Patients unless specified otherwise.
advertisement

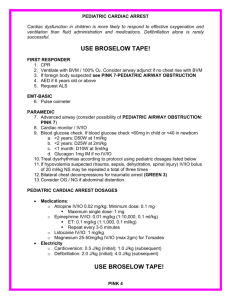
Patients < 8 years of age, unless specified otherwise. TAB 1100 PEDIATRIC PROTOCOLS TABLE OF CONTENTS Section Respiratory/Obstruction.............................................................................A Asthma.......................................................................................................B Allergy/Anaphylaxis....................................................................................C Cardiac Arrest Protocol .............................................................................D Ventricular Fibrillation ....................................................................…........E PEA (Pulseless Electrical Activity) .............................................................F Asystole .....................................................................................................G Traumatic Cardiac Arrest ...........................................................................H Hypothermic Cardiac Arrest...........................................…..........................I Bradycardia.................................................................................................J Symptomatic Tachycardia...........................................................................K Premature Ventricular Contractions (PVCs/VPBs)......................................L Deliveries and Neonatal Resuscitation .......................................................M APGAR Scores/Inverted Pyramid................................................................N Pediatric Tables ..........................................................................................O Seizures ......................................................................................................P Poisons and Overdose (Unconscious Unknown) .......................................Q Pediatric Surgical Needle Cricothyrotomy...................................................R Altered Mental Status…………………………………………………………... S Operation Safe Haven…………………………………………………………..T Pediatric Hypotension/Shock (Non-Trauma)………………………………… .U Pediatric Vomiting And Diarrhea………………………………………………. V Pediatric Multiple Trauma……………………………………………………… W Pediatric Head Trauma………… ..X …...………………………………………… Pediatric Extremity Trauma…………………………………………………… ..Y Pediatric Burns…………………………………………………………………... Z Pediatric Pain Management……………………………………………………. AA A PEDIATRIC RESPIRATORY DISTRESS History a. b. c. d. e. f. g. h. i. Sudden Gradual onset Duration Cough Fever Upper respiratory Sore throat Hoarseness Current medications Objective Findings a.. Mental status: alert, agitated, confused, somnolent, decreased level to pain b. Respiratory effort: upper airway sounds, (stridor) chest wall movement, use of accessory muscles, retractions, (depressions between ribs on inspiration) nasal flaring, substernal retractions, inherent respiratory rate c. Audible breathing noise: wheezes, cough, crowing, grunting e. Lungs by auscultation: wheezes, rales, crackles (wet sounds), diminished breath sounds f. Other findings: drooling, fever, poor skeletal muscle tone g. Skin color: cyanosis, pallor, capillary refill Specific Considerations 1. If children with croup, epiglottitis or laryngeal edema are in respiratory arrest, it is usually due to exhaustion or airway obstruction. You may still be able to ventilate or bag/valve/mask (BVM) technique. Epiglottis/Croup can become total airway obstructions quickly. Constantly monitor the airway. 2. Bag/valve/mask in small children carries the risk of excessive pressures and possible pneumothorax. It is possible to get overly excited and over ventilate. 3. In respiratory distress of sudden onset, think of foreign body aspiration. The mouth is a major sensory organ for children. The EMS Personnel must anticipate infants and children placing a multitude of obstructive hazards in their airways. 4. You may be called to attend a child who has allegedly aspirated something that was in his or her mouth, but is now asymptomatic. This child may not need emergency intervention, but should immediately be seen by a physician. Once the object has settled in the lung and is not irritating or obstructing a major airway, the child can rapidly become asymptomatic, while still requiring removal to prevent further complications. These patients require transport and skillful monitoring. Tab 1100 Pediatric Protocol A-1 Pediatric Respiratory Distress, cont. 5. Total airway obstructions that cannot be cleared by conventional methods may require surgical needle Cricothyrotomy in emergency situations. PEDIATRIC REPPRITORY DISTRESS 1. Safe scene, standard precautions 2. Put patient in position of comfort (usually upright) 3. Assess airway, breathing, circulation 4. Start oxygen therapy as indicated (assist ventilations if necessary) 5. Move patient to vehicle, contact On-Line Medical Control 6. Assist ventilation (advanced airway procedures if indicated) 7. Take vitals, pulse, respirations, capillary refill, BP, EKG, pulse oximeter use Broselow Tape to determine weight in kilograms 8. Attach pulse oximeter 9. Establish IV Normal Saline 1000ml (IO only if patient becomes unconscious, unresponsive and is in a life threatening situation). 10. Contact On-Line Medical Control with full assessment Tab 1100 Pediatric Protocol A-2 B PEDIATRIC ASTHMA History a. b. c. d. Sudden Gradual onset Duration Cough e. f. g. h. i. Lower respiratory sounds Current medications Allergies Medic alert tag Diseases Objective Findings a. Mental status: alert, agitated, confused, somnolent, decreased level to pain b. Respiratory effort: lower airway sounds, chest wall movement, use of accessory muscles, retractions (depressions between ribs on inspiration), nasal flaring, substernal retractions, inherent respiratory rate c. Audible breathing noise: wheezes, cough, grunting d. Lungs by auscultation: wheezes, rales, crackles (wet sounds), diminished breath sounds e. Other findings: drooling, poor skeletal muscle tone f. Skin color: cyanosis, pallor, capillary refill Specific Considerations 1. Wheezing is the hallmark of lower airway obstruction. Decreased, unequal, or absent breath sounds also can occur. The respiratory rate generally is rapid (although when expiration becomes prolonged, the rate may fall, an ominous sign). Bronchiolitis, asthma, and foreign body obstruction are the major diagnosis to consider. 2. Wheezing in a child with a past history or family history of allergies suggests asthma, particularly if it resolves when treated with bronchodilators. The diagnosis of asthma is difficult to make on the first episode of wheezing; consider other processes that produce wheezing, such as bronchiolitis, foreign-body aspiration, pneumonia, pulmonary edema, and some insecticide poisonings. Conversely, a known asthmatic with severe bronchospasm may have little wheezing because of poor air movement through the small airways. Forced exhalation or coughing will often accentuate the wheezing, and careful auscultation of peripheral lung fields will confirm the absence of normal breath sounds. Tab 1100 Pediatric Protocol B-1 Pediatric Asthma, cont. 2. Life-threatening complications of asthma include pneumothorax, cardiac dysrhythmias, bronchial plugging and respiratory failure. Lungs that are hyperinflated because of air trapping increase the risk of pneumothorax and pneumomediastinum. Suspect those diagnoses in a patient with decreased unilateral or bilateral aeration, in a patient with subcutaneous emphysema or in a patient who acutely decompensates. In the patient who acutely decompensates, suspect either a tension pneumothorax or pneumopericardium. PEDIATRIC ASTHMA 1. Safe scene, standard precautions. 2. Put patient in position of comfort. 3. Assess airway breathing, circulation. 4. Start oxygen therapy as indicated, assist ventilations if necessary 5. Take vitals, pulse, respirations, capillary refill, BP, EKG, pulse oximeter Use Broselow tape to determine weight in kilograms and dosing. 6. If no change or slight improvement, administer Albuterol Aerosol ½ unit dose if patient weight is <10kg. If >10kg, administer one (1) unit dose. 7. Move patient to vehicle contact On-Line Medical Control 8. If no change or slight improvement, administer Albuterol Aerosol ½ unit dose if patient weight is <10kg. If >10kg, administer one (1) unit dose. 9. If indicated, establish IV Normal Saline 1000ml using regular drip (10gtts) tubing (IO if patient becomes unconscious and unresponsive) and in life threatening situation. 10. Repeat vitals, pulse oximeter 11. Contact On-Line Medical Control 12. Vitals/ Epinephrine .01mg/kg (.01ml/kg) 1:1000 subcutaneous. Not to exceed 0.3mg. 13. Solu-Medrol 1-2 mg/Kg IV push, to maximum dose of 125 mg. Tab 1100 Pediatric Protocol B-2 C ALLERGY / ANAPHALAXIS History a. b. c. d. e. f. g. h. i. Exposure to allergens Prior reactions Onset and progression of present state Exposure to environment Toxic exposure Medications Diseases Allergies Medic alert tag k. l. m. n. o. p. q. r. s. t. Itching Wheezing Respiratory distress Nausea Weakness Abdominal cramps Chest tightness Swelling Hives Difficulty swallowing or speaking Objective Findings a. Mental status: alert, agitated, confused, somnolent, decreased level to pain b. Respiratory effort: lower airway sounds, chest wall movement, use of accessory muscles, retractions (depressions between ribs on inspiration), nasal flaring, substernal retractions, inadequate respiratory rate c. Audible breathing noise: wheezes, cough, grunting d. Lungs by auscultation: wheezes, rales, crackles (wet sounds), diminished breath sounds e. Other findings: drooling, poor skeletal muscle tone f: Skin color: cyanosis, pallor, and capillary refill Specific Considerations 1. Patients with allergic reactions can deteriorate quickly. Airway is a prime concern. Tab 1100 Pediatric Protocol C-1 Pediatric Allergy/ Anaphylaxis, cont. 2. Anxiety, tremor, palpitations, tachycardia and headache are not uncommon with the administration of Epinephrine. Symptoms with the use of Epinephrine may be particularly severe when given IV and may, in pediatric patients, induce vomiting or cause V-fib. IV Epinephrine should be a last resort. All IV Epinephrine in anaphylaxis should be the 1:10,000 concentration. 3. 4. 5. Before treating anaphylaxis, be sure your patient has objective signs as well as subjective symptoms. Hyperventilators will occasionally think they are having an allergic reaction. Epinephrine will aggravate this situation and add to their anxiety. Lethal edema may be localized to the tongue, uvula or other upper airway structures. Examine closely and be prepared to initiate advanced airway techniques early before swelling occurs. If anaphylaxis has been precipitated by either an injection of medication or insect toxin (stingers should be removed), half of the indicated Epinephrine dose may be given subcutaneous by the injection site, the rest in another extremity with a clean needle. Do not let treatment of the injection site distract you from IV treatment of life threatening anaphylaxis. Do not inject Epinephrine into the end of an organ (i.e., tip of nose, digits, penis) or face. Tab 1100 Pediatric Protocol C-2 Pediatric Allergy/ Anaphylaxis, cont. 1. Safe scene, universal precautions 2. Put patient in position of comfort 3. Assess airway, breathing, and circulation 4. Start oxygen therapy as indicated. (Assist ventilations if necessary) 5. Take vitals, pulse, respirations, capillary refill, BP, EKG, pulse oximeter. Use Broselow Tape to determine weight in kilograms 6. Attach Pulse Oximeter 7. If no change, administer Epinephrine 0.01mg/kg (0.01ml/kg) 1:1000 subcutaneous, not to exceed 0.3mg. (If unconscious due to shock, administer 0.1mg/kg 1:10000 Epinephrine IV/IO as a last resort as it may cause vomiting or V-Fib) 8. If no change and in the presence of respiratory distress, administer Albuterol aerosol ½ unit dose of if patient weight is <10kg. If >10kg, administer one (1) unit dose. 9. If no change, administer Benadryl 1mg/kg IM/IV/IO. 10. Establish IV Normal Saline 1000 ml using regular drip (10gtts) tubing. (IO if patient loses consciousness, unresponsive and in a life threatening situation). 11. Move patient to vehicle, contact On-Line Medical Control 12. Repeat set of vitals. 13 If patient displays symptoms of shock, administer fluid bolus of Normal Saline 20ml/kg IV as needed. 14. Contact On-Line Medical Control 15. Administer Solu-medrol 1-2 mg/kg IV push to max dose of 125 mg/kg Tab 1100 Pediatric Protocol C-3 D PEDIATRIC CARDIAC ARREST PROTOCOL History a. b. c. d. e. f. g. h. i. j. k l. m. n. Time of onset Bystander CPR Time lapse until CPR Preceding symptoms Underlying cause Age Diseases Medications Medical adjuncts Establish known allergies Chronic physical development Evidence of trauma Note unusual presentations Evidence of abuse, neglect or poisoning Objective Findings a. Patient totally unresponsive b. Agonal Respirations or Apnea c. Absence of pulse d. Skin temperature vs. environment e. Evidence of dependent lividity (refer to DOA Protocol Q-1, Tab 700) Specific Considerations On-Line Medical Control must be contacted no later than the point indicated in the 1. protocol. It is recommended that On-Line Medical Control be contacted early with a brief assessment so they may ready for patient. Give ETA, the situation, patient age. 2. Pediatric patients are not just “small people”. The most common cause of pediatric cardiac arrest is Hypoxia. 3. For Hypothermic cardiac arrest (Refer to Tab 1100 Protocol I.) 4. Survival from cardiac arrest is related to both BLS and ALS treatment. The EMS Personnel should make assignments so all resources are utilized to their fullest, i.e. CPR. 5. For children, intraosseous or peripheral cannulation is acceptable, whichever procedure is felt to be accomplished the quickest in life threatening situations. It should be noted, however, that if an IV is not accomplished within 90 seconds, IO should be accomplished. Patient must be unconscious and unresponsive, and in a life threatening situation to establish IO access. IO should be your initial attempt to vascular access in children less < 6 years of age in cardiac arrest. Tab 1100 Pediatric Protocol D-1 Pediatric Cardiac Arrest, cont. 6. The first EMS Personnel on scene should check effectiveness of CPR while in progress. Pay close attention to ventilatory support. 7. All pediatric cardiac arrests with advanced airways in place should have capnographic monitoring initiated after procedure (If available). 8. Medications that may be given via the endotracheal tube if no IV or IO access are: Narcan 1. Atropine concentration 8mg/20ml 2. Valium (non oil based) 3. Epinephrine – 1:1000 concentration only 4. Lidocaine (not in Fulton Co.) 5. The dosage of Epinephrine when administered into the tracheal bronchial tree should be ten (10) times the dose, otherwise given IV or IO. Lidocaine, Atropine, Narcan and Valium dosages should be doubled. Medications given endotracheally require a 5ml Saline flush followed by 5 ventilations. In the V-fib scenario where there is no IV or IO access, Lidocaine should be administered in lieu of Amiodarone. Amiodarone may not be given endotracheally. 9. Pediatric airways are small, softer and easier to obstruct or collapse. Be cautious when inserting an advanced airway. Use uncuffed tubes on pediatrics < 6 years old. 10. Respiratory reserve is small: minor insults such as improper positioning, vomitus or airway narrowing can lead to major airway problems. 11. Circulatory reserve is also small: the loss of one unit of blood is sufficient to account for severe shock or death in an infant. Conversely, 500ml of unnecessary fluid can result in acute pulmonary edema. Bolus volume replacement for shock is 20ml per kilogram. 12. Vital signs and level of consciousness are difficult to assess. History, a high index of suspicion and “soft signs” can be critical. Listen to the parents/caregivers. 13. Nutritional reserves are limited, particularly in younger infants. 14. Electrolyte solutions should always be used in pediatric IV’s or IO. (Normal Saline) 15. Pediatric equipment and drugs should be stored separately so they can be found easily when needed. 16. Procedures with poor likelihood of success or complications should be left to the hospital setting if simpler support and rapid transport will suffice to maintain the patient (advanced airway procedures, etc) 17. Emphasis should be placed on simultaneously securing the airway and rapid transport to the hospital. The EMS Personnel need to consider that moving a patient with an advanced airway in place may be more difficult than controlling the airway by less invasive methods (oral airway, BVM). Tab 1100 Pediatric Protocol D-2 Pediatric Cardiac Arrest, cont. 18. SIDS (Sudden Infant Death Syndrome) will be one of the most frequent causes of Cardiorespiratory arrest in infants between the ages of 1 month to 1 year. The parents or caretakers will have a great deal of guilt feelings. Recognizing and addressing these feelings, can help prevent some of the long-term effects of this occurrence. Unfortunately SIDS can be very hard to distinguish from child abuse. Therefore, it is important not to be judgmental or suggest a diagnosis. PEDIATRIC CARDIAC ARREST 1. Safe scene, universal precautions 2. Call for backup if needed 3. Identify rhythm and treat according to appropriate protocol Tab 1100 Pediatric Protocol D-3 E PEDIATRIC VENTRICULAR FIBRILLATION / PULSELESS VENTRICULAR TACHYCARDIA PEDIATRIC VENTRICULAR FIBRILLATION / TACHYCARDIA 1. Safe scene, standard precautions. 2. Establish unresponsiveness, apnea, and pulselessness. 3. Start CPR, move patient to vehicle, contact On-Line Medical Control 4. Apply AED or attach combo patch. Use Broselow Tape to determine weight in kilograms 5. Identify rhythm as V-fib or pulseless V-tach. 6. Defibrillate at 2J/kg, if no change. 7. Defibrillate at 4J/kg, if no change. 8. Defibrillate at 4J/kg, if no change. 9. Assists ventilations, use advanced airway maneuver if indicated, confirm bilateral breath sounds. Reconfirmation is mandated every time patient is moved. 10. Hard wire patient, monitor lead II. 11. Establish IV / IO Normal Saline using a regular drip (10gtt) tubing. Use Broselow Tape to determine weight in kilograms. 12. If no change, administer Epinephrine 0.01 mg/kg (0.1ml/kg) 1:10,000 IV/IO. Circulate with CPR. 13. If no change, defibrillate at 4J/Kg. (Within 30 seconds of medication) 14. If no change, administer Amiodarone 5mg/kg, one time dose. Circulate with CPR. 15. If no change, defibrillate at 4J/kg. (Within 30 seconds of medication) 16. Contact On-Line Medical Control and give full assessment, CPR should be maintained during this time. 17. If no change, administer Epinephrine 0.01mg/kg (0.1ml/kg) 1:10,000 IV/IO 18. Defib 4J/Kg. Tab 1100 Pediatric Protocol E-1 Pediatric, Pea, cont. 5. Identify rhythm as PEA 6. Establish IV/IO Normal Saline 250ml using regular drip (10gtt) tubing. Use Broselow tape to determine weight in kilograms. 7. Use advanced airway maneuvers if indicated. Confirm bilateral breath sounds. Reconfirmation is mandated every time patient is moved. 8. If no change, administer Epinephrine 0.01mg/kg (0.1ml/kg) 1:10,000 IV/IO. Circulate with CPR. 9. Contact On-Line Medical Control CPR should be maintained during this time. 10. If no change, administer Epinephrine 0.01mg/kg (0.1ml/kg) 1:10,000 IV/IO Tab 1100 Pediatric Protocol F-2 G PEDIATRIC ASYSTOLE PROTOCOL Asystole may be caused by many underlying factors. The following possible causes should be considered and if verified, the appropriate treatment administered prior to Epinephrine or Atropine therapy. Use the 5 H’s and 5 T’s acronym. Tab 1100 Pediatric Protocol G-1 Pediatric Asystole, cont. It is not acceptable to terminate efforts in a pre-hospital setting on pediatric once ALS has been started. The patient must be transported to closest facility and pronounced by a physician. 1. Safe scene, standard precautions. 2. Establish unresponsiveness, apnea, and pulselessness. 3. Start CPR, move patient to vehicle, contact On-Line Medical Control 4. Assist ventilations, insert advanced airway (if indicated). Confirm bilateral breath sounds. Reconfirmation is mandated every time patient is moved. 5. Apply combo patch. 6. Identify rhythm as asystole. 7. Establish IV/IO Normal Saline 250ml using regular drip (10 gtt) tubing. Use Broselow Tape to determine weight in kilograms. 8. If no change, administer Epinephrine 0.01mg/kg (0.1ml/kg) 1:10,000 IV/IO. Circulate with CPR. 9. Hard wire patient, monitor lead II. 10. Contact On-Line Medical Control, CPR should be maintained during this time. 11. If no change, administer Epinephrine 0.01mg/kg (0.1ml/kg) 1:10,000 IV/IO (repeat every 3-5 minutes) Tab 1100 Pediatric Protocol G-2 H PEDIATRIC TRAUMATIC CARDIAC ARREST For this protocol, the pediatric patient is defined as < 16 years of age and sustained a cardiac arrest from significant trauma. Special Considerations 1. The emphasis in this protocol will be to load and go. The patient should have no delay in transport after extrication, except as needed for c-spine and airway control. Consider contacting On-Line Medical Control early. 2. The receiving hospital should be given four (4) specific pieces of information: TPatient meets trauma protocol EETA AAge of patient MMechanism of injury 3. EMS Personnel should utilize other responders for extrication and other tasks (setting up IV’S in the squad during extrication) Tab 1100 Pediatric Protocol H-1 Pediatric Traumatic Arrest, cont. 1. Safe scene, standard precautions. 2. Manual c-spine control, (patient should be c-collared and backboarded with CID as soon as possible, if manual stabilization methods are inadequate). 3. Establish unresponsiveness, apnea, and pulselessness. 4. Start CPR, move patient to vehicle, contact On-Line Medical Control 5. Assist ventilations, insert advanced airway if indicated (reconfirmation of airway placement is mandated every time patient is moved) 6. Capnography monitoring will be utilized on all patients with and advanced airway in place during cardiac arrests. (If available) 7. Attach combo patch. Use Broselow Tape to determine weight in kilograms 8. V-fib/V-tach: (with no pulse) Defib at 2J/kg, no change, Defib at 4J/kg, no change, Defib at 4J/kg. (if rhythm other than V-fib/V-tach, go to #9) 9. Establish IV/IO of Normal Saline 1000ml using regular drip (10gtt) tubing. Administer a fluid bolus of 20ml/kg 10. Hard wire patient, monitor lead II. 11. EMS Personnel should contact On-Line Medical Control with full assessment, ETA and treatments done thus far. CPR should be maintained during this time. 12. If no change, administer another fluid bolus of Normal Saline 20ml/kg IV/IO. Tab 1100 Pediatric Protocol H-2 I PEDIATRIC HYPOTHERMIC CARDIAC ARREST PROTOCOL For this protocol, the pediatric patient is defined as < 8 years of age with suspected hypothermia. These are load and go patients PEIDATRIC HYPOTHERMIA ARREST 1. Safe scene, standard precautions. 2. Remove patient from environment (maintain horizontal position and avoid rough movement and excess activity). 3. Remove all wet garments. 4. Protect against heat loss and wind chill (use blankets and insulating equipment). 5. Establish unresponsiveness, apnea, and pulselessness. 6. Start CPR, move patient to vehicle, contact On-Line Medical Control 7. Attach combo patch. 8. If no pulse and V-fib/V-tach, defibrillate 2J/kg, if no change, defibrillate at 4J/kg, if no change, defibrillate at 4J/kg. (Do not administer cardiac medications). 9. Establish IV / IO Normal Saline using regular drip (10gtt ) tubing. Use Broselow Tape to determine weight in kilograms. 10. Continue warming efforts. 11. Use and an advanced airway if indicated. Confirm bilateral breath sounds. Reconfirmation is mandated every time patient is moved. 12. Hard wire patient, monitor lead II 13. Contact On-Line Medical Control Tab 1100 Pediatric Protocol I-1 J PEDIATRIC BRADYCARDIA PROTOCOL (Patient is not in cardiac arrest) Special Considerations 1. All pediatric bradyarrhythmias are to be treated with this protocol. These may include: a. Sinus Bradycardia b. First Degree AV Block c. Relative Bradycardia 2. 3. d. Absolute Bradycardia e. Second Degree Mobitz 1 (Wenckebach) f. Second Degree AV Block g. Third Degree Heart Block Treatment may not be required if patient is not symptomatic. Remember that the normal heart rates for pediatric patients are higher than that of adults. If a child’s heart rate is < 60/min, this pediatric patient needs not only ALS intervention, but chest compressions if symptomatic. The same holds true for an infant with a heart rate < 80/min. If the patient displays any of the following symptoms, treatment should be initiated: a. Shortness of Breath b. Decreased Level of Consciousness c. Hypotension d. PVC’s Hypoxemia, acidosis, and hypotension interfere with normal sinus node function and slow conduction. In addition, excessive vagal stimulation (i.e. suctioning) may produce bradycardia. Sinus bradycardia, sinus node arrest with a slow junctional or idioventricular rhythm and atrioventricular block are the most common preterminal rhythms observed in infants and children. All slow rhythms that result in instability require immediate treatment. Tab 1100 Pediatric Protocol J-1 Pediatric Bradycardia, cont. 1. Safe scene, standard precautions 2. Assess airway, breathing, circulation 3. Start oxygen therapy, as indicated (advanced airway precautions) 4. Move patient to vehicle, contact On-Line Medical Control 5. Establish IV (or IO if patient is unconscious, unresponsive and in a life threatening situation) Normal Saline using a regular drip tubing (10gtts) 6. Attach cardiac monitor and monitor lead II. 7. Identify rhythm as Bradycardia 8. Take vitals, pulse, respirations, capillary refill, BP, pulse oximeter Use Broselow Tape to determine weight in kilograms 9. If no change, administer Epinephrine 0.01mg/kg (0.1ml/kg) 1:10,000 IV (repeat every 3- 5 min) 10. Contact On-Line Medical Control 11. If no change, administer Atropine 0.02 mg/kg (minimum dose 0.1mg, maximum single dose 0.5mg child, 1.0mg adolescent) may be repeated once. 12. Transcutaneous Pacing – set rate at 100 and start 20 milliamps increasing in increments of 5 milliamps until capture. Tab 1100 Pediatric Protocol J-2 K PEDIATRIC SYMPTOMATIC TACHYCARDIA PROTOCOL (Not in cardiac arrest) All pediatric symptomatic tachycardias are to be treated with this protocol. These may include: a. Atrial Fibrillation/flutter b. Wide complex tachycardia of uncertain type c. PSVT (Paroxysmal Supraventricular Tachycardia) d. VT (Ventricular Tachycardia) e. Polymorphic Ventricular Tachycardia Defined will be symptomatic or unstable patients. Signs and symptoms are as follows: a. Shortness of breath b. c. d. e. f g. Decreased level of consciousness Hypotension Shock Pulmonary congestion Congestive heart failure Delayed capillary refill > 2 seconds Special Considerations 1. Supraventricular tachycardia (SVT) is the most common arrhythmia producing cardiovascular instability in pediatrics and it can occur throughout the pediatric years. 2. SVT in pediatrics often produces a heart rate > 220 beats per minute, but possibly as high as 300 beats per minute (infants >220, children >180). Lower heart rates may be observed in children during episodes of SVT. 3. The QRS complex is narrow in more than 90% of involved children, making differentiation between sinus tachycardia and SVT difficult. 4. Because wide-QRS SVT is relatively uncommon in infants and children, any wide-QRS tachycardia should be assumed to be of ventricular origin. 5. Although medication administration is the first choice of treatment, if any delays occur in administration of the appropriate medication, go directly to cardioversion if indicated. Caution: IO should only be established if patient meets the criteria in Tab 500 U (Intraosseeous Needle). 6. Cardiopulmonary stability during episodes of SVT is affected by the child’s age, duration of SVT, ventricular function, and ventricular rate. 7. Very rapid rates for long periods in young infants can lead to a low-output state and shock. If myocardial function is poor, SVT can produce signs of shock in a relatively short time. 8. 12-lead EKG’s are indicated on pediatrics after conversion. 9. In pediatric SVT, all possible causes should be considered and if verified, the appropriate treatment administered prior to Epinephrine or Atropine therapy. 10. Use the 5 H’s and 5 T’s acronym. Tab 1100 Pediatric Protocol K-1 Pediatric Symptomatic Tachycardia, cont. PEDIATRIC TACHYCARDIA 1. Safe scene, standard precautions. 2. Assess airway, breathing, circulation. (Take suction and advanced airway placement precautions). 3. Start oxygen therapy as indicated. (advanced airway device if indicated) 4. Move patient to vehicle, contact On-Line Medical Control 5. Establish an IV (IO if unconscious, unresponsive and in a life threatening situation) of Normal Saline using a regular drip (10gtt) tubing. 6. Attach cardiac monitor and monitor lead II. 7. Identify rhythm as tachycardia. 8. Take vitals, pulse, respirations, capillary refill, BP, pulse oximeter Use Broselow Tape to determine weight in kilograms Tab 1100 Pediatric Protocol K-2 Pediatric Symptomatic Tachycardia, cont. 9. If QRS <0.08 and P waves present, probable sinus tachycardia. Treat underlying cause (fever etc.) 10. If QRS < 0.08 and P waves absent, probable SVT. Vagal maneuvers if no change, administer Adenocard 0.1mg/kg IV (not to exceed 6mg) rapid push followed by a rapid 5ml bolus of saline. (If vascular no access available or patient unstable, go to 12). If no change, this dose may be doubled not to exceed 12mg. If no change, go to 13. 11. If QRS > 0.08, probable V-tach. (if no vascular access available or patient unstable, go to 12). Administer Amiodarone 5mg/kg over 20 to 60 minutes. Infusion will be ran at approximately 120 gtts/min. 12. If patient’s condition deteriorates, synchronized cardioversion at 0.5J/kg to 1.0J/kg. May be doubled to 2J/kg if ineffective. If sedation required, contact On-Line Medical Control first. (You may receive an order for Valium 0.2mg/kg or Versed 0.03mg/kg). 13. Contact On-Line Medical Control Tab 1100 Pediatric Protocol K-3 L PEDIATRIC PREMATURE VENTRICULAR CONTRACTIONS (PVCs)(VPBs) For this protocol, the pediatric patient is defined as < 8 years of age displaying some form of ventricular ectopy. Signs and Symptoms a. Decreased LOC b. Shortness of breath c. More than six PVC’s per minuet d. A salvos (run of PVC’s) e. Multifocal PVC’s f. R on T Special Considerations a. Patient may be better served with rapid transport and supportive measures vs. pharmacological treatment. b. Treatment may not be required for a patient who is non symptomatic. Tab 1100 Pediatric Protocol L-1 Pediatric PVC’s/ VPB’s, cont. PEDIATRIC PVC’S / VPB’S 1. Safe scene, standard precautions. 2. Reassure patient (may be helpful to put in position of comfort). 3. Assess airway, breathing, circulation. 4. Start oxygen therapy as indicated. 5. Establish IV Normal Saline using regular drip (10gtt) tubing. 6. Attach cardiac monitor and monitor lead II. Treat per appropriate protocol. 7. Take vitals, pulse, BP, respirations, pulse oximeter, EKG. 8. Repeat set of vitals, contact On-Line Medical Control, move patient to vehicle 9. Administration of an antiarrhythmic. . Tab 1100 Pediatric Protocol L-2 M DELIVERIES AND NEONATAL RESUSCITATION History of Mother a. Due date b. Prenatal care c. Previous pregnancies and problems d. Medications e. Duration of labor f. g. Foul smelling or stained amniotic fluid History of multiple births History of Infant a. If already delivered b. When was delivery c. How has infant behaved since delivery d. What has been done for infant Differential a. b. Evidence of trauma Note unusual presentations Objective Findings a. Vital signs, APGAR score at 1 and 5 minutes. (see table) b. Temperature or warmth of skin vs. environment c. Color capillary refill d. Spontaneous movement e. Meconium (brown/green/black stool fragments) in amniotic fluid f. Note time of delivery. Specific Considerations 1. Neonatal resuscitation, unlike most other resuscitation situations, requires careful attention to temperature. For neonates, the management priorities are: A- Airway B- Breathing C- Circulation T- Temperature 2. Avoid stimulation of the back of the pharynx during suctioning. This may cause bradycardia in the newborn. Do suction nares, as baby’s breath only through the nose for the first few months. In newborns, suction the mouth first. Tab 1100 Pediatric Protocol M-1 Deliveries and Neonatal Resuscitation, cont. 3. If thick meconium is present in the upper airway, or an open adequate airway cannot be obtained, use laryngoscope and suction to clear airway under direct vision to avoid contamination of the lungs with meconium as much as possible. Hypoxia and vagal stimulation can result if prolonged suctioning occurs. Do not stimulate infant to cry until airway is cleared. 4. Airway management should be kept as simple as possible. BVM use may be efficient during transport if there is only one rescuer, but chances of over ventilation (pneumothorax) or inadequate ventilation are increased. Advanced airway management should be accomplished as soon as possible, if indicated. 5. 6. Infants and particularly preemies, are very fragile. Basic stabilization with attention to airway control, suctioning, temperature conservation and CPR if indicated enroute to the hospital is recommended. Remember to watch for multiple deliveries. It is estimated that over 5 million neonatal deaths occur each year. Nearly 20% of these from asphyxia conversely nearly 1 million could be saved by simple resuscitation measures. Watch the airway. Tab 1100 Pediatric Protocol M-2 Deliveries and Neonatal Resuscitation, cont. Normal Delivery 1. Safe scene, standard precautions. 2. If baby is not delivered and head is not appearing at vaginal opening with contractions, transport and prepare to stop for delivery enroute if situation changes. Place mother in left lateral recumbent if possible, to maintain blood pressure. a. Prepare mother for delivery: 1. Put mother in position of comfort 2. Vitals 3. Start mother on oxygen 4. 5. 6. 3. Establish IV of Normal Saline Set up for delivery as precaution Contact On-Line Medical Control. If baby is not delivered, but head visible with contractions (crowning), delivery is imminent (Accomplish treatments to mother when possible) a. Contact On-Line Medical Control with assessment. b. Set up clean or sterile area for delivering baby: 1. Place sterile or clean drape between mother’s legs 2. Set sterile ties, scissors and suction on drape 3. Put on sterile gloves 4. Assign one attendant to mother, second to infant if possible. c. As infant’s head is delivering, put very gentle pressure against it to prevent an explosive delivery d. As soon as head has delivered, use bulb syringe suction to clear mouth and nares. (This should be done before delivery of the rest of infant if possible). As the neck is delivered, ensure cord is not wrapped around infant’s neck. e. Repeat suctioning immediately after delivery, also administer oxygen near face and stimulate by drying with clean towel or blanket. 4. After baby is delivered, assess general appearance: a. If infant pink, with good cry and movement (APGAR 8-10): 1. Keep in clean, dry blanket 2. Keep infant level with perineum 3. Clamp the cord in two places about 8-10 inches from infant 4. Cord may be cut between the clamps if desired. 5. Bundle infant with mother, continue to monitor 6. Transport as soon as possible and notify On-Line Medical Control b. If infant color poor, weak cry or limp (APGAR 7 or less): 1. Hold oxygen tubing near infant’s face. 2. Keep infant warm. 3. Continue to stimulate with suction and drying. Tab 1100 Pediatric Protocol M-3 Deliveries and Neonatal Resuscitation, cont. 4. 5. 6. 7. 8. 9. 10. 11. Assist ventilation with bag/valve mask with supplemental oxygen if respirations are in inadequate or heart rate < 100. Use 40-60 breaths/minute. CPR if heart rate < 60/min and unresponsive to ventilatory control. Chest compression rate 120/min (3:1 ratio). Clamp and cut cord. Transport as soon as possible and notify On-Line Medical Control. BVM may achieve adequate ventilatory support. If not, insert advanced airway en route to hospital. Establish an IV, using umbilical vein, Normal Saline using a mini gtt enroute to hospital. If no change, administer Epinephrine .01 ml/kg 1:10,000 minimum 1ml or advanced airway Transport to hospital Tab 1100 Pediatric Protocol M-4 Cry P PEDIATRIC SEIZURES History a. b. c. d. e. f. g. h. i. j. k. l. m. n. o. p. q. Time of onset Duration of seizure Description of seizure Activity Recent illness Previous seizures Medications Diseases Pupils (note size, symmetry) Rash Blood sugar level Incontinence Postictal Level of consciousness Inappropriate behavior Sweet/fruity odor Other odors Differential a. b. c. Evidence of trauma Note unusual presentations Evidence of abuse, neglect, or poisoning Objective Findings a. Mental status: alert, agitated, confused, somnolent b. Other findings: drooling, snoring, grunting c. Fever, skin temperature vs. environment d. Signs of trauma e. Skin color: cyanosis, pallor, capillary refill Specific Considerations 1. Move hazardous material away from patient. Restrain only to protect patient. Protect patient's head. Remember, always immediately check pulse after seizure stops. 2. Trauma to the tongue is unlikely to cause serious problems. Trauma to the teeth may. Attempts to force anything into patient's airway, may cause a complete obstruction. Tab 1100 Pediatric Protocol P-1 Pediatric Seizures, cont. 3. Seizures can be caused by: a. Hypoxia b. Low glucose levels c. Irritable cerebral focus d. Alcohol e. Drugs f. Fever 4. 5. Remove excess clothing if patient feels febrile. (dress lightly) If patient is obviously febrile, you may use cool, wet towels during transport. DO NOT DELAY TRANSPORT FOR COOLING. Unbundling is often sufficient. Unlike the adult with a diagnosis of Epilepsy, a child who has had a seizure, even those alert on arrival of the squad, usually requires transport. DO NOT be falsely reassured by return to normal cry. Seizures in children may not be the usual (tonic-clonic) grand mal type. A staring, peculiar eye movement, unresponsiveness or arm twitching may be the only clue. Do not make the diagnosis of "febrile seizures" in the field. This diagnosis cannot be made until other causes are excluded. If the diagnosis of meningitis is made at a later time, be sure to check with the receiving hospital concerning the need for prophylactic antibiotics for all EMS personnel. 6. 7. 8. 9. Tab 1100 Pediatric Protocol P-2 Pediatric Seizures, cont . PEDIATRIC SEIZURES 1. Safe scene, standard precautions 2. ABC (airway, breathing, circulation) 3. Oxygen 4. Move patient to vehicle, Contact On-Line Medical Control 5. If patient is ACTIVELY SEIZING, Administer Versed 0.2 mg/kg, IN via MAD (Mucosal Atomization Device), ½ should be administered into each nare. 6. Vitals (Broselow Tape), pulse oximeter 7. IV Normal Saline (blood sugar) or initiate a Saline Lock 8. < 80mg/dl, administer Dextrose 25% 1-2ml/kg IV (Draw 1-2 ml of Dextrose 50% and dilute with 1-2 ml saline) If no IV, administer Glucagon ½ unit IM. 9. Vitals 10. If BP adequate, administer Ativan 0.05-0.10mg/kg slow IV 11. Vitals 12. Contact On-Line Medical Control with full assessment 13. Administer Dextrose 25% 1-2ml/kg IV (Draw 1-2 ml of Dextrose 50% and dilute with 1-2 ml saline)(may be ordered even if blood sugar is > 80mg/dl), Tab 1100 Pediatric Protocol P-3 Q POISONS AND OVERDOSES (UNCONSCIOUS UNKNOWN) History a. b. c. d. e. f. g. h. What When How much Reason Actions of bystanders; i.e. induced vomiting Diseases Medications Establish known allergies Differential a. b. c. Evidence of trauma Evidence of drug ingestion Note unusual presentations Objective Findings a. Mental status, alert, confused, lethargic b. Patient totally unresponsive c. Skin temperature vs. environment d. Appropriate actions e. Sweet/fruity odor f. Unusual odor g. Medic alert tags Specific Considerations 1. All empty containers of ingested material should accompany patient to hospital. All emesis Should be saved. Any questionable material should be taken to emergency department; i.e.: empty vials. 2. Pay particular attention to: a. Increased salivation b. Soot or burns in mouth c. Irritation of the eyes d. Sweating and skin burns e. Lung findings; i.e.: edema f. Arrhythmias g. Capillary refill Tab 1100 Pediatric Protocol Q-1 Pediatric Seizures, cont. 3. . Antidotes a. b. c. d. Product labels and home kits may be misleading and dangerous. Watch the ABCs. Do not neutralize acids with alkali. Do not neutralize alkali with acid. With hydrocarbon ingestion, do not induce vomiting, unless poison e. f. g. 4. 5. dissolved in hydrocarbon. Gasoline should be flushed from trauma victims and is often overlooked. Protect yourself in inhalation poisoning incidents. Do not induce vomiting in the following patients who have ingested: a. Strong base acids b. Silver nitrate c. Strychnine d. Who are not alert External Contamination ( See Infection Control Protocol 300 I-1) Tab 1100 Pediatric Protocol Q-2 Pediatric Seizures, cont. PEDIATRIC POISONS AND OVERDOSE (UNCONCIOUS UNKNOWN) INTERNAL CONTAMINATION 1. Safe scene, standard precautions. 2. Establish responsiveness 3. Reassure patient (explain procedures) 4. Evaluate airway, take appropriate action. (insert advanced airway en route to hospital if indicated) 5. Take vitals; pulse, respirations, capillary refill, BP, EKG Use Broselow Tape to determine weight in kilograms 6. Attach Pulse oximeter 7. Attach Cardiac monitor (treat per appropriate protocol). 8. Administer high flow oxygen using a non-rebreather mask 9. Move patient to vehicle,contact On-Line Medical Control 10. IV Normal Saline 250ml (test blood sugar) 11. 12. Blood sugar < 80mg/dl, administer Dextrose 25% 1-2ml/kg IV. (Draw 1-2ml/kg Dextrose 50% and dilute with equal ml saline) Blood sugar > 80mg/dl, go to 13. If no IV and blood sugar < 80mg/dl, administer Glucagon ½ unit IM. Recommended Dextrose concentrations and dosing are: a. Neonate: 1-2mL/Kg 12.5% Dextrose b. < 2 years: 1-2mL/Kg 25% Dextrose c. > 2 years: 1-2mL/Kg 50% Dextrose (Draw dosage of 50% Dextrose and dilute with equal ml of saline) Vitals 13. Narcan 0.1mg/kg IV or IN, (over 5 years, 2mg) 14. Contact On-Line Medical Control 15. Dextrose 25% 1-2ml/kg IV (Draw 1-2 ml/kg Dextrose 50% and dilute with equal ml saline) Tab 1100 Pediatric Protocol Q-3 Pediatric Seizures, cont. 16. This patient should be transported in the lateral recumbent position with a close watch on the airway. (If trauma situation suspected, use full c-spine precautions). Tab 1100 Pediatric Protocol Q-4 R PEDIATRIC SURGICAL NEEDLE CRICOTHYROTOMY CONSIDERATIONS: Under most circumstances an adequate airway is provided by repositioning of the head and jaw, an oropharyngeal airway, or advanced airway maneuvers. Rarely a child with an upper airway foreign body, severe oral/facial injuries, anaphylaxis or a laryngeal fracture will require this procedure. THIS PROCEDURE IS TO BE USED ONLY IN A CHILD WHO HAS A TOTALLY OBSTRUCTED AIRWAY IN WHOM ALL OTHER EFFORTS HAVE FAILED. Equipment Needed a. b. c. d e. f. 1-1/4" 14ga. IV catheter w/flexible over the needle catheter pediatric ambu bag 20" IV extension set 3ml syringe 15mm adapter from 2.5 or 3.0 pediatric endotracheal tube Providine iodine preps Complications of the Surgical Cricothyrotomy are a. Incorrect placement missing the airway b. Asphyxia c. Aspiration d. Creation of a false passage into the tissues f. Subglottic stenosis or edema g. Laryngeal stenosis or trauma h. Hemorrhage h. Laceration of esophagus j. Laceration of the trachea k. Mediastinal emphysema l. Vocal cord trauma or paralysis m. Delayed soft tissue infection Tab 1100 Pediatric Protocol R-1 Pediatric Surgical Cricothyrotomy, cont. PEDIATRIC SURGICAL NEEDLE CRICOTHYROTOMY CONSIDERATIONS: 1. Safe scene, standard precautions. 2. Try to establish an airway using less invasive airway maneuvers. 3. Patient must be in supine position with neck in a neutral position, c-spine control if indicated. 4. Palpate the cricothyroid membrane anteriorly, between the thyroid cartilage and cricoid cartilage. If time allows, prep the area with betadine swabs. 5. Use a 1-1/4” #14 gauge needle, 3ml syringe attached. Puncture the skin midline and directly over the cricothyroid membrane. 6. Direct the needle at 45º angle distally. Insert the needle through the lower half of the cricothyroid membrane. Aspiration of air confirms entry into the tracheal lumen. 7. Remove the syringe and withdraw the metal stylet while advancing the synthetic catheter distally. 8. Attach the catheter hub to the IV extension tubing, attach the 15mm adapter to the proximal end of the extension tubing and then to the pediatric ambu device. Ventilate. 9. Auscultate chest for adequate ventilation. 10. The catheter should be held by hand until the airway is turned over to the hospital staff. You should maintain a grip on the catheter at all times during transport to avoid dislodging. Different methods of taping and immobilization of the catheter may be necessary depending on circumstances, but under no situations should the paramedic relinquish their grip on the surgical airway catheter. 11. Make sure the systems attached to Auto Vent or 100% oxygen using a pediatric ambu bag. Tab 1100 Pediatric Protocol R-2 S Pediatric Altered Mental Status For this protocol, the pediatric patient is defined as < 16 years of age. History A. B. C. D. E. F. Known diabetic, medic alert tag? Drugs, drug paraphernalia? Repot of illicit drug use or toxic ingestion? Past medical History. Medications. History of trauma? Objective Findings A. Decreased mental status B. Change in baseline mental status C. Bizarre behavior D. E. Hypoglycemia Hyperglycemia Specific Considerations 1. Be aware of altered mental status as a presenting sign of an environmental toxin or Haz-Mat exposure and protect personal safety. 2. It is safer to assume hypoglycemia than hyperglycemia if doubt exists. Recheck BGL after therapy with IV dextrose or IN / IM Glucagon. 3. Do not give oral glucose to a patient who cannot protect their own airway. 4. Consider restraints, if necessary, for patient’s and/or rescuer’s protection. 5. The following Dextrose concentrations and dosing are recommended: a. Neonate: 1-2 mL/Kg 12.5% Dextrose b. < 2: 1-2 mL/Kg 25% Dextrose c. > 2: 1-2 mL/Kg 50% Dextrose (Draw dosage of Dextrose 50% and dilute with equal ml of saline) 6. Maximum Dextrose administration is 50mL of age-appropriate concentration. Additional amounts must be authorized by On-Line Medical Control. 7. For symptomatic patients with low BGL values, and absent intravenous access, administer Glucagon IN / IM (0.5mg < 25Kg; 1.0mg > 25Kg). Maximum dose of Glucagon is 1mg. 8. Maximum Narcan dose is 2.0mg IV / IM / ET 9. Consider other causes (head injury, overdose, stroke, hypoxia, ALTE) 10. On-Line Medical Control contact is required for any refusal of treatment and/or transport with appropriate signatures obtained on AMA form. Tab 1100 Pediatric Protocol S-1 Pediatric Altered Mental Status, cont. Pediatric Altered Mental Status 1. Safe scene, standard precautions 2. Spinal immobilization (if indicated) 3. ABC (airway, breathing, circulation) 4. Oxygen 5. Move patient to vehicle, contact On-Line Medical Control 6. Vitals (Broselow Tape) 7. IV Normal Saline using regular drip tubing (10gtts) 8. BGL test 9. Glucose < 60 a. Oral Glucose b. Dextrose 1-2mL c. Glucagon IN / IM 0.5mg < 25Kg; 1.0mg > 25Kg (if no IV access) Glucose 60 – 250 a. Normal Saline bolus (10cc/Kg) b. If respirations are depressed Narcan 0.1mg/Kg IV / ET / IM Glucose > 250 signs of dehydration a. Normal Saline Bolus 10cc/Kg b. If signs of shock Normal Saline bolus 20cc/Kg 10. Contact On-Line Medical Control 11. Dextrose 25% 1-2mL/Kg IV (Draw 1-2ml/kg Dextrose 50% and dilute with equal ml saline) 12. Narcan 0.1mg/Kg IV / ET / IM 13, Glucagon IN / IM 0.5mg < 25Kg; 1.0mg > 25Kg Tab 1100 Pediatric Protocol S-2 T OPERATION SAFE HAVEN Emergency Medical Services Worker Obligations to Whom a Child Which is Less Than 72 Hours Old is Delivered (ORC 2151.3515 et.seq. Effective April 9, 2001) While acting in their official capacity an EMS worker (first responder, EMT-Basic, Intermediate, or EMT-Paramedic) on behalf of the Emergency Services Organization (as defined by 4765.01) that employs the worker or for which the worker provides services, shall take possession of a child who is seventy-two hour old or younger if that child’s parent has voluntarily delivered the child to that person without the parent expressing an intent to return for the child. Upon taking possession of the child the Emergency Services Organization shall do all of the following: A. Perform any act necessary to protect the child’s health or safety; B. Notify Dispatch that the child has been taken into possession; C. When forms developed by the Ohio Department of Jobs and Family Services (ODJFS) are available designed to gather medical information concerning the child and the child’s parents, provide such to surrendering parent; D. E. If available, offer written materials developed by ODJFS that describe services available to assist parents and newborns; Only if the child appears to have a condition which reasonable indicates physical or mental abuse or neglect-attempt to identify, and if necessary, pursue the person who delivered the child; EMS Workers shall Not: 1. Coerce or otherwise try to force the parent into revealing the identity of the child’s parents; 2. Pursue or follow the parent after the parent leave the place at which the child was delivered; 3. Coerce or otherwise try to force the parent not to desert the child; 4. Coerce or otherwise try to force the parent to accept the medical information forms promulgated by the ODJFS; 5. Coerce or otherwise try to force parent to accept materials promulgated by the ODJFS; Items (1) and (2) above do not apply to a person who delivers or attempts to deliver a child who has suffered any physical or mental wound, injury, disability, or condition or a nature that reasonably indicates abuse or neglect of the child. Tab 1100 Pediatric Protocol T-1 U PEDIATRIC HYPOTENSION/SHOCK (Non-Trauma) For this protocol, the pediatric patient is defined as < 16 years of age. History 1. 2. 3. Blood loss Fluid Loss a. Vomiting b. Diarrhea Infection Objective Findings 1. Restlessness 2. Dizziness 3. Increased HR, rapid pulse 4. Decreased BP 5. Pale, cool, clammy 6. Delayed capillary refill Differential a. b. c. d. f. Trauma Infection Dehydration Congenital heart disease Medication or toxin Special Considerations 1. Consider all possible causes of shock and treat per appropriate protocol. 2. Decreasing heart rate in pediatric patient is a sign of impending collapse. 3. The following Dextrose concentrations and dosing are recommended: a. Neonate: 1-2mL/Kg 12.5% Dextrose b. < 2 yrs: 1-2mL/Kg 25% Dextrose c. > 2 yrs: 1-2mL/Kg 50% Dextrose (Draw 1-2ml/kg Dextrose 50% and dilute with equal ml saline) 4. For symptomatic patients with low BGL values, and absent intravenous access, administer Glucagon IN / IM (0.5 mg < 25Kg; 1.0mg > 25Kg). Maximum dose of Glucagon is 1.0mg Tab 1100 Pediatric Protocol U-1 Pediatric Hypotension/Shock, cont. PEDIATRIC HYPOTENSION/SHOCK (Non-Trauma) 1. Scene safe, universal precautions 2. ABC (airway, breathing, and circulation) 3. If evidence or history of Trauma follow multiple trauma protocol (Tab 1100 W) 4. Oxygen therapy 15 L/min. 5. Move patient to vehicle, start transport. Contact On-Line Medical Control 6. Establish IV / IO using regular drip tubing (10gtts) 7. Take vitals, use Broselow Tape to determine weight in Kg. 8. Determine BGL a. > 60 Normal Saline bolus 20cc/Kg as needed. b. < 60 Oral Glucose (mentation?). Dextrose 1-2mL If no IV access administer Glucagon IN / IM 0.5mg < 25Kg; 1.0mg > 25Kg. Follow with a Normal Saline bolus 20cc/Kg. 10. Repeat vitals, contact On-Line Medical Control 11. Dopamine 5-20mcg/Kg/min Tab 1100 Pediatric Protocol U-2 V PEDIATRIC VOMITING AND DIARRHEA For this protocol, the pediatric patient is defined as < 16 years of age. History a. b. c. d. e. f. g. h. i. j. Time of last meal Last bowel Movement/ emesis Improvement of worsening with food or activity Duration of problem Other sick contacts Past medical History Medications Menstrual history (pregnancy) Travel history Bloody emesis/ diarrhea Objective Findings a. Pain b. Character of pain c. Distention d. Constipation e. Diarrhea f. Anorexia g. Radiation ASSOCIATED SYPTOMS (Helpful to localize source): Fever, headache, blurred vision, weakness, malaise, cough, dysuria, mental status changes, rash. Differential a. b. c. d. e. f. g. h. i. j. CNS Myocardial infarction Drug, medication or substance abuse GI or renal disorders Diabetic Ketoacidosis Infections (pneumonia, influenza) Electrolyte abnormalities Food or toxin induced Pregnancy or gynecological disease Psychological Special Conditions 1. Complete assessment and physical exam including evaluation of mental status, skin, HEENT, neck, heart, lungs, abdomen, back, extremities, and neuro. 2. Frequent re-assessments are needed to monitor vascular status. Tab 1100 Pediatric Protocol V-1 Pediatric Vomiting and Diarrhea, cont. PEDIATRIC VOMITING AND DIARRHEA 1. Scene safe, universal precautions 2. Establish responsiveness 3. ABC’s (airway, breathing, circulation) 4. Oxygen 5. Vitals (Broselow Tape) 6. Move patient to vehicle, contact On-Line Med Control 7. Establish IV Normal Saline using regular drip tubing (10gtts), 20cc/Kg bolus as needed 8. Attach cardiac monitor 9. Test BGL a. If < 60 refer to Altered Mental States protocol (Tab 1100 S) b. If > 250 10cc/Kg Normal Saline Bolus 10. Contact On-Line Medical Control Tab 1100 Pediatric Protocol V-2 W PEDIATRIC MULTIPLE TRAUMA For this protocol, the pediatric patient is defined as < 16 years of age. History a. b. c. d. e. f. g. h. Time and mechanism of injury Damage to structure or vehicle Other injured or dead Speed and details of MVC Restraints / protective equipment Ejection Past medical history Medications Objective Findings a. Pain, swelling b. Deformity, lesions, bleeding c. Altered mental status d. Unconscious e. Hypotension or shock (tachycardia may be only early sign, hypotension is a late sign) f. Arrest Differential (life threatening) a. Chest injury 1. Tension pneumothorax 2. Flail chest 3. Pericardial tamponade 4. Open chest wound 5. Hemothorax b. Intra-abdominal bleeding c. Pelvis / femur fracture d. Head injury (see head trauma Tab 1100 X) e. Extremity fracture / dislocation f. HEENT (airway obstruction) g. Hypothermia Special Considerations 1. Physical exam: Mental status, skin, HEENT, heart, lungs, abdomen, extremities, back, and neurovascular status. 2. Mechanism of injury is the most reliable indicator of serious injury. Examine all restraints and protective equipment for damage. 3. In prolonged extrications or serious trauma consider air ambulance transportation. 4. Severe bleeding from an extremity, not rapidly controlled, may necessitate the application of a tourniquet. Tab 1100 Pediatric Protocol W-1 -ALL TREATMENTS EXCEPT C-SPINE, CPR, AIRWAY, AND CONTROL OF LIFE THREATENING HEMORHAGE SHOULD BE INITIATED AFTER TRANSPORT. 1. Scene safe, universal precautions 2. C-spine (manual) 3. Evaluate LOC 4. ABC’s (airway, breathing, circulation) 5. Provide Oxygen 15 L/min NRB and airway control (consider use of advanced airway device if indicated) 6. Control life threatening hemorrhage 7. Transport decision 8. Extricate as necessary 9. Expose patient 10. Move patient to vehicle, contact On-Line Medical Control 11. Establish IV Normal Saline bolus 20cc/ Kg as needed 12. Vital signs / perfusion 13. If hypotension continues consider splinting of any fractures, control any external hemorrhaging. Also, consider chest decompression if there are signs and symptoms of tension pneumothorax. 14. Reassess for life threatening injuries 15. Contact On-Line Medical Control 16. Secondary survey Tab 1100 Pediatric Protocol W-2 X PEDIATRIC HEAD TRAUMA For this protocol, the pediatric patient is defined as < 16 years of age. History a. b. c. d. e. f. g. Time of injury Mechanism (blunt vs. penetrating) Loss of consciousness (LOC) Bleeding Past medical history Medications Evidence of multi-trauma Objective Findings a. Pain, swelling, bleeding b. Altered mental status c. Unconscious d. Respiratory distress / failure e. Vomiting f. Major traumatic mechanism of injury g. seizure Differential a. b. c. d. e. f. g. Skull Brain injury (concussion, contusion, hemorrhage, or laceration) Epidural hematoma Subdural hematoma Subarachnoid hemorrhage Spinal Injury Abuse Special Consideration 1. If GCS < 12 considerer rapid transport. With GCS < 8 anticipate advanced airway 2. 3. 4. 5. procedures. Mild hyperventilation should be considered only if evidence of herniation (blown pupil, decorticate / decerebrate posturing, bradycardia) Target EtCO2 value to 30 mmHg. Increased intracranial pressure may cause hypertension and bradycardia (Cushing’s Response). Hypotension usually indicates injury or shock unrelated to the head injury (ICP). The most important item to monitor and document is a change in level of consciousness. Tab 1100 Pediatric Protocol X-1 Pediatric Head Trauma, cont. 6. Concussions are periods of confusion or LOC associated with traumas which may have resolved by the time EMS arrives. Any prolonged confusion or mental status abnormality which does not return to normal within 15 minuets or any documented LOC should be evaluated by a physician immediately. 7. The following Dextrose concentrations and dosing are recommended a. Neonate: 1-2mL/Kg 12.5% Dextrose b. < 2: 1-2mL/Kg 25% Dextrose c. > 2: 1-2mL/Kg 50% Dextrose (Draw 1-2ml/kg Dextrose 50% and dilute with equal ml saline) For symptomatic patients with low BGL, and absent intravenous access, administer Glucagon IN / IM (0.5 < 25Kg; 1.0mg > 25Kg). Maximum dose of Glucagon is 8. 1mg. Tab 1100 Pediatric Protocol X-2 Pediatric Head Trauma, cont. -ALL TREATMENTS EXCEPT C-SPINE, CPR, AIRWAY, AND CONTROL OF LIFE THREATENING HEMORHAGE SHOULD BE INITIATED AFTER TRANSPORT. 1. Scene safe, universal precautions 2. C-spine (manual) (if not an isolated head trauma refer to pediatric multiple trauma protocol Tab 1100 W) 3. Evaluate LOC 4. ABC’s (airway, breathing, circulation) 5. Provide Oxygen 15 L/min NRB and airway control (consider use of advanced airway device if indicated) 6. Control life threatening hemorrhage 7. Transport decision. Move patient to vehicle, contact On-Line Medical Control 8. Establish IV / IO Normal Saline bolus 20cc/ Kg as needed 9. Vital signs / perfusion. Obtain GCS a. GCS > 8 1. Monitor and reassess every 5 minuets b. GCS < 8 1. Maintain airway with SPO2 > 90 (advanced airway device if indicated) 2. Seizure? If yes, refer to Pediatric Seizure Protocol (Tab 1100 P) 3. Obtain BGL, if < 60 administer Dextrose 1-2mL/Kg IV. ( Draw 1-2ml/kg Dextrose 50% and dilute with equal ml saline)If no IV access, Glucagon IN / IM (0.5mg < 25Kg; 1.0mg > 25Kg) 15. Contact On-Line Medical Control 16. Secondary survey Tab 1100 Pediatric Protocol X-3 Y PEDIATRIC EXTREMITY TRAUMA For this protocol, the pediatric patient is defined as < 16 years of age. History a. b. c. d. e. f. g. Type of injury Mechanism: crush / penetrating / amputation Time of injury Open vs. closed wound / fracture Wound contamination Medical history Medications Objective Findings a. Pain, swelling b. Deformity c. Altered mental status d. Diminished pulse / capillary refill e. Decreased extremity temperature Differential a. b. c. d. e. f. g. Abrasion Contusion Laceration Sprain Dislocation Fracture Amputation Special Considerations 1. Urgently transport any injury with vascular compromise. 2. Severe bleeding from an extremity not rapidly controlled may necessitate the application of a tourniquet. 3. Hip dislocations and knee and elbow fracture / dislocations have a high incidence of vascular compromise. 4. In amputations, transport and notify medical control immediately so that the appropriate destination can be determined. Tab 1100 Pediatric Protocol Y-1 Pediatric Extremity Trauma, cont. PEDIATRIC EXTREMITY TRAUMA 1. Scene safe, universal precautions 2. C-spine (if indicated) 3. Evaluate LOC 4. Provide Oxygen 15 L/min NRB and airway control (consider use of advanced airway device if indicated) 5. Wound care hemorrhage control. a. Amputaion? 1. Clean amputated part 2. Wrap in sterile dressing soaked in Normal Saline 3. Place in container / hazard waste bag 4. Place container on ice / refrigerate 6. Transport decision. Move patient to vehicle, contact On-Line Medical Control 7. Vitals 8. Establish IV Normal Saline bolus 20cc/ Kg as needed 9. Pain control (refer to Tab 1100 AA) 10. Contact On-Line Medical Control Tab 1100 Pediatric Protocol Y-2 Z PEDIATRIC BURNS For this protocol, the pediatric patient is defined as < 16 years of age. History a. b. c. d. e. f. g. h. Type of exposure Inhalation injury Time of injury Past medical history Medications Other trauma Loss of consciousness Tetanus / Immunization status Objective Findings a. Burns, pain, swelling b. Dizziness c. Hypotension / shock d. Airway compromise f. Singed facial or nasal hair g. Hoarseness / wheezing Differential a. b. c. d. e. g. Superficial (1st degree) Partial thickness (2nd degree) Full thickness (3rd degree) Chemical Electrical Radiation Special Considerations 1. Do not overlook the possibility of multiple system trauma. 2. Do not overlook the possibility of child abuse. 3. Burn patients are probe to hypothermia. Never apply ice or cool burns that involve > 10% body surface area. 4. Circumferential burns to extremities are dangerous due to potential vascular compromise secondary to soft tissue swelling. 5. Consider potential CO poisoning. Treat with 100% Oxygen via NRB mask. 6. Early advanced airway procedures may required for significant inhalation burns. 7. Critical burns (transfer to burn center) a. > 20% body surface area (BSA) age > 10 b > 10% BSA age < 10 c. 3rd degree burns > 5% Tab 1100 Pediatric Protocol Z-1 Pediatric Burns, cont. 8. 9. d. 2nd degree burns to face, eyes, hands, or feet e. Electrical burns f. Respiratory burns g. Deep chemical burns h. Burns with extremes of age or chronic disease i. Burns associated with major traumatic injury If airway involvement, consider transport to the closest hospital for optimal airway management. a. Be prepared to assist ventilations and put an advance airway in place if indicated. If pain control is needed, administer Fentanyl 1mcg/Kg IV / IN (not to exceed 50mcg/dose). If allergy administer Morphine 0.1-0.2mg/Kg IV (not to exceed 5mg/dose). Any additional amount must be authorized by On-Line Medical Control. Tab 1100 Pediatric Protocol Z-2 Pediatric Burns, cont. Thermal Burns - If no airway involvement, consider direct transport to Burn Center. 1. Scene safe, universal precautions 2. Remove any smoldering clothing or clothing that is non adherent to patient. Also, remove any rings, bracelets, and any other constricting items 3. Oxygen as indicated 4. Assess and treat for associated trauma 5. < 10% BSA (using rule of nines) 6. Cool with Normal Saline 7. Cover with dry sterile sheet or dressing 8. Vitals 9. Move patient to vehicle, contact On-Line Medical Control. 10. Establish IV access, Normal Saline bolus 20mL/Kg as needed (consider 2nd IV for burns > 30% BSA) 11. For pain control administer Fentanyl 1mcg/Kg IV / IN. If Fentanyl allergy administer Morphine 0.1-0.2mg/Kg IV Chemical Burns - If no airway involvement, consider direct transport to Burn Center. 1. Scene safe, universal precautions 2. Remove any smoldering clothing or clothing that is non adherent to patient. Also, remove any rings, bracelets, and any other constricting items 3. Oxygen as indicated 4. Assess and treat for associated trauma 5. Move patient to vehicle, contact On-Line Medical Control Tab 1100 Pediatric Protocol Z-3 Pediatric Burns, cont. 6. If eye involvement continually flush with Sterile Water in affected eye 7. Flush area with Sterile Water or Normal Saline for 10-15 minuets 8. Establish IV Normal Saline 20ml/Kg bolus as needed 9. For pain control administer Fentanyl 1mcg/Kg IV / IN. If Fentanyl allergy administer Morphine 0.1-0.2mg/Kg IV Tab 1100 Pediatric Protocol Z-4 PEDIATRIC RULE OF NINES (a useful approximation of body surface area) 1. Head: 18% 2. Arm: 9% each 3. Chest and Abdomen: 18% 4. Back and Buttocks: 18% 5. Leg: 13.5% each 6. Genitalia: 1% Tab 1100 Pediatric Protocol Z-5 AA PAIN MANAGEMENT For this protocol, the pediatric patient is defined as > 8 years or age. Applies to those with severe pain associated with an isolated injury. Contact Medical Control for pediatric pts. < 8 History a. b. c. d. e. f. Location Duration Severity Past medical history Medications Drug use Objective Findings a. Severity (pain scale) b. Quality (dull, sharp, etc) c. Radiation d. Relation to movement, respiration e. Increased with palpation of area Differential a. b. c. d. e. f. g. Per specific protocol Musculoskeletal Visceral (abdominal) Cardiac Pleural / respiratory Neurogenic Renal Specific Considerations 1. Studies show that pain is some type of presenting pain for up to 70% of patients. Pain evolution is no recognized as the “fifth vital sign”. 2. Care providers are influenced in their subjective evaluations of pain by other patient factors and by their prior personal and professional experience with pain. Self-reporting is actually shown to be the most accurate reflection of pain intensity, NOT the care provider’s opinion. 3. Objective measures or pain ratings improve pain management by: a. Balancing imprecise clinician pain assessment b. Tracking success of pain management Tab 1100 Pediatric Protocol AA-1 Pediatric Pain Management, cont. 4. Pain assessment a. Numeric rating (1-10) b. Visual analog scale (pain level marked on a horizontal line) c. Verbal rating scale (none, mild, moderate, severe, unbearable) d. 5. 6. 7. 8. 9. 10. Wong Baker FACES scale (pediatrics) A number of studies have shown that early administration of analgesics allows patients to relax, removes voluntary guarding and permits better assessment of localized tenderness. Guidelines for safe analgesics: a. Be aware of effects of combining drugs: Adding one CNS depressant or hemodynamic depressant to another can create unpredictable changes. b. Adding IV analgesics on top of Don’t forget about medication allergies: recently taken oral sedatives, or muscle relaxants may cause unpredictable additive effects as well. c. Know your pain management goal: Your goal may actually be different to different types of patients (reduction of pain vs. removal of pain. d. Give a complete report to ED staff: Drugs given, time, results, and adverse effects. Assess serial vital signs with emphasis on blood pressure, respiratory status and LOC. Analgesics administration in the fied must be transported to Hospital with ALS. Analgesic administration precludes a patient’s ability to refuse transport due to possible altered mental status. Administer Fentanyl at 1mcg/Kg IV / IN (not to exceed 50mcg/dose). If allergy to Fentanyl, administer Morphine 0.1-0.2mg/Kg (not to exceed 5mg/dose). Repeat dosing of analgesics must be authorized by On-Line Medical Control. Tab 1100 Pediatric Protocol AA-2 Pediatric Pain Control, cont. PEDIATRIC PAIN CONTROL 1. Scene safe, universal precautions 2. C-spine (if indicated) 3. Evaluate LOC 4. ABC’s, Oxygen and airway control as indicated. 5. Transport decision. Move patient to vehicle, contact On-Line Medical Control 7. Vitals 8. Establish IV Normal Saline. 9. Pain severity: a. < 8 use distraction techniques b. 8 or > Fentanyl 1mcg/Kg IV / IN. If Fentanyl allergy, Morphine 0.1-0.2mg/Kg IV. 10. Contact On-Line Medical Control Tab 1100 Pediatric Protocol AA-3