRNA and untransfected ECFCs reduced the percentage of necrotic tissue by a factor of 2 relative to the PBS-treated animals (P⬍0.05 and P⬍0.01, respectively). In contrast, ECFCs transfected with siRNA ␣6 had no beneficial effect relative to PBS-treated controls (P⬍0.001 versus untransfected ECFCs, and P⬍0.01 versus ECFCs transfected with scramble siRNA) (Figure 3). These results are in accordance with TUNEL analysis (supplemental Figure IV). Loss of ␣6 Reduces ECFC Incorporation Into the Microvasculature of Ischemic Skeletal Muscle We evaluated the number of human ECFCs (labeled red with an anti– human CD31 antibody) incorporated into the mouse microvasculature (labeled green). ECFCs were found in the ischemic leg but not in the healthy leg. siRNA ␣6 –transfected ECFCs were incorporated 5 times less efficiently than un- 1572 Arterioscler Thromb Vasc Biol August 2010 When ECFCs were transfected with siRNA ␣6, AKT phosphorylation after adhesion on laminin was reduced by 50% compared with untransfected ECFCs or ECFCs transfected with scramble siRNA (P⬍0.0001 for all) (Figure 6). Discussion Downloaded from http://atvb.ahajournals.org/ by guest on September 29, 2016 Figure 3. Histomorphometry: ␣6 knockdown in ECFCs abrogates their protective effect on necrosis. Representative hematoxylin-eosin photomicrographs and quantitative histomorphometric analysis of sections from ischemic gastrocnemius muscle 14 days after ischemia onset. Five hours after the onset of ischemia, mice were injected intravenously with PBS (n⫽4) or with 105 cells suspended in PBS, as follows: ECFCs (n⫽4), ECFCs transfected with scramble siRNA (n⫽5), or ECFCs transfected with siRNA ␣6 (n⫽6). Data are given as mean⫾SEM. *P⬍0.05, **P⬍0.01, and ***P⬍0.001. transfected ECFCs and ECFCs transfected with scramble siRNA (n⫽5 per group, P⬍0.001) (Figure 4). Loss of ␣6 Expression Reduces ECFC Adhesion to ECM The basement membrane of blood vessels damaged during ischemia may be exposed, and integrin ␣61 mediates cell attachment to laminin, the main component of the basement membrane. Therefore, we used an adhesion assay on Matrigel (61% laminin, 30% collagen IV, and 7% entactin) to study the role of ␣6 in ECFC adhesion to this substitute of basement membrane. Transfection with siRNA ␣6 reduced ECFC adhesion to Matrigel by 50% (P⬍0.01) compared with all the control groups. As expected, there was no difference between untransfected ECFCs, ECFCs treated with the transfection reagent DharmaFECT (Df) alone, and ECFCs transfected with scramble siRNA (Figure 5A). Loss of ␣6 Expression Reduces VEGF-Induced ECFC Migration In Vitro After the onset of ischemia, VEGF is released and functions as a chemoattractant to recruit cells involved in vascular repair. Therefore, we used Boyden chambers to study the role of ␣6 in ECFC migration toward VEGF. ECFCs transfected with siRNA ␣6 migrated 40 times less efficiently than untransfected ECFCs, ECFCs transfected with Df alone, and ECFCs transfected with scramble siRNA (P⬍0.0001 for all) (Figure 5B). Loss of ␣6 Expression Reduces Vascular Tube Formation by ECFCs in Matrigel and AKT Phosphorylation After ECFC Adhesion on Laminin When ECFCs were transfected with siRNA ␣6, pseudotube length was reduced 15-fold compared with all the other groups: untransfected ECFCs, ECFCs transfected with Df alone, and ECFCs transfected with scramble siRNA (P⬍0.0001 for all) (Figure 5C). siRNA ␣6 Has No Effect on ECFC Proliferation, Apopotosis or Viability Transfection with scramble siRNA or siRNA ␣6 has no significant effect on ECFC proliferation (Figure 5D), apoptosis, or viability (supplemental Figure V). This study demonstrates the importance of ␣6 in the proangiogenic properties of ECFCs. As previously reported, ECFCs injected intravenously into a nude mouse model of hind limb ischemia improved neovessel formation and reperfusion15–17 and provided protection toward necrosis. However, inhibition of ECFC cell surface ␣6 expression by using specific siRNA abrogated all these beneficial effects. To understand why the cells lacking ␣6 were unable to improve neovessel formation and reperfusion, we investigated the role of ␣6 in the homing of ECFCs, which is a key step in cell therapy. Indeed, some studies showed that soon after the injection, the major part of the cells is removed from the blood circulation and found mainly in the spleen, liver, and kidneys. Despite this loss, the remaining cells are located in the ischemic area.18 ECFCs that have been attracted there by VEGF or stromal cell derived factor (SDF)-1 can incorporate the damaged vasculature and form new blood vessels, unlike colony-forming unit endothelial cells, which promote angiogenesis only through the release of proangiogenic factors and cytokines.11 Even if it is still unclear, ECFCs may also secrete proangiogenic factors, such as placental growth factor-1 (PlGF1)17 and prostaglandin,16 which could explain why ECFC injection can increase neovessel formation even with few cells found in the ischemic area. Qian et al8 showed that ␣6 is involved in the homing of hematopoietic stem cells to bone marrow in a model of cell transplantation in irradiated mice. These researchers suggested that ␣6 contributes to hematopoietic stem cell transmigration to bone marrow because it serves as a receptor for ECM laminins, which are involved in regulating tissue organization, cell adhesion, differentiation, and migration.19 Other researchers reported that a subpopulation of mesenchymal stem cells, expressing high levels of ␣6, showed increased migration to infarcted heart in mice.20 To determine whether ␣6 is involved in the homing of ECFCs, we quantified the number of ECFCs incorporated into the vasculature of skeletal muscles 4 days after their injection, as described by Foubert et al.15 When cell surface ␣6 expression was inhibited by siRNA, the number of ECFCs integrated into the mouse microvasculature of the ischemic muscle was reduced 5-fold. To understand why the cells lacking ␣6 were not recruited and integrated to the ischemic mouse vasculature, we performed in vitro assays. After the obstruction of an artery, the oxygen supply is reduced and, therefore, the endothelial cells lining the walls of the downstream vessels undergo hypoxia. The death of these endothelial cells leaves the basement membrane partially uncovered. The integrin ␣61 is a receptor for laminin, the main component of the basement membrane. Consequently, ␣6 could be implicated in ECFC adhesion to the basement membrane of the injured blood vessels located in the ischemic area (supplemental Figure VI and supplemental Figure VII). Although other integrins or adhesion proteins are Bouvard et al Endothelial Progenitor Cells and ␣6-Integrin Subunit 1573 Downloaded from http://atvb.ahajournals.org/ by guest on September 29, 2016 Figure 4. ␣6 knockdown in ECFCs reduces their recruitment to ischemic muscles. Representative photomicrographs and quantitative analysis of human ECFC incorporation in ischemic gastrocnemius muscles 4 days after ischemia onset. ECFCs were identified with an anti– human CD31 antibody (red fluorescence). The mouse vasculature was stained with an anti–mouse CD31 antibody (green fluorescence). Nuclei were stained with TOPRO3iodide (blue). Five hours after the onset of ischemia, 5 mice per group were injected intravenously with 1 million cells suspended in PBS, as follows: ECFCs, ECFCs transfected with scramble siRNA, or ECFCs transfected with siRNA ␣6. Data are given as mean⫾SEM. ***P⬍0.001. White arrows show incorporated human ECFCs. also involved, when cell surface ␣6 expression was inhibited by siRNA, ECFC adhesion to Matrigel, a substitute of the basement membrane, was reduced by a factor of 2. Moreover, we verified that siRNA ␣6 had no effect on ECFC proliferation, apoptosis, or viability. These results suggest that the low number of ECFCs transfected with siRNA ␣6 found in the ischemic muscles was the result of poor attachment and was not a bias due to decreased cell proliferation or viability. Once endothelial progenitors have adhered, they must migrate to participate to the remodeling and to form new blood vessels. At sites of ischemia, VEGF and other angiogenic factors act as chemoattractants for cells involved in neovascularization.21 By using a Boyden chamber migration assay, we found that a lack of ␣6 expression inhibited ECFC migration induced by VEGF. These observations are in keeping with results previously obtained with other cell types. On human brain microvascular endothelial cells, ␣61 is involved in VEGF-induced adhesion, migration, and in vitro angiogenesis.5 ␣6 Overexpression on hepatocarcinoma cells leads them to acquire an invasive phenotype.22 Integrin ␣61 is necessary for matrix-dependent focal adhesion kinase (FAK) activation and, therefore, for the migration of hepatocarcinoma cells.23 It is also involved in the attachment of these cells to laminin.24 The same phenomenon has been observed in breast cancer, where ␣6 promotes carcinoma survival and progression.25,26 By using a different approach, our findings support the hypothesis that ␣6 could be involved in the mobilization and migration of the progenitors or stem cells from their niches. 1574 Arterioscler Thromb Vasc Biol August 2010 Downloaded from http://atvb.ahajournals.org/ by guest on September 29, 2016 Figure 5. Effects of ␣6 knockdown in ECFCs on adhesion, migration, vascular tube formation, and proliferation in vitro. A, Adhesion assay: cells were allowed to adhere to Matrigel for 20 minutes. The number of adherent cells was then determined by the p-nitrophenyl phosphate colorimetric assay. B, Migration assay: cells were allowed to migrate to the lower compartment of the Boyden chamber, containing 40 ng/mL VEGF for 6 hours. Cells that had migrated were stained and counted under a microscope with an eyepiece grid. C, Vascular tube formation assay: cells were allowed to form pseudotubes on Matrigel for 18 hours. Pseudotubes were stained and observed under a microscope, and their length was quantified with computer software (Videomet). D, Proliferation assay: cells were seeded on laminin-coated plates. After 48 hours of proliferation, the number of cells was determined by the p-nitrophenyl phosphate colorimetric assay. The ECFCs were transfected with siRNA ␣6, scramble siRNA, or the transfection reagent alone (Df); or they were untransfected. Seventy-two hours after transfection, cells were detached and used in 4 different assays. Data are normalized to untransfected ECFCs and are the mean⫾SEM of at least 3 different experiments. **P⬍0.01 and ****P⬍0.0001. When ECFCs are recruited to sites of ischemia, they can participate in vascular repair by either exerting paracrine effects or directly forming new blood vessels. Previous experiments with anti–␣6 antibodies have shown that ␣6 is involved in endothelial cell cord formation in vitro.6,13,27 Thus, we used the Matrigel model to examine the role of ␣6 in vessel formation. We found that ECFC transfection with siRNA ␣6 strongly inhibited vascular network formation, Figure 6. ␣6 Knockdown reduces AKT phosphorylation after adhesion on laminin. After 96 hours of transfection with siRNA, ECFCs were detached and seeded on laminin-coated plates. One hour later, cells were washed and lysed. Phoshorylated AKT and total AKT were quantified by Western blot analysis. Data are the ratio of pAKT to total AKT, are normalized to untransfected ECFCs, and are the mean⫾SEM of 3 different experiments. ****P⬍0.0001. suggesting a crucial role of ␣6 in ECM-mediated migration and differentiation and, consequently, in new blood vessel sprouting, orientation, and stabilization during angiogenesis. Also, siRNA ␣6 inhibits cordlike network formation by human breast cancer cells.28 ␣6 Is involved in ECFC adhesion, migration, and pseudotube formation. To understand why, we investigated different signaling pathways (AKT, extracellular signal regulated kinase, and p38), and we observed that AKT phosphorylation was reduced by a factor of 2, 1 hour after adhesion on laminin, when ␣6 was knocked down. This result could explain the observed cellular effects because the phosphatidylinositol 3-kinase/AKT pathway has been shown to be implicated in endothelial progenitor migration and adhesion.29,30 However, ECFCs may also promote angiogenesis via indirect effects, such as interactions with other cell types. Interestingly, ␣6 can mediate cell-cell interactions independently of laminin. For example, ␣61 has a key role in gamete fusion,31 resulting from an interaction with membrane-anchored cell surface ligands from the A Disintegrin and Metalloproteinase (ADAM) family. Interaction with ADAM-9 is also responsible for the induction of fibroblast motility.32 The role of ␣6 in ECFC interaction with other cell types should be further investigated. In conclusion, ␣6 plays a major role in the proangiogenic properties of ECFCs. ␣6 Is involved in ECFC adhesion to the basement membrane and in migration toward VEGF, explaining why this integrin subunit is required for ECFC recruitment to the site of ischemia and for the formation of vascular tube networks. A better understanding of the phenomenon involved in cell recruitment at the site of injury could allow us to find new strategies to enhance cell therapy efficiency. Regarding human cell therapy, our results suggest that enhancing ␣6 expression on ECFCs might improve their recruitment to sites of ischemia and Bouvard et al Endothelial Progenitor Cells and ␣6-Integrin Subunit promote vascular repair.33 On the other hand, ECFCs are involved in tumor angiogenesis,34 and ␣6 plays a role in both tumor angiogenesis and growth.5 Therefore, our findings support the possibility that ␣6, like other integrins, might be an interesting therapeutic target for strategies designed to disrupt tumor angiogenesis.35 Acknowledgments We thank the staff of Hôpital des Diaconesses for providing cord blood samples, Bruno Saubaméa and the imaging platform for their advice on microscopy, Françoise Grelac and Véronique Remones for their excellent technical assistance, and the staff of the Institut Médicament, Toxicologie, Chimie, Environnement animal facility. Sources of Funding C. Bouvard was supported (or paid) by a research grant from Ministère de l’Enseignement Supérieur et de la Recherche. Dr Boisson-Vidal was paid by Centre National de la Recherche Scientifique. Downloaded from http://atvb.ahajournals.org/ by guest on September 29, 2016 Disclosures None. References 1. Leu SJ, Liu Y, Chen N, Chen CC, Lam SC, Lau LF. Identification of a novel integrin alpha 6 beta 1 binding site in the angiogenic inducer CCN1 (CYR61). J Biol Chem. 2003;278:33801–33808. 2. Georges-Labouesse E, Messaddeq N, Yehia G, Cadalbert L, Dierich A, Le Meur M. Absence of integrin alpha 6 leads to epidermolysis bullosa and neonatal death in mice. Nat Genet. 1996;13:370 –373. 3. Pulkkinen L, Kimonis VE, Xu Y, Spanou EN, McLean WH, Uitto J. Homozygous alpha6 integrin mutation in junctional epidermolysis bullosa with congenital duodenal atresia. Hum Mol Genet. 1997;6:669–674. 4. Allegra M, Gagnoux-Palacios L, Gache Y, Roques S, Lestringant G, Ortonne JP, Meneguzzi G. Rapid decay of alpha6 integrin caused by a mis-sense mutation in the propeller domain results in severe junctional epidermolysis bullosa with pyloric atresia. J Invest Dermatol. 2003;121:1336–1343. 5. Lee TH, Seng S, Li H, Kennel SJ, Avraham HK, Avraham S. Integrin regulation by vascular endothelial growth factor in human brain microvascular endothelial cells: role of alpha6beta1 integrin in angiogenesis. J Biol Chem. 2006;281:40450 – 40460. 6. Chabut D, Fischer AM, Colliec-Jouault S, Laurendeau I, Matou S, Le Bonniec B, Helley D. Low molecular weight fucoidan and heparin enhance the basic fibroblast growth factor-induced tube formation of endothelial cells through heparan sulfate-dependent alpha6 overexpression. Mol Pharmacol. 2003;64:696 –702. 7. Castaldo C, Di Meglio F, Nurzynska D, Romano G, Maiello C, Bancone C, Muller P, Bohm M, Cotrufo M, Montagnani S. CD117-positive cells in adult human heart are localized in the subepicardium, and their activation is associated with laminin-1 and alpha6 integrin expression. Stem Cells. 2008;26:1723–1731. 8. Qian H, Tryggvason K, Jacobsen SE, Ekblom M. Contribution of alpha6 integrins to hematopoietic stem and progenitor cell homing to bone marrow and collaboration with alpha4 integrins. Blood. 2006;107:3503–3510. 9. Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275:964 –967. 10. Dimmeler S. ATVB in focus: novel mediators and mechanisms in angiogenesis and vasculogenesis. Arterioscler Thromb Vasc Biol. 2005;25:2245. 11. Yoder MC, Mead LE, Prater D, Krier TR, Mroueh KN, Li F, Krasich R, Temm CJ, Prchal JT, Ingram DA. Redefining endothelial progenitor cells via clonal analysis and hematopoietic stem/progenitor cell principals. Blood. 2007;109:1801–1809. 12. Smadja DM, Bieche I, Helley D, Laurendeau I, Simonin G, Muller L, Aiach M, Gaussem P. Increased VEGFR2 expression during human late endothelial progenitor cells expansion enhances in vitro angiogenesis with up-regulation of integrin alpha(6). J Cell Mol Med. 2007;11:1149–1161. 13. Zemani F, Benisvy D, Galy-Fauroux I, Lokajczyk A, Colliec-Jouault S, Uzan G, Fischer AM, Boisson-Vidal C. Low-molecular-weight fucoidan enhances the proangiogenic phenotype of endothelial progenitor cells. Biochem Pharmacol. 2005;70:1167–1175. 14. Couffinhal T, Silver M, Zheng LP, Kearney M, Witzenbichler B, Isner JM. Mouse model of angiogenesis. Am J Pathol. 1998;152:1667–1679. 1575 15. Foubert P, Matrone G, Souttou B, Lere-Dean C, Barateau V, Plouet J, Le Ricousse-Roussanne S, Levy BI, Silvestre JS, Tobelem G. Coadministration of endothelial and smooth muscle progenitor cells enhances the efficiency of proangiogenic cell-based therapy. Circ Res. 2008;103:751–760. 16. Herrler T, Leicht SF, Huber S, Hermann PC, Schwarz TM, Kopp R, Heeschen C. Prostaglandin E positively modulates endothelial progenitor cell homeostasis: an advanced treatment modality for autologous cell therapy. J Vasc Res. 2009;46:333–346. 17. Foubert P, Silvestre JS, Souttou B, Barateau V, Martin C, Ebrahimian TG, Lere-Dean C, Contreres JO, Sulpice E, Levy BI, Plouet J, Tobelem G, Le Ricousse-Roussanne S. PSGL-1-mediated activation of EphB4 increases the proangiogenic potential of endothelial progenitor cells. J Clin Invest. 2007;117:1527–1537. 18. Aicher A, Brenner W, Zuhayra M, Badorff C, Massoudi S, Assmus B, Eckey T, Henze E, Zeiher AM, Dimmeler S. Assessment of the tissue distribution of transplanted human endothelial progenitor cells by radioactive labeling. Circulation. 2003;107:2134 –2139. 19. Colognato H, Yurchenco PD. Form and function: the laminin family of heterotrimers. Dev Dyn. 2000;218:213–234. 20. Lee RH, Seo MJ, Pulin AA, Gregory CA, Ylostalo J, Prockop DJ. The CD34-like protein PODXL and alpha6-integrin (CD49f) identify early progenitor MSCs with increased clonogenicity and migration to infarcted heart in mice. Blood. 2009;113:816 – 826. 21. Asahara T, Takahashi T, Masuda H, Kalka C, Chen D, Iwaguro H, Inai Y, Silver M, Isner JM. VEGF contributes to postnatal neovascularization by mobilizing bone marrow-derived endothelial progenitor cells. Embo J. 1999; 18:3964–3972. 22. Scoazec JY, Flejou JF, D’Errico A, Fiorentino M, Zamparelli A, Bringuier AF, Feldmann G, Grigioni WF. Fibrolamellar carcinoma of the liver: composition of the extracellular matrix and expression of cell-matrix and cell-cell adhesion molecules. Hepatology. 1996;24:1128–1136. 23. Carloni V, Mazzocca A, Pantaleo P, Cordella C, Laffi G, Gentilini P. The integrin, alpha6beta1, is necessary for the matrix-dependent activation of FAK and MAP kinase and the migration of human hepatocarcinoma cells. Hepatology. 2001;34:42– 49. 24. Torimura T, Ueno T, Kin M, Ogata R, Inuzuka S, Sugawara H, Kurotatsu R, Shimada M, Yano H, Kojiro M, Tanikawa K, Sata M. Integrin alpha6beta1 plays a significant role in the attachment of hepatoma cells to laminin. J Hepatol. 1999;31:734 –740. 25. Cariati M, Naderi A, Brown JP, Smalley MJ, Pinder SE, Caldas C, Purushotham AD. Alpha-6 integrin is necessary for the tumourigenicity of a stem cell-like subpopulation within the MCF7 breast cancer cell line. Int J Cancer. 2008;122:298 –304. 26. Chung J, Mercurio AM. Contributions of the alpha6 integrins to breast carcinoma survival and progression. Mol Cells. 2004;17:203–209. 27. Davis GE, Camarillo CW. Regulation of endothelial cell morphogenesis by integrins, mechanical forces, and matrix guidance pathways. Exp Cell Res. 1995;216:113–123. 28. Klosek SK, Nakashiro K, Hara S, Goda H, Hasegawa H, Hamakawa H. CD151 regulates HGF-stimulated morphogenesis of human breast cancer cells. Biochem Biophys Res Commun. 2009;379:1097–1100. 29. Madeddu P, Kraenkel N, Barcelos LS, Siragusa M, Campagnolo P, Oikawa A, Caporali A, Herman A, Azzolino O, Barberis L, Perino A, Damilano F, Emanueli C, Hirsch E. Phosphoinositide 3-kinase gamma gene knockout impairs postischemic neovascularization and endothelial progenitor cell functions. Arterioscler Thromb Vasc Biol. 2008;28:68 –76. 30. Chavakis E, Carmona G, Urbich C, Gottig S, Henschler R, Penninger JM, Zeiher AM, Chavakis T, Dimmeler S. Phosphatidylinositol-3kinase-gamma is integral to homing functions of progenitor cells. Circ Res. 2008;102:942–949. 31. Barraud-Lange V, Naud-Barriant N, Saffar L, Gattegno L, Ducot B, Drillet AS, Bomsel M, Wolf JP, Ziyyat A. Alpha6beta1 integrin expressed by sperm is determinant in mouse fertilization. BMC Dev Biol. 2007;7:102. 32. Nath D, Slocombe PM, Webster A, Stephens PE, Docherty AJ, Murphy G. Meltrin gamma(ADAM-9) mediates cellular adhesion through alpha(6)beta(1)integrin, leading to a marked induction of fibroblast cell motility. J Cell Sci. 2000;113(pt 12):2319 –2328. 33. Chavakis E, Urbich C, Dimmeler S. Homing and engraftment of progenitor cells: a prerequisite for cell therapy. J Mol Cell Cardiol. 2008; 45:514 –522. 34. Ding YT, Kumar S, Yu DC. The role of endothelial progenitor cells in tumour vasculogenesis. Pathobiology. 2008;75:265–273. 35. Silva R, D’Amico G, Hodivala-Dilke KM, Reynolds LE. Integrins: the keys to unlocking angiogenesis. Arterioscler Thromb Vasc Biol. 2008; 28:1703–1713. Downloaded from http://atvb.ahajournals.org/ by guest on September 29, 2016 α6-Integrin Subunit Plays a Major Role in the Proangiogenic Properties of Endothelial Progenitor Cells Claire Bouvard, Benjamin Gafsou, Blandine Dizier, Isabelle Galy-Fauroux, Anna Lokajczyk, Catherine Boisson-Vidal, Anne-Marie Fischer and Dominique Helley Arterioscler Thromb Vasc Biol. 2010;30:1569-1575; originally published online May 27, 2010; doi: 10.1161/ATVBAHA.110.209163 Arteriosclerosis, Thrombosis, and Vascular Biology is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 2010 American Heart Association, Inc. All rights reserved. Print ISSN: 1079-5642. Online ISSN: 1524-4636 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://atvb.ahajournals.org/content/30/8/1569 Data Supplement (unedited) at: http://atvb.ahajournals.org/content/suppl/2010/05/27/ATVBAHA.110.209163.DC1.html Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Arteriosclerosis, Thrombosis, and Vascular Biology can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Arteriosclerosis, Thrombosis, and Vascular Biology is online at: http://atvb.ahajournals.org//subscriptions/ SUPPLEMENT MATERIAL Detailed Methods: ECFC isolation and culture Mononuclear cells were isolated from human umbilical cord blood by density gradient centrifugation as previously described.1 After an adhesion step, CD34+ cells were selected by magnetic activated cell sorting. The cells thus collected were plated on 0.2% gelatin-coated 24-well plastic culture dishes at a density of 5x105 cells/well in EGM-2 medium (Lonza, Walkersville, MD, USA). After 4 days, non adherent cells were removed and the medium was renewed. After 10 days of culture, ECFC colonies became visible microscopically. Cells were then detached with trypsine and expanded in EGM-2 on 0.2% gelatin coated plates and grown at 37°C in a humidified 5% CO2 atmosphere for further analysis. ECFC were used 25 to 45 days after cord blood processing. Characterization of ECFCs is described below. Flow cytometric characterization of ECFCs ECFCs were detached with accutase (PAA, Laboratory, Linz, Austria), washed in HBSS containing 2% FCS, resuspended at 5x106 cells/mL, and incubated with the following antibodies CD31-FITC, CD14-FITC (Becton Dickinson, Franklin Lakes, NJ, USA), CD34FITC, CD144-PE, CD146-PE, CD45-FITC, (Beckman Coulter, Fullerton, CA, USA) or an isotype control antibody from the same manufacturer. Ten thousand cells were analyzed on a FACScan flow cytometer, using CellQuest software (Becton Dickinson, Franklin Lakes, NJ, USA). 1 RNA interference ECFCs were transfected at subconfluence by using the DharmaFECT-1 transfection reagent (Dharmacon, Thermo Fisher Scientific, Lafayette, CO, USA) with pooled specific human integrin subunit siRNA (Table S1) or with a non targeting control siRNA, following the reagent manufacturer’s protocol. Briefly, 24 hours before transfection, the medium was replaced by EGM-2 without antibiotics. For transfection, the siRNA solution was mixed with the transfection reagent in EBM-2 for 20 minutes and then added to antibiotic-free EGM-2. The cell culture medium was then replaced by this mix containing 60 nM of siRNA (Table I). The medium was renewed with EBM-2/5% FCS after 24 hours and then every 48 hours. Between 72 and 96 hours after transfection, cells were detached with accutase and used in the different assays, (always 96 hours after transfection for in vivo studies). Kinetics of α6 knockdown is described in supplemental figure II. Gene expression analysis by quantitative real-time reverse-transcription polymerase chain reaction (qRT-PCR) Total RNA was isolated from ECFCs by using the RNeasy Mini Kit (Qiagen, Courtaboeuf, France) as recommended by the manufacturer. First-strand complementary DNA (cDNA) was synthesized from 1 µg of total RNA by using the High Capacity cDNA Archive kit, random primer and Superscript II reverse transcriptase (Life Technologies, Foster City, CA, USA). Alpha6 gene expression was analyzed by qRT-PCR using an ABI Prism 7900 HT Sequence Detection System (Life Technologies, Foster City, CA, USA) with SYBR green reporter dye (Life Technologies, Foster City, CA, USA). The following primers were used: 6 sense, 5'CACATCTCCTCCCTGAGCACA-3'; 6 antisense, 5'-TATATCTTGCCACCCATCCTT-3'; TBP sense, 5'-TGCACAGGAGCCAAGAGTGAA-3'; TBP antisense, 5'- TATATCTTGCCACCCATCCTT-5'. TBP, encoding the TATA box binding protein, was 2 used as the endogenous RNA control, and each sample was normalized on the basis of its TBP content. Results were normalized to non transfected ECFC control values. Flow cytometric analysis of 6 cell-surface expression At various culture times, cells were detached with Accutase (PAA Laboratory, Linz, Austria), washed in HBSS containing 2% FCS, resuspended at 5x106 cells/mL, and incubated with a PE-conjugated antibody against 6 (CD49f, clone G0H3, Becton Dickinson Biosciences, Franklin Lakes, NJ, USA) or an isotype-matched mouse irrelevant antibody from the same manufacturer. Five thousand cells were analyzed on a FACScan flow cytometer, using CellQuest software (Becton Dickinson, Franklin Lakes, NJ, USA). Results were normalized to non transfected ECFC control values. Flow cytometric analysis of CD31, CD144, v cell surface expression after transfection After 96 hours of transfection with siRNA, cells were detached with Accutase (PAA Laboratory, Linz, Austria), washed in HBSS containing 2% FCS, resuspended at 5x10 6 cells/mL, and incubated with the following antibodies CD31-FITC, CD49a-PE, CD49b-FITC, CD49c-PE, CD49e-PE, CD29-FITC, CD104-PE, CDCD51/CD61-FITC (Becton Dickinson Biosciences, Franklin Lakes, NJ, USA), CD144-PE (Beckman Coulter, Fullerton, CA, USA) or an isotype-matched mouse irrelevant antibody from the same manufacturer. Ten thousand cells were analyzed on a FACScan flow cytometer, using CellQuest software (Becton Dickinson, Franklin Lakes, NJ, USA). 3 In situ apoptosis detection on ischemic muscles sections (TUNEL assay) Frozen tissue sections (10µm) were dried, fixed in formaldehyde solution and labeled using TACSTM 2 TdT-DAB In Situ Apoptosis Detection Kit (R&D Systems, Minneapolis, MN, USA), following the manufacturer’s protocol. Evaluation of Caspase 3 activity After 96 hours of transfection with siRNA, wells were washed and the medium was changed by a serum free medium. After six hours of serum starvation, cells were washed and lysed. Lysates were then used in the Caspase 3 colorimetric assay kit (assay designs, Ann Harbor, MI, USA), following the manufacturer’s protocol. The assay was done three times in duplicate. The results were normalized to the untransfected ECFC group and represented as means + SEM of three experiments. Evaluation of cell viability After 96 hours of transfection with siRNA, dead cells present in the supernatant were collected, and living adherent cells were detached and collected. After centrifugation, the pellets were resuspended, and cell suspension was diluted in trypan blue. The number of living cells (no coloration) and dead cells (blue coloration) present in each well was quantified using a Malassez cell and a microscope. Laminin, human CD31 and mouse CD31 labeling on ischemic and non ischemic muscles Frozen tissue sections (10 µm) were fixed in ice-cold acetone, immunostained with a biotinylated anti-human CD31 antibody (clone JC70A, DAKO, Glostrup, Denmark), and incubated with streptavidin-Alexa 555 (Invitrogen, Carlsbad, CA, USA). The mouse vasculature was stained with a rat anti-mouse CD31 monoclonal antibody. And murine 4 laminin present in the muscles was stained with a rabbit anti-mouse laminin antibody. Nuclei were stained with TOPRO3 iodide. Sections were observed under a confocal microscope. 5 Supplemental Figures Figure I: Flow cytometric analysis of surface antigens on ECFCs. ECFCs were positive for CD31, CD34, CD144 and CD146 but not for monocytic markers CD45 and CD14. Isotypic control is represented in grey. The microphotograph represents ECFCs, with their characteristic cobblestone shape. 6 Figure II: Assessment of siRNA efficiency by qRT-PCR (A) and flow cytometry (B): kinetics of cell-surface 6 expression and mRNA quantification. ECFCs were cultured and transfected as described in Materials and Methods. At various times after this transfection, the quantity of 6 integrin subunit mRNA was determined by RT-PCR (A) and its protein expression at the ECFC surface was measured by flow cytometry (B). 7 Results for ECFCs transfected with DharmaFECT alone (), scramble siRNA ( ), or siRNA 6 ( ) were normalized to untransfected control ECFCs ()). Results are means ± S.E.M. of three different experiments. *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001. Neither the transfection reagent nor the scramble siRNA degraded α6 mRNA or affected α6 expression at the cell surface (no significant difference with untransfected ECFCs). The siRNA directed against α6 efficiently induced α6 mRNA degradation for at least 144 hours (Figure S2A). As a result, α6 integrin subunit expression was reduced on ECFCs transfected with siRNA α6 (about 10% of control value from 48 h to 96 h (P<0.0001) and 20% after 120 h) (Figure S2B). We thus decided to use cells 72 hours after transfection for in vitro experiments and 96 hours after transfection for in vivo experiments. 8 Figure III: siRNA α6 has no effect on CD31, CD144, v cell surface expression after 96 hours of transfection These results show that siRNA 6 are specific and that the observed effects are due to the loss of 6 and not to off-targets. 9 Figure IV: In situ apoptosis detection on ischemic muscles sections (TUNEL assay) Gastrocnemius sections (10µm) were stained using TACSTM 2 TdT-DAB In Situ Apoptosis Detection Kit. Apoptotic cells (dark brown nucleus), and necrotic cells (brown staining in the cytoplasm of enlarged cells) were more numerous in groups injected with PBS or with ECFC transfected with siRNA α6 than in groups injected with untransfected ECFCs or ECFCs transfected with scramble siRNA. Injection of ECFCs or ECFCs transfected with scramble siRNA protected tissues from apoptosis, but when α6 is knocked down, this beneficial effect is lost. 10 Figure V: siRNA α6 has no effect on ECFC apoptosis (A) or viability (B) after 96 hours of transfection. Results are mean + SEM of three different experiments. A: Apoptosis. After 96 hours of transfection, cells were serum starved for 6 hours, lysed and used in a caspase 3 colorimetric assay. 11 There is no significant difference in caspase 3 activity between the different groups (untransfected ECFCs, ECFCs transfected with scramble siRNA or ECFCs transfected with siRNA 6). This result indicates that transfection with siRNA does not influence apoptosis. B: Viability. 96 hours after transfection, dead and living cells were quantified using trypan blue. Transfection with siRNA 6 or scramble siRNA had no effect on cell viability, the number of dead and living cells was not significantly different in the different groups. As a consequence, cellular effects observed on ECFCs transfected with siRNA 6 are caused by the reduction of 6 expression and not by an increased apoptosis or a decreased viability. 12 A C B D Figure VI: expression of laminin in ischemic and non ischemic muscles Gastrocnemius sections were stained for mouse CD31 (green) and laminin (red). Laminin is a component of the basement membrane and of the extracellular matrix. Laminin is present between muscle fibers and all around blood vessels, in non ischemic muscles (A, C) as well as in ischemic muscles (B,D). 13 Figure VII: ECFCs recruited in ischemic muscles are colocalized with laminin. Human ECFCs were identified with an anti-human CD31 antibody (red fluorescence). Laminin was stained with an anti-mouse laminin antibody (green fluorescence). Nuclei were stained with TOPRO3-iodide (represented in blue). We did not find any ECFC in non ischemic muscles. In contrast, in ischemic muscles, where the basement membrane of damaged blood vessels may be exposed, ECFC are recruited and we can observe that they are colocalized with laminin. 14 Table I: SiRNA mix of human ITGA6 (ON-TARGETplus SMARTpool) Sense sequence Antisense sequence J-007214-05 GGAUCGAGUUUGAUAACGAUU 5’-P. UCGUUAUCAAACUCGAUCCUU J-007214-06 GGAUAUGCCUCCAGGUUAAUU 5’-P. UUAACCUGGAGGCAUAUCCUU J-007214-07 GAAAGGGAUUGUUCGUGUAUU 5’-P. UACACGAACAAUCCCUUUCUU J-007214-08 ACAGAUAGAUGAUAACAGAUU 5’-P. UCUGUUAUCAUCUAUCUGUUU Legends for video files Injected human ECFCs, shown in red, are incorporated into the green mouse microvasculature of the ischemic muscle and form chimeric vessels. The nuclei are represented in blue. References 1. Zemani F, Benisvy D, Galy-Fauroux I, Lokajczyk A, Colliec-Jouault S, Uzan G, Fischer AM, Boisson-Vidal C. Low-molecular-weight fucoidan enhances the proangiogenic phenotype of endothelial progenitor cells. Biochem Pharmacol. 2005;70:1167-1175. 15