Thrombolytic Therapy for Pulmonary Embolism : Frequency
advertisement

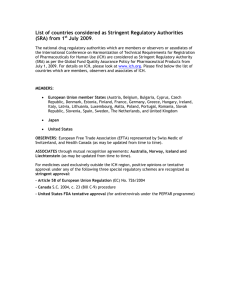
Thrombolytic Therapy for Pulmonary Embolism* Frequency of Intracranial Hemorrhage and Associated Risk Factors Daniel S. Kanter, MD; Katriina M. Mikkola; Sanjay R. Patel, MD; J. Anthony Parker, MD, PhD; and Samuel Z. Goldhaber, MD, FCCP risk factors and frequency of intracranial hemorrhage among Study objectives: To determine thefor embolism. patients undergoing thrombolysis andpulmonary controlled A analysis. Design: retrospective descriptive the United States, Canada, and Italy. Setting: Hospitalized patients at centers inembolism on perfusion scans or angiography. Patients: All had evidence of pulmonary Interventions: None. Measurements and results: Data were analyzed on 312 patients from five previously reported studies of pulmonary embolism thrombolysis. The frequency of intracranial hemorrhage up to 14 days after pulmonary embolism thrombolysis was 6 of 312 or 1.9% (95% confidence interval, 0.7 to 4.1%). Two of six intracranial hemorrhages were fatal. Two of the six patients received of the protocol because they had pre-existing, known intracranial thrombolysis in violation BP at the time of hospital admission was significantly elevated in diastolic disease. Average an who developed intracranial hemorrhage (90.3 ±15.1 mm Hg) compared with those patients who did not (77.6± 10.9 mm Hg; p=0.04). Other baseline characteristics and laboratory data were similar in both groups. Decreased level of consciousness, hemiparesis, and visual field deficits were the most common clinical signs of intracranial hemorrhage. Conclusions: Intracranial hemorrhage after pulmonary embolism thrombolysis is an infrequent but often grave complication. Meticulous patient screening before administering thrombolysis is imperative. Diastolic hypertension at the time of hospital admission is a risk factor for intracranial (CHEST 1997; 111:1241-45) hemorrhage after pulmonary embolism thrombolysis. Key words: intracranial hemorrhage; hypertension; pulmonary embolism; thrombolytic therapy DVT=deep venous thrombosis; PE=pulmonary embolism; rt-PA=recombinant tissue plasminogen activator Abbreviations: CI=confidence interval; T ntracranial hemorrhage (ICH) is one of the most serious and feared complications of thrombolysis for pulmonary embolism (PE), but only limited information exists on the frequency of its occurrence -¦" For related commentary see pages 1246 and 1410 Neurology/Neurosurgery Intensive Care Unit (Dr. Kanter), Department of Neurology (Dr. Kanter), and Cardio¬ vascular Division, Department of Medicine (Dr. Goldhaber), Brigham and Women's Hospital; the Division of Nuclear Med¬ icine (Dr. Parker), Beth Israel Hospital, Boston; Lund Univer¬ School of Medicine, Lund, Sweden (Ms. Mikkola); and sity Harvard Medical School (Drs. Kanter, Patel, Parker, and Gold¬ haber), Boston. received August 27, 1996; revision accepted Decem¬ Manuscript ber 5. Reprint requests: Samuel Z. Goldhaber, MD, FCCP, Cardiovas¬ *From the cular Division, Brigham Street, Boston, MA 02115 and Women s Hospital, 75 Francis ICH=intracranial hemorrhage; associated risk factors. Most current knowledge of ICH comes from studies in thrombolysis-related patients with myocardial infarction. However, we do not know if the same frequencies and risk factors apply to patients with PE. Therefore, we reviewed our experience in patients who have undergone PE to determine the risk factors and fre¬ thrombolysis of ICH up to 14 days after administration of quency or a thrombolytic agent. Materials and Methods Data on 312 patients from five previously reported studies17 of thrombolysis in PE (as an adjunct to heparin anticoagulation) were analyzed in an overview. The first trial was a dose selection trial of recombinant tissue plasminogen activator (rt-PA) and all 47 patients received 50 to 90 mg over 2 to 6 h.1-3 The second trial was a study of 45 patients randomized to rt-PA, 100 mg over 2 h CHEST/111 /5/MAY, 1997 Downloaded From: http://journal.publications.chestnet.org/ on 09/29/2016 1241 Table 1.Frequency Of ICH in Our Five Trials17 ICH No. Fatal Nonfatal Total 2/312 4/312 6/312 Table 2.Demographic and Historical Data for Patients Treated With Thrombolysis 95% CI 0.6 1.3 1.9 0.08-2.3 0.3-3.3 Patient Data 0.7-4.1 Mean age, yr Age<50yr, % Male:female Body weight, kg* urokinase, 2,000 Units/lb body weight, as a bolus followed by same dose per hour for up to 24 h.4 In the third trial, 90 patients were randomized to rt-PA, 100 mg over 2 h vs urokinase, 3 million units.5 The fourth trial consisted of 101 patients randomized to rt-PA, 100 mg over 2 h followed by heparin (46 patients) or heparin alone (55 patients).6 The fifth trial compared rt-PA, 100 mg over 2 h to 0.6 mg/kg (maximum 50 mg) over 15 min in 90 patients.7 All patients were given heparin infusions at the conclusion of their thrombolytic regimens. Data from six patients assigned to thrombolytic therapy who did not receive the assigned drug and from 55 patients randomized to heparin alone (in the fourth trial) were excluded from the analysis. The diagnosis of PE in all patients was based on pulmonary Prior PE/DVT, % vs History of cancer, % the angiograms or perfusion scans as described in the original reports.17 Exclusion criteria were similar in all five trials: signif¬ icant internal bleeding within the previous 6 months, intracranial disease, operation or biopsy within 10 days, occult blood on stool significant examination, impairment of hepatic thrombocytopenia, or severe renal function, pregnancy, severe or any concurrent condition likely to limit survival hypertension, to 1 anemia month. or were obtained from case report forms and hospital discharge summaries, and were entered into a database (SAS Institute Inc; Cary, NC). ICHs were confirmed by CT. ICH up to 14 days after thrombolysis w?as considered to be possibly related to thrombolytic treatment and was counted as an ICH due to thrombolysis. Continuous variables were analyzed using the Wilcoxon rank sum test. Categorical variables were examined with Fisher's Exact Test. All reported p values are two-tailed. Data Results The overall frequency of ICH was 6 of 312 or 1.9% (95% confidence interval [CI], 0.7 to 4.1%) (Table 1). Three patients died, two of ICH and one of recurrent PE or myocardial infarction, but no autop- Duration of symptoms, d Patients Patients With ICH Without ICH 68.1±8.1 57.3±17.0 0 35 0.10 1 1.20 1.00 80.2±20.6 83.3±18.8 33 30 1.00 17 18 1.00 2.7±1.9 3.7±3.3 p Valu 0.14 0.76 0.57 *Mean±SD. performed. The other three were dis¬ from chargeddeficits.the hospital with minor residual neu¬ rologic Patients with ICH were older (68.1 ±8.1 years vs 57.3±17.0 years), but this trend did not achieve statistical significance (p=0.14). No patient younger than 50 years of age suffered an ICH, and 35% of the entire cohort was in this age group. There was no gender predominance. Body weight, history of prior PE or deep venous thrombosis (DVT), known can¬ cer, and duration of symptoms were similar in patients with and without ICH (Table 2). Baseline characteristics (Table 3) revealed an ele¬ vated diastolic BP in patients who subsequently suffered an ICH (90.3±15.1 mm Hg vs 77.6±10.9 mm Hg; p^O.04). Hospital admission pulse pres¬ sures, hematocrit levels, platelet counts, and coagu¬ lation values were similar in patients with and with¬ out ICH (Table 3). None of the partial times drawn within 6 h of ICH thromboplastin were symptoms markedly elevated (>100 s) in pa¬ tients with ICH. Fibrinogen values were <200 mg/dL in two patients with ICH during the first 24 h after thrombolysis. However, average fibrinogen lev¬ els did not differ between patients with and without sies were ICH (Table 3). Table 4 shows the frequency of ICH by thrombo- Table 3.Baseline Characteristics Patients With ICH* Patients Without ICH* Characteristics (n=6) (n=306) Hospital admission systolic BP, mm Hg Hospital admission diastolic BP, mm Hgf Hospital admission pulse pressure, mm Hg 145.3±33.7 90.3±15.1 55.0±21.2 37.4±6.8 227.0±45.4 34.2±17.7 401 ±304 127.2±18.1 77.6±10.9 49.6±14.5 39.1±5.5 260.3± 105.1 41.4±37.5 364±178 Hematocrit, % Platelet count, 103/mm3 Activated partial thromboplastin time, s Fibrinogen, mg/dL* Value 0.21 0.04 0.64 0.38 0.47 0.49 0.95 Values are mean±SD. f p<0.05 on Wilcoxon rank sum test. 'Patients with ICH, n=4; patients without ICH, n=192. * 1242 Downloaded From: http://journal.publications.chestnet.org/ on 09/29/2016 Clinical Investigations Table 4.Intracranial Hemorrhages Assignment Percent of nonperfused 47 rt-PA, 50-90 mg 0 4 rt-PA, 100 mg rt-PA, 0.6 mg/kg bolus 1 (2.9) (1.7) Urokinase, 2,000 U/lb/hX24h Urokinase, 3 million units/2h 0 1 (2.2) thrombolysis rapidly 5.4 0.43 6.3 *<3=small size PE; 4-6 moderate size PE; 7-9=massive PE.9 = 45 is an infrequent but at times fatal thrombolysis The complication. presence of diastolic hypertension on hospital admission is associated with a higher risk of ICH. Younger patients appear to be at very low risk for thrombolysis-related ICH after PE. The frequency of ICH after thrombolysis for PE in our series (1.9%; 95% CI, 0.7 to 4.1%) is slightly in most studies of thrombolysis for higher thaninfarction (0.3 to 1.4%).8 The wide CIs, myocardialand small number of hemorrhages render however, direct comparisons with larger series imprecise. Two of the six ICHs occurred late (62.5 and 157 h) after and were probably due to administra¬ thrombolysis tion of heparin and not to thrombolysis. Further¬ more, the first and fifth patients (Table 5) received that actually thrombolysis in violation of the protocolknown intra¬ excluded their participation because of cranial disease (seizures and transient ischemic Discussion reverse lung Angiogram score* (0-9) 138 59 23 (Table 6). can Patients With ICH Without ICH p Value 0.22 52 41 on scan No significant differences are appar¬ lyric regimen. ent given the small number of ICHs. All hemor¬ were primarily in the rhages were lobar; noneor basal brainstem, cerebellum, ganglia (Table 5). Clinical signs of ICH included confusion or de¬ creased level of consciousness (three), hemiparesis (two), visual field deficits (two), aphasia (one), head¬ ache (one), and arm paresthesias (one). Four of the six patients had the onset of ICH within 24 h of treatment (range for completion of1.5theto thrombolytic 157 h). The size of PE based on all patients, lung scans and angiograms did not differ in patients with and without ICH PE Severity ofPE Patients Patients Without ICH Patients With ICH (< Drug Table 6.ICH and by Treatment right ventric¬ at¬ tacks). Previous studies of PE thrombolysis report only an occasional ICH.910 The introduction of CT scanning ular dysfunction and can reduce the rate of recurrent PE.6 This overview demonstrates that ICH after PE Table 5.Patient Data* Time to First History' Location of ICH Age/Sex Medical History 71/F Prior DVT; seizure; bilateral TKR Left parietal 81/M Bilateral TKR Left frontal 67/M Thyroid disease; Left occipitoparietal RHH and right parietal RHH Left occipital and small right of HTN Neurologic Symptoms Admission Symptoms After BP, mm Fibrinogen/ mg/dL PTT^ s Thrombolysis/ h Hg 110/75 Drowsiness, 121 45 Outcome Minor deficits after rehabilitation aphasia, and right-sided weakness 4-PPD 57/M Angina pectoris 64/F Alcoholism; anemia; occipital Right frontal malignant Right hemiplegia.>coma Altered mental 4,5 166/103 231 52 Death 1.5 110/70 358 26 Persistent RHH 62.5 132/88 60 Persistent RHH 157 Death due 194/101 PE status or to recurrent Ml melanoma; TIA 65/F Unknown Right temporoparietal Headache and arm 22 160/105 72 91 Death paresthesias HTN=hypertension; TKR=total knee replacement; RHH=right homonymous hemianopsia; PPD=purified protein derivative; TIA=transient attack; MI.myocardial infarction. fTime to symptoms attributed to the ICH after completion of thrombolytic infusion. * Lowest fibrinogen value in first 24 h. §Partial thromboplastin time closest to ICH symptoms (within 6 h). * ischemic CHEST/111 /5/MAY, 1997 Downloaded From: http://journal.publications.chestnet.org/ on 09/29/2016 1243 the mid-1970s allowed earlier and more accurate diagnoses of ICH which previously could be proved or at only by craniotomy autopsy. Therefore, studies done before CT scanning was available may have underestimated the frequency of ICH. The largest (to our knowledge) case series of PE thrombolysisarepatients in(since the introduction of CT scanning) listed Table 7. Only three ICHs were described in 455 patients. Combining our series with those listed in Table 7 yields an ICH frequency of 9 in 767 patients or 1.2% (95% CI, 0.5 in to 2.2%).n-17 All ICHs in our series were in lobar locations (ie, cortical regions or subcortical white matter). This is consistent with previous series of thrombolysis-re¬ lated and anticoagulant-related ICH.1820 By con¬ trast, ICH due to hypertensive small-vessel disease, which is presumably the most common cause of ICH overall, usually occurs in deep structures such as the basal ganglia, thalamus, pons, or cerebellum.21 Hence, the underlying sites of vascular rupture and mechanisms for pure hypertensive vs anticoagulation and thrombolysis-related ICH are probably differ¬ ent. However, both acute and chronic hypertension may play important contributory roles in these ICHs, since three of six of our patients had a history of and higher BPs were found on hospital hypertension, admission in those who suffered an ICH. A greater than expected frequency of systemic arterial hyper¬ tension has also been found in patients with ICH after myocardial infarction thrombolysis.22 Confusion or altered level of consciousness was seen in three of six of our patients as an initial sign of ICH. This is typical for ICH of any kind, which confusion, focal commonly produces ordrowsiness, and cowork¬ nausea. Sloan weakness, headache, in ers19 noted alteration consciousness in 65% of those with ICH in the Thrombolysis in Myocardial Infarction (TIMI) II trial. Table 7.Studies ofPE Thrombolysis in the Era of Head CT Scanning* Studv Year UKEP11 Verstraete et al12 Levine et al13 Diehl et al14 European Cooperative Study Group15 Meneveau et al16 Sors et al17 Present study Total 767 ?Overall ICH No. of Patients Receiving PE Thrombolysis 1987 1988 34 1990 33 1992 54 129 1992 63 199389 1994 53 1996 No. of Patients With ICH In the largest study (to our knowledge) of ICH after thrombolysis for myocardial infarction, clinical data and brain imaging on 268 patients with ICH were analyzed.22 Multivariate regression analysis showed that age, weight, prior cerebrovascular dis¬ ease, diastolic and systolic BP, history of hyperten¬ sion, and combined thrombolytic therapy or acceler¬ ated thrombolytic therapy were significantly associated with an increased risk of ICH. There are similar trends toward increased age, decreased and increased systolic BP in our patients with weight, ICH that might be statistically significant in a larger series. The available autopsy evidence on ICH after myocardial infarction thrombolysis demonstrates that a high proportion of these patients have cerebral amyloid angiopathy.19-23 This condition is signifi¬ cantly more common with increasing age and in¬ volves the deposition of protein with amyloid char¬ acteristics in the walls of cortical and leptomeningeal vessels. This deposition results in structural changes more brittle and susceptible to making theAn vessels association between apoprotein E e4 rupture. and cerebral amyloid angiopathy has re¬ phenotype cently been described.24 Patients with amyloid angi¬ and chronic hypertension may be at increased opathy risk for thrombolysis-related ICH. Despite increasing experience with thrombolysis, the risk of ICH in an individual patient remains defined. Diastolic hypertension increases the poorly risk of ICH after PE thrombolysis, probably in part changes in the integrity of cerebral vessels.25 through Patients with intracranial disease or diastolic hyper¬ tension should be offered thrombolysis only if the benefits of treatment outweigh the risks. Careful attention must be paid to clinical risk factors for ICH, because fibrinogen levels do not appear to provide incremental utility in assessing risk. Risk factors for ICH identified in patients with myocar¬ dial infarction may be applicable to patients with PE. Further research is necessary to clarify the underly¬ ing mechanisms for thrombolysis-related ICH. Im¬ detection of patients with vascular injury proved from hypertension or cerebral amyloid angiopathy could permit identification of individuals at high risk for developing ICH following thrombolysis. 1 Goldhaber References SZ, Vaughan DE, Markis JE, et al. Acute pulmo¬ plasminogen activator. Thrombolytic therapy of acute pulmonary embolism: current status and future potential. J Am Coll Cardiol 1987; 10:96Bnary embolism treated with tissue Lancet 1986; 2:886-89 2 312 frequency (n=767) is 1.2% (95% CI, 0.5 to 2.2%). 1244 Downloaded From: http://journal.publications.chestnet.org/ on 09/29/2016 104B 3 Goldhaber SZ, Markis JE, Kessler CM, et al. treatment Perspectives on of acute pulmonary embolism with tissue plasminClinical Investigations ogen activator. Semin Thromb Haemost 1987; 13:171-77 4 Goldhaber SZ, Kessler CM, Heit J, et al. Randomized controlled trial of recombinant tissue plasminogen activator versus urokinase in the treatment of acute pulmonary embo¬ lism. Lancet 1988; 2:293-98 5 Goldhaber SZ, Kessler CM, Heit JA, et al. Recombinanttissue-type plasminogen activator versus a novel dosing regi¬ men of urokinase in acute pulmonary embolism: a random¬ ized controlled multi-center trial. J Am Coll Cardiol 1992; 20:24-30 6 Goldhaber SZ, Haire WT>, Feldstein ML, et al. Alteplase heparin in acute pulmonary embolism: randomised trial assessing right-ventricular function and pulmonary' per¬ fusion. Lancet 1993; 341:507-11 7 Bolus Alteplase Pulmonary Embolism Group. Reduced dose bolus alteplase vs conventional alteplase infusion for pulmo¬ nary embolism thrombolysis. Chest 1994; 106:718-24 8 Levine MN, Goldhaber SZ, Gore JM, et al. Hemorrhagic complications of thrombolytic therapy in the treatment of myocardial infarction and venous thromboembolism. Chest versus 1995; 108:291S-301S 9 The Urokinase Pulmonary7 Embolism Trial. A national coop¬ erative study. Circulation 1973; 47(suppl II): 1-108 10 Urokinase Pulmonary Embolism Trial Study Group. Uroki¬ nase streptokinase embolism trial: phase II trials results. JAMA 1974; 229:1606-13 11 The UKEP Study. Multicentre trial on two local regimens of urokinase in massive pulmonary embolism. Eur Heart J 1987; 8:2-10 12 Verstraete M, Miller GAN, Bounameaux H, et al. Intravenous and intrapulmonary recombinant tissue-type plasminogen pulmonary embolism. Circulation 1988; 77:353-60 13 Levine M, Hirsh J, Weitz J, et al. A randomized trial of a single bolus dosage regimen of recombinant tissue plasmin¬ ogen activator in patients with acute pulmonary embolism. Chest 1990; 98:1473-79 14 Diehl J-L, Meyer G, Igual J, et al. Effectiveness and safety of bolus administration of alteplase in massive pulmonary em¬ bolism. Am J Cardiol 1992; 70:1477-80 activator in the treatment of massive European Cooperative Study Group for Pulmonary Embo¬ lism. Effects of intravenous urokinase versus alteplase on total pulmonary resistance in acute massive pulmonary embolism: a European multicentre double-blind trial. J Am Coll Cardiol 1992; 19:239-45 16 Meneveau N, Bassand J, Schiele F, et al. Safety of thrombo¬ lytic therapy in elderly patients with massive pulmonary embolism: a comparison with nonelderly patients. J Am Coll Cardiol 1993; 22:1075-79 17 Sors H, Pacouret G, Azarian R, et al. Hemodynamic effects of bolus vs 2-h infusion of alteplase in acute massive pulmonary7 embolism: a randomized controlled multicenter trial. Chest 1994; 106:712-17 18 Uglietta JP, O'Connor CM, Boyko OB, et al. CT patterns of intracranial hemorrhage complicating thrombolytic ther¬ apy for acute myocardial infarction. Radiology 1991; 181: 15 555-59 19 Sloan MA, Price TR, Petito CK, et al. Clinical features and pathogenesis of intracerebral hemorrhage after rt-PA and heparin therapy for acute myocardial infarction: the Throm¬ bolysis in Myocardial Infarction (TIMI) II Pilot and Random¬ ized Clinical Trial combined experience. Neurology 1995; 45:649-58 20 Kase CS, Robinson RK, Stein RW, et al. Anticoagulantrelated intracerebral hemorrhage. Neurology 1985; 35:943-48 21 Wiggins WS, Moody DM, Toole JF, et'al. Clinical and computerized tomographic study of hypertensive intracere¬ bral hemorrhage. Arch Neurol 1978; 35:832-33 22 Gore JM, Granger CB, Simoons ML, et al. Stroke after thrombolysis: mortality and functional outcomes in the GUSTO-I trial. Circulation 1995; 92:2811-18 23 Pendlebury WW, Iole ED, Tracy RP, et al. Intracerebral hemorrhage related to cerebral amyloid angiopathy and t-PA treatment. Ann Neurol 1991; 29:210-13 24 Greenberg SM, Rebeck GW, Vonsattel JP, et al. Apolipoprotein E epsilon 4 and cerebral hemorrhage associated with amyloid angiopathy. Ann Neurol 1995; 38:254-59 25 Garcia JH, Ho KL. Pathology of hypertensive arteriopathy. Clin North Am Neurosurg 1992; 3:497-507 CHEST/111 /5/MAY, 1997 Downloaded From: http://journal.publications.chestnet.org/ on 09/29/2016 1245