Changes in cross-sectional area of the coronary lumen
advertisement

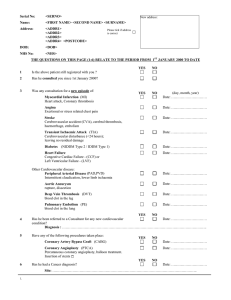
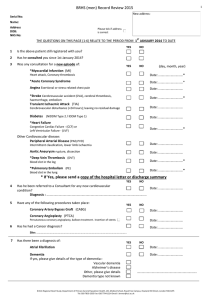
THERAPY AND PREVENTION PTCA Changes in cross-sectional area of the coronary lumen in the six months after angioplasty: a quantitative analysis of the variable response to percutaneous transluminal angioplasty MARYL R. JOHNSON, M.D., GAIL P. BRAYDEN, M.D., ELIZABETH E. ERICKSEN, M.S.E.E., STEVE M. COLLINS, PH.D., DAVID J. SKORTON, M.D., DAVID G. HARRISON, M.D., MELVIN L. MARCUS, M.D., AND CARL W. WHITE, M.D. Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016 ABSTRACT Although immediate and late changes in coronary stenoses after percutaneous transluminal coronary angioplasty (PTCA) have been reported, most investigators have employed qualitative or semiquantitative techniques to analyze the angiograms. Such data is not optimal because of considerable interobserver variability and the use of relative instead of absolute changes in lesion geometry. Analysis is further compounded by the indistinct edges that characterize coronary lesions immediately after angioplasty. To quantify the changes in minimal cross-sectional area (MCSA) of the coronary lumen that occur during and after PTCA, we analyzed the angiograms of 23 patients before PTCA, SD) months follow-up using two computerimmediately after PTCA, and at 7.2 + 3.0 (mean assisted methods of angiographic analysis quantitative coronary angiography (QCA) and videodensitometry (VID). QCA provides an absolute measure of the area of the lumen; VID is a nongeometric method that is not dependent on exact border recognition. Based on these quantitative methods, we found that successful angioplasty is associated with about a three-fold increase in the MCSA of the lesion (from 1.0 to 3.2 mm2). This area is, however, well below normal and is less than half of the average MCSA of the inflated dilating balloon. Analysis of follow-up angiograms demonstrated that eight of 23 patients had a substantial late increase in the MCSA of the lesion (from 2.7 to 4.1 mm2) after the angioplasty procedure. Clinical, hemodynamic, and angiographic characteristics immediately after PTCA were not predictive of MCSA of the lumen at follow-up. Because substantial late increases in MCSA of the lumen occur in about one-third of patients, angiographic and noninvasive analyses performed immediately after PTCA will not define the ultimate adequacy of coronary dilation in many patients undergoing PTCA. Circulation 73, No. 3, 467-475, 1986. ± PERCUTANEOUS transluminal coronary angioplasty (PTCA) has gained wide clinical acceptance as a treatment for coronary artery disease.1' 2 Despite widespread use, however, neither the mechanisms responsible for the initial coronary luminal enlargement From The Cardiovascular Center, The Cardiovascular Image Processing and Ultrasonic Imaging Laboratories, and Departments of Internal Medicine, Electrical and Computer Engineering, and Radiology University of Iowa and Iowa City Veterans Administration Medical Center, Iowa City. Supported by National Institutes of Health grants HL27633, HL29976, HL00916, HL14388, HL32295 (Specialized Center of Research in Ischemic Heart Disease), and HL01290 (Research Career Development Award, Dr. Skorton), and the U.S. Veterans Administration grant MRIS 1100.2. Address for correspondence: Maryl Johnson, M.D., Cardiovascular Division, Department of Internal Medicine, University of Iowa Hospitals and Clinics, Iowa City, IA 52242. Received July 1, 1985; revision accepted Oct. 3, 1985. Vol. 73, No. 3, March 1986 produced by PTCA nor the factors that determine the duration of the increase in the size of the lumen are well understood. Previous angiographic follow-up studies have shown that restenosis occurs in approximately onethird of initially successful dilations.3 Visual estimates of percent stenosis have also suggested that in some cases a further increase in size of the lumen may occur in the 6 months after PTCA.' 6,7 The significance of such observations based on percent stenosis is uncertain for several reasons. First, estimates of percent stenosis are associated with a high degree of interobserver variability." Second, measurements of percent stenosis correlate poorly with size of the lumen and physiologic significance of the lesion.'2 '4 Third, immediately after angioplasty, the dilated coronary 467 JOHNSON et al. Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016 segment has a shaggy or rough appearancel 15 and luminal borders may be difficult to define. Finally, assessing changes in size of the lumen with the use of percent stenosis after angioplasty may be especially difficult since balloon dilation may change the adjacent "tnormal" segment as well the stenotic segment. 16 In this study we used two computer-assisted methods of angiographic analysis - quantitative coronary angiography and videodensitometry - to quantify the changes in cross-sectional area of the coronary lumen that occur during and after angioplasty. Such quantitative studies of dilated lesions may help elucidate the mechanism of continued symptom relief in most patients after PTCA. In addition, if quantitative angiographic characteristics of the lesion immediately after angioplasty or changes in size of the lumen from before to immediately after PTCA predict the course of the patient during follow-up, perhaps the need for follow-up coronary angiography to detect asymptomatic restenosis could be obviated. Quantitative coronary angiography was selected since it has low interobserver variability and provides an absolute measure of the cross-sectional area of the vessel.'17 18 Such absolute measures of luminal area correlate with the physiologic significance of coronary stenoses.'3 Videodensitometric analysis was selected as a nongeometric approach that is not based on the assumptions inherent to quantitative coronary angiography. During videodensitometry, x-ray transmission through the contrastfilled coronary artery provides an index of size of the lumen that is independent of its shape.'9 Therefore, the videodensitometric method is not directly dependent on precise operator definition of vessel edges and may be particularly appropriate for evaluating lesions immediately after PTCA when vessel edges may be indistinct and the shape of the lumen may be irregular. Videodensitometric analysis of coronary lesions is reproducible, and the results of videodensitometric analysis correlate with size of the coronary lumen and with the physiologic significance of the lesion.20 21 Methods Patient population. Between June 1981 and September 1982, 47 patients underwent single-vessel angioplasty at the University of Iowa. The lesion was successfully dilated in 30 of the 47 cases (64%). All patients with successful angioplasties were asked to return for routine follow-up coronary angiography at 6 months. Twenty-five patients (83%) did so. Twentythree of these patients, restudied at 7.2 + 3.0 (mean + SD) months after angioplasty, had high-quality initial and follow-up angiograms that were adequate for analysis by quantitative coronary angiography. Thus, 23 patients form the basis of this report. The angiograms of 18 of these patients were also technically suitable for videodensitometric analysis. 468 PTCA protocol. The investigational protocol and consent forms were approved by the institutional review committee of the University of Iowa and written informed consent was obtained from each patient before angioplasty. Pharmacologic therapy. For 24 to 48 hr before PTCA, patients were treated with 325 mg aspirin every 8 hr, 75 mg dipyridamole every 8 hr, and 10 mg nifedipine every 8 hr (minimum dose). Whenever possible /3-blocker therapy was tapered over the same period and discontinued at least 6 to 12 hr before the procedure. During the angioplasty procedure, all patients received 200 to 500 ml 10% Dextran in normal saline by infusion and nitroglycerin sublingually and/or by the intracoronary route (average dose 1.0 + 0.1 mg, mean + SEM). Eighteen of the 23 patients were also treated with sublingual nifedipine (average dose 14.4 + 1.7 mg). Intravenous nitroglycerin was administered to one patient during the procedure. Nifedipine, aspirin, and dipyridamole were continued during the follow-up period. l3-Blocker therapy was resumed at the time of hospital discharge. Follow-up angiograms were performed after sublingual and/ or intracoronary nitroglycerin in 22 of the 23 patients (average dose 0.6 + 0.1 mg). Two patients received sublingual nifedipine and one patient received intravenous nitroglycerin at the time of follow-up angiography. Coronary angiography. Coronary angiography was performed by the percutaneous femoral technique described by Judkins.22 Angiograms were obtained in multiple single-plane projections with the use of a Siemens angioscope with a 7 inch cesium iodide image intensifer. The angiograms were recorded on 35 mm film at 60 frames/sec. Projections were selected so that orthogonal right anterior oblique (RAO) and left anterior oblique (LAO) views of the vascular segmpent containing the lesion were available for analysis. Film processing was carefully controlled. Measurement of intracoronary pressures and lesion gradients. Arterial pressure measurements were made with a contrast-filled diagnostic or guiding coronary catheter immediately before contrast injections. The mean pressure gradient across the stenosis was measured before and after completion of angioplasty with the guiding catheter and the angioplasty catheter, both of which were filled with contrast. Angioplasty techniques. All dilations were performed with a USCI DG or G 20-30 balloon and were done before the availability of steerable catheter systems. An average of four dilations per procedure were used. Dilation pressures ranged from 2 to 9 atmospheres, with the average inflation time being 20 sec. Quantitative coronary angiography. The Brown-Dodge system of quantitative coronary angiography'7 18 was used to define absolute minimal coronary cross-sectional area in the vicinity of the dilated lesion. Data from two orthogonal midcycle cine frames was entered into the computer and the absolute minimal cross-sectional area of the vascular segment was determined automatically by the computer program. 17 This analytic procedure was repeated for each of three consecutive paired orthogonal angiographic frames of lesion segments before PTCA, immediately after PTCA, and at follow-up. The average value of the determinations of minimal cross-sectional area from the three sets of frames at each angiographic study was then calculated and reported as the lesion minimal cross-sectional area. The size of the inflated dilating balloon at an average inflation pressure was similarly determined with quantitative coronary angiographic techniques. The reproducibility of quantitative coronary angiographic measurements of minimal cross-sectional area of the coronary lumen in the study population was defined by having two independent observers perform the analysis on each pre-PTCA, immediate post-PTCA, and follow-up angiogram. CIRCULATION THERAPY AND PREVENTION-PTCA Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016 Videodensitometric analysis. Videodensitometric analysis was performed as previously described.20 Individual cine frames were digitized with a Vanguard cine film transport, the projected image of which was coupled through selectable optical lenses to a high-quality vidicon camera (Cohu model 8000). Prior to digitizing cine frames, calibration data relating mean gray level (digitized value) and optical density of the film were measured using a Kodak gray level step-wedge with 21 optical density levels. These data were entered into the computer, and a continuous calibration curve was calculated by use of linear interpolation between measured data points. Individual cineangiographic frames were then digitized at a magnification of 3.7 into a 512 x 512 pixel matrix with eight-bit (256 levels) graylevel resolution. The digitized images were displayed on a video monitor and an operator-interactive program was used to perform the videodensitometric analysis. The length of the segment of the vessel to be analyzed was identified by the operator. The computer then calculated and displayed a gray-level profile perpendicular to the axis of the vessel at the defined segment of interest. Using the plotted profile as an aid, the operator then identified the vessel borders as well as background regions on both sides of the vessel. The gray-level profile for each lesion was converted to an optical density profile with the use of the previously determined calibration curve. The optical density for each point on the profile within the vessel was corrected for the optical density of the corresponding background, and an integrated optical density value for the vascular segment of interest was obtained by summing the resultant optical densities over all points within the vessel. This value for integrated optical density was reported in optical density units. Under certain assumptions,23 integrated optical density is proportional to cross-sectional area of the lumen. We have previously found that values of integrated optical density determined in this way have good intraobserver (r = .98) and interobserver (r = .87) reproduc- ibility.21 Statistical methods. Except as otherwise noted, values are expressed as mean + SEM. Interobserver variability for quantitative coronary angiographic analysis was defined in two ways. First, we calculated the average percent variability between values of minimal cross-sectional area determined by the two observers. Second, we defined the mean absolute variability (in mm2) for all lesions analyzed by both observers. Interobserver variability before PTCA, immediately after PTCA, and at follow-up were compared by analysis of variance (ANOVA). Variability at the different times was also compared by use of confidence intervals of the calculated sample variance of the differences. Hemodynamic data for the patient groups before PTCA, immediately after PTCA, and at follow-up were analyzed by ANOVA and Duncan's multiple-range test. Quantitative coronary angiographic and videodensitometric data from the pre-PTCA, post-PTCA, and follow-up angiograms were also analyzed by ANOVA and Duncan's multiple-range test. Linear regression analysis was used to compare results obtained with quantitative coronary angiography to those obtained with videodensitometric analysis. Results Patient population. The study group included 16 men and seven women with a mean age of 53.3 ± 1.9 years. The mean duration of angina before PTCA was 7.6 + 2.7 months. The group included 15 patients who underwent PTCA of the left anterior descending coronary artery, six who underwent PTCA of right coronary artery, and two who underwent PTCA of the Vol. 73, No. 3, March 1986 circumflex artery. The clinical indication for angioplasty was stable angina in 10 (43%), unstable angina in six (26%), and severe residual stenosis after myocardial infarction in seven (30%). Thirteen patients (57%) had recurrent chest pain believed to be compatible with angina before follow-up angiography. This recurrent pain was mild in three patients and moderate in 10 patients. At the time of angiographic follow-up, 19 patients were still taking one or more antianginal drugs (nitrates in 14 patients, calcium-channel blockers in nine patients, and /3-blockers in nine patients). Other clinical features of the patient population included diabetes mellitus in one (4%), hypertension TABLE 1 Minimal cross-sectional areas of coronary lesions before PTCA, immediately after PTCA, and 6 months after PTCA MCSA (mm2) Patient No. Group A (n 8) 1 2 3 4 5 6 7 8 Mean +SEM Group B (n 7) 9 10 11 12 13 14 15 Mean -+SEM Group C (n -8) 16 17 18 19 20 21 22 23 Mean + SEM Before After Vessel PTCA PTCA Follow-up LAD RCA LCX LAD RCA LAD RCA RCA 1.43 1.03 1.28 0.45 1.15 1.53 1.27 0.64 1.08 0.13 1.57 2.29 3.24 2.90 1.92 3.85 3.26 2.85 2.74 0.27 1.87 2.80 4.32 3.93 4.70 4.66 7.07 3.37 LAD LAD RCA LAD LAD LCX LAD 0.78 0.70 0.74 1.83 1.36 0.41 0.59 0.92 0.19 2.43 2.37 4.19 4.11 2.74 3.31 2.36 3.07 0.30 2.64 1.98 3.73 4.72 2.61 3.21 1.98 2.98A 0.37 LAD LAD LAD LAD LAD LAD LAD RCA 1.57 0.88 0.86 0.58 0.97 1.56 1.41 1.12 1.12 0.13 2.71 5.73 2.63 1.94 3.54 4.65 3.37 5.13 3.71 0.47 2.07 1.05 1.42 0.92 1.49 1.60 1.42 2.98 1.62 0.23 4.09A 0.55 MCSA - minimal cross-sectional area of vessel defined by quantitative coronary angiography; LAD = left anterior descending coronary artery; RCA = right coronary artery; LCX = left circumflex artery. Ap < .05 compared with group C at follow-up. 469 JOHNSON et al. in nine (39%), hypercholesterolemia (greater than 250 mg/dl) in eight (35%), and a history of smoking in 15 (65%). Quantitative coronary angiography - interobserver Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016 variability. Average interobserver variability was found to be 41% for the pre-PTCA angiograms and 17% for the immediate post-PTCA and follow-up angiograms. The larger percent variability in the pre-PTCA group reflected the smaller size of the lumen before PTCA than after PTCA or at follow-up (table 1). When considered in absolute terms, interobserver variability was similar for the pre-PTCA, post-PTCA, and follow-up angiograms (0.4, 0.6, and 0.6 mm2, respectively; p = NS by ANOVA). The confidence intervals for interobserver variability were not different immediately after PTCA compared with at follow-up. Patient subgroups. Patients were divided into three groups based on the change in minimal cross-sectional area of the coronary lumen from the angiogram obtained immediately after PTCA to the angiogram obtained at follow-up. Changes greater than those due to our average percent interobserver variability (±+ 17%) were considered significant for the purpose of defining the groups. The three groups thus defined were as follows: group A (n = 8), patients with a significant increase in minimal cross-sectional area of the coronary lumen during follow-up; group B (n = 7), patients with no significant change in minimal crosssectional area of the coronary lumen during follow-up; group C (n = 8), patients with a significant decrease in minimal cross-sectional area of the coronary lumen (i.e., restenosis) during follow-up. Groups A, B, and C did not differ with respect to age, duration of angina before PTCA, history of smoking, or incidence of diabetes mellitus, hypertension, or hypercholesterolemia. Although there were no significant differences in nitroglycerin or nifedipine therapy among the groups at the time of angioplasty or at follow-up, patients in all groups received more vasodilator therapy during the PTCA procedure than at the follow-up catheterization. Table 2 lists the hemodynamic measurements made at the time of PTCA and at the follow-up catheterization. The transstenotic gradient before and immediately after PTCA, as well as the change in gradient from before to immediately after PTCA, did not differ significantly between the groups. The mean aortic pressure immediately after PTCA and at followup did not differ between the groups. Similarly, for groups A, B, and C the mean aortic pressure was not significantly different immediately after PTCA than at follow-up. Seventy-five percent of group A 470 TABLE 2 Hemodynamic measurements at PTCA and follow-up Transstenotic gradient (mm Hg) Before PTCA After PTCA Mean aortic pressure (mm Hg) After PTCA Follow-up Ap = Group A Group B Group C 54.0±6.5 22.2±6.7 49.0±6.5 15.0±5.3 46.0±4.5A 11.1 ±3.0A 70.0±6.5 79.9±4.8 78.8±4.4 81.0±7.0 64.0±4.1A 72.9±2.9A NS, group A vs group B vs group C. patients, 38% of group B patients, and 50% of group C patients had complaints of chest pain before follow-up angiography. Characteristics of coronary lesions - quantitative coro- nary angiography. Table 1 shows the minimal crosssectional areas of the dilated coronary arterial segments before PTCA, immediately after PTCA, and at follow-up for the groups. Groups A, B, and C did not differ significantly with respect to mean size of the lumen before PTCA, mean size immediately after PTCA, or the change in size from before to immediately after PTCA. Thus, immediate results were comparable in the three patient groups. At follow-up, size of the coronary lumen was significantly greater in groups A and B than in group C (p < .05). Figure 1 shows the individual values for minimal cross-sectional area of the lumen before PTCA, immediately after PTCA, and at follow-up for group A patients (n = 8), the patients who showed an increase in minimal cross-sectional area of the lumen during the follow-up period. Figure 1 also shows the cross-sec- 8 6 Minimal CrossSectional Area 4 (mm2) 2 0 Before PTCA Follow Inflated Balloon FIGURE 1. Vessel minimal cross-sectional areas for group A patients before PTICA, immediately after PTCA, and at follow-up. Also shown for reference is the cross-sectional area of the inflated dilating balloon as Immediately After PTCA up defined by quantitative coronary angiography. CIRCULATION THERAPY AND PREVENTION-PTCA Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016 tional area of the inflated angioplasty balloon used in these patients as determined by quantitative coronary angiography (6.9 mm2). In this patient group, the minimal cross-sectional area of the lesion was 2.74 ± 0.27 mm2 immediately after angioplasty. Minimal crosssectional area of the lesion had increased an average of 49% by the time of the follow-up study (to 4.09 + 0.55 mm2). In three of the patients, the increase in size of the lumen during follow-up was greater than the increase in size from before to immediately after angioplasty. In all of the patients, however, size of the lumen immediately after angioplasty was significantly less than the cross-sectional area of the inflated dilating balloon. The mean minimal cross-sectional area of the dilated segment in group A patients immediately after PTCA was 40% of the cross-sectional area of the inflated dilating balloon. This increased to 59% of the cross-sectional area of the inflated dilating balloon during follow-up. The cross-sectional area of the dilated segment at follow-up was similar to the size of the inflated dilating balloon in only one patient. Characteristics of coronary lesions - videodensitometric analysis. Eighteen of the patients had initial and followup angiograms that were analyzed by videodensitometric analysis. As shown in figure 2, the results of videodensitometric analysis performed on these angiograms correlated well with results of quantitative coronary angiography (r - .77). The changes in size of the coronary lumen in patients in group A (figure 3), group B (figure 4), and group C (figure 5) were similar whether defined by videodensitometric techniques or quantitative coronary angiography. Using videodensitometric techniques, we again found no significant Quantitative Coronary Angiography 6 Minimal CrossSectional Area (MM2) 4 2 0 Before Immediately Follow up PTCA After PTCA Videodensitometry 20 -* 15 Integrated Optical 10 Density 5 0 Before Immediately Follow PTCA After PTCA up FIGURE 3. Coronary lumen sizes for group A patients before PTCA, immediately after PTCA, and at follow-up, defined by quantitative coronary angiography (top) and videodensitometry (bottom). *p < .05 compared with integrated optical density immediately after PTCA. 8 differences in lumen size before PTCA or immediately after PTCA between the groups, confirming that the immediate results of angioplasty were the same in all groups. At follow-up, integrated optical density, an index of cross-sectional area of the lumen, was significantly greater in groups A and B than in group C (p < .05). Two of the five group A patients in whom videodensitometric analysis was performed showed evidence of an increase in area of the lumen during follow-up that was greater than the increase in area from before to immediately after PTCA. Thus, our data, obtained by two methods of quantitative angiographic analysis, illustrate the variable outcome of dilated lesions during follow-up despite similar results immediately after PTCA. FIGURE 2. The relationship between integrated optical density (defined by videodensitometric analysis and reported in optical density units) and minimal cross-sectional area of the lesion (defined by quantitative coronary angiography) for pre-PTCA, post-PTCA, and follow-up angiograms of 18 patients. Discussion There is considerable evidence, in addition to subjective angiographic findings, that PTCA represents an effective treatment for selected coronary stenoses. This evidence includes decreased transstenotic gradi- 25 20 15 Integrated Optical Density 10 A 5 r=0.77 n=54 ~ 0 l 0 'AI - l l l 7 4 5 1 2 6 3 Minimal Cross-Sectional Area (mme Vol. 73, No. 3, March 1986 471 JOHNSON et al. 6 Quantitative Coronary Angiography N=7 Minimal Cross Sectional Area (mm2) 4 ~r 2 0 20 Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016 Integrated Optical Density --- 1,~~~ 1 Before Immediately Follow PTCA After PTCA up Videodensitometry N=6 15 *1* 10 rt~~~-- 5 0 5 a 5 i Before Immediately Follow up PTCA After PTCA FIGURE 4. Coronary lumen sizes for group B patients before PTCA, immediately after PTCA, and at follow-up, defined by quantitative coronary angiography (top) and videodensitometry (bottom). 'p = NS compared with integrated optical density immediately after PTCA. ents, ' improved symptomatic and electrocardiographic response to exercise,24 fewer myocardial perfusion defects on thallium-201 scintigraphy,24 25 improved left ventricular diastolic filling velocity,26 and normalization of exercise-induced wall motion abnormalities on the radionuclide ventriculogram.27' 28 This study provides additional objective documentation of the results of angioplasty by defining in absolute terms, using two methods of computer-assisted analysis of coronary angiograms (quantitative coronary angiography and videodensitometry), the change in area of the lumen that occurs during and after angioplasty. In this study, as in previous studies,3-' we found that approximately one-third of lesions (35% in our study) restenose during the follow-up period. Importantly, however, 35% of our patients (group A) showed a late increase in area of the lumen over the period of followup. Indeed, the amount of increase in lumen area during follow-up was substantial, in three cases surpassing the change in area from before to immediately after angioplasty. This late increase in lumen area in onethird of the patients after dilation is particularly intrigu472 ing since studies of the natural history of untreated atherosclerotic lesions using quantitative coronary angiography have shown that only 4% of lesions spontaneously regress during a similar time period.'8 Although computer-assisted quantitative coronary angiography is of greater reliability and accuracy than visual angiographic estimates, this technique nonetheless relies on drawing of vessel borders from an unenhanced cineangiographic image. Casual inspection suggests that detection of the coronary lesion edge may be especially problematic immediately after PTCA when the vessel edge is indistinct." '1 However, in our study the interobserver variability immediately after PTCA was the same as that at follow-up, suggesting that edge definition, at least with the high-quality and greatly magnified angiograms on which we performed quantitative coronary angiography, may not represent a greater problem immediately after PTCA than at other times. In the future, the development of digital image acquisition and newer computer techniques of edge detection and enhancement may minimize any border recognition difficulties that do exist. Quantitative Coronary Angiography 6 Minimal Cross- Sectional Area (mm2) N=8 4 2 0 m a . I a -F --1ma Before Immediately Follow PTCA After PTCA up 20 Integrated Optical Density Videodensitometry 15 10 5 0 Before Immediately Follow PTCA After PTCA up FIGURE 5. Coronary lumen sizes for group C patients before PTCA, immediately after PTCA, and at follow-up, defined by quantitative coronary angiography (top) and videodensitometry (bottom). t p = NS compared with integrated optical density immediately after PTCA. CIRCULATION THERAPY AND PREVENTION-PTCA Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016 For the present, however, the agreement seen between results obtained by quantitative coronary angiographic analysis and those obtained by videodensitometric analysis, a procedure that depends less on exact definition of vessel edges, strengthens the conclusions of our study. We found no differences in hemodynamic, quantitative angiographic, or videodensitometric characteristics of coronary lesions in the three patient subgroups before or immediately after angioplasty. Specifically, the transstenotic pressure gradient, the minimal crosssectional area, and the integrated optical density of the lesion before and immediately after angioplasty did not significantly differ among the three groups in which there were markedly disparate late outcomes. The change in size of the lumen during follow-up also could not be predicted by the presence or absence of recognized coronary risk factors. We noted a similar incidence of recurrent chest pain among patients in all groups, despite the fact that the average minimal crosssectional area of the lesion at follow-up was significantly greater in groups A and B than in group C. The reason for recurrent chest pain in group A and B patients despite the preservation of size of the coronary lumen is unclear, but could relate to the activity level of the patient, to vasospasm, or to the lack of a suitable functional assessment of coronary vasodilator reserve. Of more concern is the absence of angina in 50% of group C patients despite significant restenosis - restenosis that could be treated with repeat PTCA but that was not clinically apparent before routine followup angiography. Thus, we found no clinical or quantitative angiographic characteristics that could predict the late outcome of a patient with a successfully dilated coronary segment. Mechanism of dilation in PTCA. Despite evidence of decreased lesion severity and improved myocardial perfusion after PTCA, there is not widespread agreement regarding its underlying mechanism. Initially it was assumed that simple compression of atheroma resulted in an immediate increase in lumen size.29 Subsequent experimental evidence suggested focal intimal fractures30' 31 and overstretching of elastic fibers in the vessel wall32 as possible mechanisms. Our finding that the cross-sectional area of dilated lesions immediately after PTCA is less than the cross-sectional area of the inflated balloon suggests that vascular stretching occurs during dilation that is followed by elastic recoil. However, the fact that one-third of successfully dilated lesions show a substantial further increase in size of the lumen during late follow-up without further balloon inflations shows that vascular stretching is not the only Vol. 73, No. 3, March 1986 mechanism of improvement after PTCA. If the effects of angioplasty were related only to vascular stretching and the magnitude of the lumen area achieved after balloon removal, we would expect that the area would remain unchanged during late follow-up (as occurred in 30% of our patients), or perhaps show evidence of restenosis (if the atherosclerotic process continued or were accelerated). Late improvement in size of the lumen is thus unexpected. We speculate that two mechanisms may be involved. First, coronary vasospasm may occur in some patients immediately after dilation, despite the use of vasodilating agents. The late increase in cross-sectional area of the lumen at follow-up would then represent resolution of spasm at the site of dilation. Second, pathologic studies have indicated that fracture of intimal plaque often occurs at the time of successful dilation.30' 31 During the followup period, retraction of the intimal flap with fibrosis and endothelial healing could result in an increased lumen size33 if excessive platelet deposition or accelerated atherosclerosis did not occur. Quantitative analysis of coronary stenoses. Serruys et al.34 have also used quantitative angiographic and videodensitometric techniques to analyze coronary lesions before and after angioplasty. However, these authors emphasized lesion analysis with the use of percent stenosis and diameter measurements rather than absolute cross-sectional area of the lumen. Although of importance in understanding the physiologic significance of coronary stenoses in general,12' 13 calculation of the minimal cross-sectional area of lesions after PTCA is especially critical. The relationship between the position of the lesion and the dilating balloon during angioplasty is often imprecise. Since multiple dilations in slightly varying positions are usually performed, late changes in percent stenosis may reflect changes in the dilated lesion, the adjacent dilated "normal" segment, or both. We have previously shown that significant changes in the cross-sectional area of the adjacent "normal" segment occur during late followup.16 Therefore, it is likely that only an absolute measurement of coronary cross-sectional area can yield quantitative information regarding progression or regression of the dilated lesion during follow-up. Limitations of the study. There are several potential limitations of this study. First, the sample size was small and represented our initial experience with angioplasty. Despite the small sample size, however, the series was consecutive and a high proportion of patients (83%) returned for follow-up angiograms. Although steerable catheter systems have increased the primary success rate of angioplasty, we have no reason 473 JOHNSON et al. Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016 to postulate that this would have exerted a major influence on the late outcome after PTCA. Changes in dilation parameters (either inflation pressure or duration) could influence the results, but these changes have not influenced the restenosis rate, and thus would be unlikely to alter our results. There were major differences in the drugs the patients received at the time of the two catheterizations. Vasodilators were used more frequently and in larger doses during the dilation procedure than at the time of follow-up angiography. This does not, however, preclude the possibility of angioplasty-induced vasospasm immediately after PTCA, with subsequent release of vascular tone over time. Indeed, if vasodilator therapy had been comparable during PTCA and at follow-up, minimal areas of the lumen at follow-up may have been even larger, resulting in more patients in groups A and B and fewer in group C. Clinical implications. Our findings may be clinically important in the management of patients after PTCA. Because stenosis resistance is primarily dependent on the fourth power of the radius of the lesion at its narrowest point, even a small late change in area of the lumen may result in a change in coronary flow sufficient to alter a patient's symptomatology or objective evidence of ischemia. Thus, the adequacy of coronary dilation should not be judged solely on immediate changes in the gradient or angiographic appearance, or even on the minimal cross-sectional area of the dilated lesion immediately after PTCA. Our results also indicate that noninvasive tests performed soon after PTCA (e.g., graded exercise testing, myocardial scintigraphy, and exercise-gated radionuclide ventriculography) should be interpreted cautiously with regard to predicting the long-term success of the dilation. Since neither the hemodynamic nor the angiographic characteristics of the lesions immediately after PTCA nor the clinical characteristics of the patients during follow-up seem to be able to predict restenosis, at the present time a follow-up angiographic study appears to be needed in most instances. Finally, our results confirm a variable late outcome after initially successful PTCA - an outcome that may be susceptible to manipulation by improved angioplasty techniques or the use of pharmacologic agents. Controlled trials of different dilation techniques, as well as of antiplatelet agents and other therapies that might minimize restenosis, with quantitative angiographic follow-up are needed to further investigate these possibilities. We thank Janice Ripley and Kyle Snowden for technical assistance and Jill Christy for preparation of the manuscript. 474 Data analysis was performed with "Clinfo" (supported by grant RR59 from the Clinical Research Centers Branch, NIH). References 1. Gruntzig AR, Senning A, Siegenthaler WE: Nonoperative dilatation of coronary artery stenosis. N Engl J Med 301: 61, 1979 2. Kent KM, Bentivoglio LG, Block PC, Cowley MJ, Dorros G, Gosselin AJ, Gruntzig A, Myler RK, Simpson J, Stertzer SH, Williams DO, Fisher L, Gillespie MJ, Detre K, Kelsey S, Mullin SM, Mock MB: Percutaneous transluminal coronary angioplasty: Report from the registry of the National Heart, Lung, and Blood Institute. Am J Cardiol 49: 2011, 1982 3. Hollman J, Gruentzig A, Meier B, Bradford J, Galan K: Factors affecting recurrence after successful coronary angioplasty. J Am Coll Cardiol 1: 644, 1983 (abst) 4. Guiteras-Val P, David PR, Lesperance J, Dangoisse V, Crepeau J, Dyrda I, Bourassa MG: Clinical and angiographic follow-up of successful percutaneous transluminal coronary angioplasty (PTCA). Circulation 66(suppl II): 11-330, 1982 (abst) 5. Jutzy KR, Berte LE, Alderman EL, Ratts J, Simpson JB: Coronary restenosis rates in a consecutive patient series one year post successful angioplasty. Circulation 66(suppl II): 11-331, 1982 (abst) 6. Engel HJ, Kaltenbach M, Kober G, Scherer D, Lichtlen PR: Spontaneous regression of coronary obstructions after transluminal dilatation. Circulation 62(suppl III): III-159, 1980 (abst) 7. Holmes DR, Vlietstra RE, Smith HC, Vetrovec GW, Cowley MJ, Kent KM, Detre KM, Myler R: Restenosis following percutaneous transluminal coronary angioplasty (PTCA): a report from the NHLBI PTCA registry. Am J Cardiol 49: 905, 1982 (abst) 8. Detre KM, Wright E, Murphy ML, Takaro T: Observer agreement in evaluating coronary angiograms. Circulation 52: 979, 1975 9. Zir LM, Miller SW, Dinsmore RE, Gilbert JP, Harthorne JW: Interobserver variability in coronary angiography. Circulation 53: 627, 1976 10. DeRouen TA, Murray JA, Owen W: Variability in the analysis of coronary arteriograms. Circulation 55: 324, 1977 11. Galbraith JE, Murphy ML, deSoyza N: Coronary angiogram interpretation. Interobserver variability. JAMA 240: 2053, 1978 12. White CW, Wright CB, Doty DB, Hiratzka LF, Eastham CL, Harrison DG, Marcus ML: Does visual interpretation of the coronary arteriogram predict the physiologic importance of a coronary stenosis? N Engl J Med 310: 819, 1984 13. Harrison DG, White CW, Hiratzka LF, Doty DB, Barnes DH, Eastham CL, Marcus ML: The value of lesion cross-sectional area determined by quantitative coronary angiography in assessing the physiologic significance of proximal left anterior descending coronary arterial stenoses. Circulation 69: 1111, 1984 14. Johnson MR, Fleagle SR, Aylward PE, Collins SM, Skorton DJ, Hiratzka LF, Harrison DG. White CW, Marcus ML: Digital processing and analysis of coronary cineangiograms: Geometric and physiological assessment of coronary stenosis. Circulation 70(suppl II): II-324, 1984 (abst) 15. Holmes DR, Vlietstra RE, Mock MB, Reeder GS, Smith HC, Bove AA, Bresnahan JF. Piehler JM, Schaff HV, Orszulak TA: Angiographic changes produced by percutaneous transluminal coronary angioplasty. Am J Cardiol 51: 676, 1983 16. Brayden GP, Harrison DG, Marcus ML, White CW: Changes in the adjacent normal coronary segment preclude use of % stenosis to quantitate late coronary lesion changes following PTCA. Clin Res 31: 702A, 1983 (abst) 17. Brown BG, Bolson E, Frimer M, Dodge HT: Quantitative coronary arteriography: estimation of dimensions, hemodynamic resistance, and atheroma mass of coronary artery lesions using the arteriogram and digital computation. Circulation 55: 329, 1977 18. Brown BG, Bolson EL, Dodge HT: Arteriographic assessment of coronary atherosclerosis. Review of current methods, their limitations, and clinical applications. Arteriosclerosis 2: 2, 1982 19. Sandor T, Als AV, Paulin S: Cine-densitometric measurement of coronary arterial stenoses. Cath Cardiovasc Diagn 5: 229, 1979 20. Collins SM, Skorton DJ, Harrison DG, White CW, Eastham CL, Hiratzka LF, Doty DB. Marcus ML: Quantitative computer-based videodensitometry and the physiological significance of a coronary stenosis. In IEEE Computer Society: Computers in cardiology. Long Beach, CA, 1982, p 219 CIRCULATION THERAPY AND PREVENTION-PTCA Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016 21. Collins SM, Johnson MR, Ericksen EE, Fleagle SR, Hiratzka LF, Harrison DG, White CW, Skorton DJ: Videodensitometric analysis of coronary stenoses: methodological considerations and geometric and functional validation. Circulation 70(suppl II): 11-30, 1984 (abst) 22. Judkins MP: Selective coronary arteriography. Part I: A percutaneous transfemoral technic. Radiology 89: 815, 1967 23. Reiber JHC, Slager CJ, Schuurbiers JCH, denBoer A, Gerbrands JJ, Troost GJ, Scholts B, Kooijman CJ, Serruys PW: Transfer functions of the x-ray cine video chain applied to digital processing of coronary cineangiograms. In Heintzen PH, Brennecke R, editors: Digital imaging in cardiovascular radiology. Stuttgart, 1983, George Thieme Verlag, p 89 24. Scholl JM, Chaitman BR, David PR, Dupras G, Brevers G, Guiteras Val P, Crepeau J, Lesperance J, Bourassa MG: Exercise electrocardiography and myocardial scintigraphy in the serial evaluation of the results of percutaneous transluminal coronary angioplasty. Circulation 66: 380, 1982 25. Hirzel HO, Nuesch K, Gruentzig AR, Luetolf UM: Short- and long-term changes in myocardial perfusion after percutaneous transluminal coronary angioplasty assessed by thallium-201 exercise scintigraphy. Circulation 63: 1001, 1981 26. Bonow RO, Kent KM, Rosing DR, Lipson LC, Bacharach SL, Green MV, Epstein SE: Improved left ventricular diastolic filling in patients with coronary artery disease after percutaneous transluminal coronary angioplasty. Circulation 66: 1159, 1982 27. Kent KM, Bonow RO, Rosing DR, Ewels CJ, Lipson LC, McIn- Vol. 73, No. 3, March 1986 tosh CL, Bacharach S, Green M, Epstein SE: Improved myocardial function during exercise after successful percutaneous transluminal coronary angioplasty. N Engl J Med 306: 441, 1982 28. Sigwart U, Grbic M, Essiner A, Bischof-Delaloye A, Sadeghi H, Rivier JL: Improvement of left ventricular function after percutaneous transluminal coronary angioplasty. Am J Cardiol 49: 651, 1982 29. Dotter CT: Transluminal angioplasty pathologic basis. In Zeitler E, Gruntzig A, Schoop W, editors: Percutaneous vascular recanalization. Technique. Application. Clinical results. Berlin, 1978, Springer-Verlag, p 3 30. Baughman KL, Pasternak RC, Fallon JT, Block PC: Transluminal coronary angioplasty of postmortem human hearts. Am J Cardiol 48: 1044, 1981 31. Freudenberg H, Wefing J, Lichtlen PR: Risks of transluminal coronary angioplasty. A postmortal study. Circulation 58(suppl II): II80, 1978 (abst) 32. Castaneda-Zuniga WR, Formanek A, Tadavarthy M, Vlodaver Z, Edwards JE, Zollikofer C, Amplatz K: The mechanism of balloon angioplasty. Radiology 135: 565, 1980 33. Block PC: Percutaneous transluminal coronary angioplasty. Am J Roentgenology 135: 955, 1980 34. Serruys PW, Reiber JHC, Wijns W, Brand Mvd, Kooijman CJ, tenKaten HJ, Hugenholtz PG: Assessment of percutaneous transluminal coronary angioplasty by quantitative coronary angiography: diameter versus densitometric area measurements. Am J Cardiol 54: 482, 1984 475 Changes in cross-sectional area of the coronary lumen in the six months after angioplasty: a quantitative analysis of the variable response to percutaneous transluminal angioplasty. M R Johnson, G P Brayden, E E Ericksen, S M Collins, D J Skorton, D G Harrison, M L Marcus and C W White Downloaded from http://circ.ahajournals.org/ by guest on September 29, 2016 Circulation. 1986;73:467-475 doi: 10.1161/01.CIR.73.3.467 Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231 Copyright © 1986 American Heart Association, Inc. All rights reserved. Print ISSN: 0009-7322. Online ISSN: 1524-4539 The online version of this article, along with updated information and services, is located on the World Wide Web at: http://circ.ahajournals.org/content/73/3/467 Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for which permission is being requested is located, click Request Permissions in the middle column of the Web page under Services. Further information about this process is available in the Permissions and Rights Question and Answer document. Reprints: Information about reprints can be found online at: http://www.lww.com/reprints Subscriptions: Information about subscribing to Circulation is online at: http://circ.ahajournals.org//subscriptions/