in vivo </Emph - Bioscience Reports
advertisement

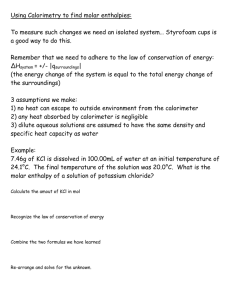
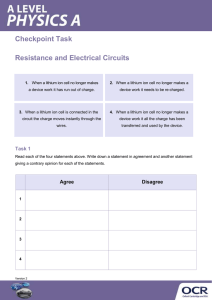
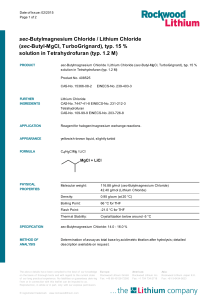
Bioscience Reports, Vol. 7, No. 9, 1987 In Vitro and In Vivo Effect of Chloropromazine, Imipramine and Lithium Chloride on Monoamine Oxidase Activity in Rat Brain Mitochondria Maitreyi Nag t and Namita Nandi Received May 20, 1987 KEY W O R D S : m o n o a m i n e oxidase; chloropromazine; imipramine; lithium chloride. Chloropromazine (CPZ) and imipramine at a concentration of 1 x 10- 3 M inhibit rat brain mitochondrial monoamine oxidase activity in vitro by 70 and 55 % respectively, 'while lithium, even at a concentration of 0.05 M, inhibits the activity of this enzyme 'very negligibly (4%). In vivo, these drugs at a dose level of 56 mg CPZ, 76 mg Jimipramine and 76 mg lithium chloride/Kg body wt., did not cause any observable 'variation from normal in brain mitochondrial monoamine oxidase activity. INTRODUCTION Lithium salts are effective in the treatment of unipolar and bipolar mania and ,depression (1). However, in severe excited or aggressive states, lithium alone is less ,effective than in combination with other drugs, e.g. chloropromazine (CPZ) and imipramine (2,3). Substantial evidence suggests that CPZ is a potent adrenergic blocker while imipramine shows this effect only in large doses (4). Based largely on the observation that mood-altering drugs can affect the function of central neurotransmitter amines in animals (5,6), it has been hypothesized that affective illness may involve alterations in brain norepinephrine. A number of investigators (7,8,9) have therefore been interested in the effect of lithium, CPZ and imipramine administration on brain amine function. Noradrenalin discharged from the neuron in physiologically Indian Institute of Chemical Biology, 4 Raja S.C. Mullick Road, Jadavpur, Calcutta 700 032. t To w h o m correspondence should be addressed. 701 0144-8463/87/0900-0701505.00/0 9 1987Plenum PublishingCorporation 702 Nag and Nandi active form is inactivated mainly by cellular reuptake or by conversion to normetaepinephrine through enzymatic O-methylation. Norepinephrine released intracellularly either spontaneously or by reserpine-like drugs is inactivated primarily by mitochondrial monoamine oxidase (MAO) before leaving the cell (10). Although MAO does not play a major role in terminating the activity of norepinephrine at receptor, it may be largely responsible for regulating the level of norepinephrine in neurons (11). In this report, the effects of these drugs on MAO activity in rat brain mitochondria has been studied. MATERIALS AND METHODS Male albino rats (120-150 grams) were killed by decapitation and the brain tissue was removed and homogenized in chilled 0.25 M sucrose to give a 10 % suspension (w/v) and the crude mitochondrial fraction was prepared according to Broody and Bain (12) which served as the source of MAO. Mitochondria was resuspended in isotonic sucrose to give 10% suspension. The standard assay mixture for MAO contained 0.025 M phosphate buffer, pH 7.0, mitochondria 500mg, 0.1 M tyramine HC1, 0.0125 M semicarbazide, drugs (as shown in Table 1) and water in a total volume of 2 ml. All incubations were carried out at 37~ for 30 minutes with air as the gas phase. The enzyme was preincubated with drugs for 15 minutes at 37~ prior to the addition of tyramine. Protein was estimated by the method of Lowry et al. (13) using bovine serum albumin as the standard. Aldehyde formed was measured at 450 mM by the method of Green and Haughton (14) with slight modification as described previously (15). The enzyme activities are expressed on the basis of #moles product formed/ 30 min/3 mg protein. For the in vivo experiments CPZ, imipramine and lithium chloride were injected dermally on alternate days in a single dose for 2 weeks at a dose of 56 mg, 76 mg and 77 mg/kg body wt. respectively. Control rats were treated with saline for the same Table 1. Effect ofchloropromazine, imipramine and lithium chloride on monoamine oxidase activity of rat brain mitochondrial fraction [values are mean + SD of six observations in each group] Drugs Conc. (M) Micromoles of aldehyde-dinitrophenyl hydrazone formed/30 min/3 mg protein Without drug With drug % inhibition Chloropromazine (CPZ) 5 x 1O- 4 1 x 10 -3 0.222 _+ 0.047 0.195 _+ 0.017 0.073 + 0.013 0.059 + 0.004 67 70 Imipramine 1 • 10 -4 1 x 10 -3 0.206 _+ 0.037 0.224 + 0.030 0.124 _+ 0.003 0.101 + 0.020 40 55 Lithium chloride 5 x 10 -2 0.191 + 0.021 0.183 _ 0.025 4 Lithium chloride (A) and CPZ (B) 5 • 10 -2 1 • 10 -3 0.234 + 0.140 0.078 + 0.007 67 Lithium chloride (A) imipromine (B) 5 x 10 -z 1 x 1O-3 0.230 + 0.017 0.098 + 0.005 57 Effect of D r u g s on M o n o a m i n e O x i d a s e 703 period. All the rats (drug treated and control) were sacrificed after two weeks and MAO activity was estimated in the brain mitochondrial fraction. RESULTS AND D I S C U S S I O N The table shows that imipramine and CPZ both inhibit monoamine oxidase activity in rat brain mitochondrial fraction in vitro, while lithium chloride (0.05 M) negligibly inhibits the activity. Imipramine at a concentration of 1 x 10-3 M inhibits the enzyme activity by 55 %, while at a concentration of 1 x 10 -4 M enzyme activity is inhibited by 40 %. CPZ inhibits MAO activity by nearly 70 % both at a concentration of 1 x 10 -3 M and 5 x 10 -4 M. The inhibition of enzyme activity either by C P Z or by imipramine does not change much when combined with lithium in vitro. Results of in vivo studies with the above drugs could not demonstrate any variation of MAO activity from the saline treated control rats (Fig. 1). Although our results with lithium chloride agree with the results of other investigators who could not demonstrate any significant effect of lithium chloride either in rat brain (7) or in renal cortex (16), Bocker et al. (17) and Kisseleva (18) demonstrated increased MAO activity in the platelet (in vivo) and in rat brain homogenate (in vitro) respectively. Although there may be some specific similarities when platelet MAO and MAO localized in different brain areas are compared (19), the degree to which platelet MAO may reflect changes in brain is not known. From out studies, it may be assumed that I I Control CPZ "O >'/-~ 9. I / ~ A 17 0 (D "-- c~ Z//;I 0.15 0 ./.,., Cl /, /I/ A"~ ~ ,//A x: Z IA ,.I-~ '*-- r- "O F~ Lithium 0.20 E 0 FrTTT] Imipramine 0.10 r- M,.- o 0 1 0.05 If) N') ,,''/'1 "/'~ i/ I 0 z_ Fig. 1. I~ "/'~ ////I 0 //A Effect o f C P Z , i m i p r a m i n e a n d l i t h i u m chloride on M A O activity of rat b r a i n m i t o c h o n d r i a . 704 Nag and Nandi lithium, the tricyclic a n t i d e p r e s s a n t i m i p r a m i n e a n d the t r a n q u i l i z e r C P Z affect the a m i n e m e t a b o l i s m by a m e c h a n i s m o t h e r t h a n t h a t of interfering with o x i d a t i v e d e a m i n a t i o n . L i t h i u m alters the a m o u n t of m o n o a m i n e n e u r o t r a n s m i t t e r reaching the p o s t - s y n a p t i c r e c e p t o r ceils by increasing the n e u r o n a l u p t a k e (17,20). It m a y also alter the a m i n e m e t a b o l i s m by interfering with the d i s c h a r g e of p r e s y n a p t i c vesicles (21). Both the a n t i d e p r e s s a n t i m i p r a m i n e a n d the t r a n q u i l i z e r C P Z a p p e a r to i n h i b i t the u p t a k e of n o r e p i n e p h r i n e . U n l i k e the i m i p r a m i n e , C P Z , which is a central adrenergic b l o c k e r , does n o t c o n c u r r e n t l y increase the n o r e p i n e p h r i n e level in b r a i n (7). H e n c e it m a y be c o n c l u d e d t h a t a n y of the drugs, e.g. l i t h i u m chloride, C P Z o r i m i p r a m i n e , m a y alter the a m i n e m e t a b o l i s m n o t by affecting o x i d a t i v e d e a m i n a t i o n , but b y other processes as discussed above. ACKNOWLEDGEMENTS T h a n k s are d u e to M r S. G. K u n d u a n d M r P. S e n g u p t a for their assistance in u n d e r t a k i n g this research w o r k . REFERENCES 1. Gershon, S. and Shopsin, B. (1973). Lithium: Its role in Psychiatric Research and Treatment, Plenum Press, New York. 2. Schou, M. (1976). Neuro. Res, Program Bull. 14:117-121. 3. Garver, D. L. and Davis, J. M. (1979). Life Sci. 24:383-393. 4. Von Haefely, W., Hurlimann, A. and Thoenen, H. (1964), Helv. physiol, pharmac, aeta. 22:15 18. 5. Schildkraut, J. J. (1965). Am. J. Psychiat. 122:509-522. 6. Bunney, W. E. Jr. and Davis, J. M. (1965). Arch, gen, Psychiat. 13:509-522, 7. Schanberg, S. M., Schildkraut, J. J. and Kopin, I. J. (t967). Biochem. Pharmacol. 16:393-399. 8. Beckmann, H., Laurent, J. S. and Goodwin, F. K. (1975). Psychopharmacol. 42:277-282. 9. Murphy, D. L., Colburn, R. W., Davis, J. M. and Bunney, W. E. Jr. (1970). Am. J. Psychiat. 127:339 345. 10. Kopin, I. J. (1966). Pharmae. Rev. 18:513-523. 11. Glowinski, J., Kopin, I. J. and Axelord, J. (1965). J. Neurochem. 12:25-30. 12. Brody, T. M. and Bain, J. A. (1950). J. Biol. Chem. 195:685-695. 13. Lowry, O. H., Rosebrough, N L, Farr, A. L. and Randall, R. J. (1951). J. Biol. Chem. 193:265-275. 14. Green, A. L. and Haughtou, T. M. (1964). Biochem. J. 78:172-175. 15. Guha, S. R. (1966). Biochem. Pharmaeol. 15:161-168. 16. Batdessarini, R. and Yorke, C. (1970). Nature 288:1301-1303. 17. Blocker, J., Roth, R. and Heninger, G. (1974). Life Sci. 15:2109-2118. 18. Kiseleva, I. (1972). Vapr. reed. Zhym. 18:449-506. 19. Collins, G. G. S., Sandler, M., William, E. D. and Youdim, M. B. H. (1970). Nature 225:817-820. 20. Colburn, R. W., Goodwin, F. K., Bunney, W. E. Jr. and Davis, J. M. (1967). Nature 215:1395 1397. 21. Bunney, W. E. Jr., Gershon, E. S., Murphy, D. L. and Goodwin, F. K. (1972). J. Psychiat. Res. 9:207 226.