Respiratory system measurement
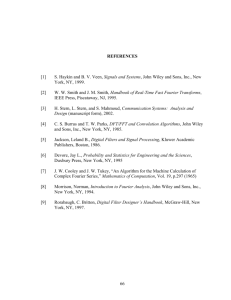
advertisement

(bx•Qb)in PPL Ubx (AWOx •QAWO)in VA (a) PA QAWO AWO (bx•Qb)out VL (b) Figure 9.1 Models of the lungs (a) basic gas-transport unit of the pulmonary system. Here (x Q) is the molar flow of X through the airway opening, AWO, and the pulmonary capillary blood network, b. Ubx is the net rate of molar uptake –that is, the net rate of diffusion of X into the blood. VD and VA are the dead-space volume and alveolar volume, respectively. (b) A basic mechanical unit of the pulmonary system. PA is the pressure inside the lung – that is, in the alveolar compartment. PPL and PAWO are the pressures on the pleural surface of the lungs and at the airway opening, respectively. VL is the volume of the gas space within the lungs, including the airways; QAWO is the volume flow of gas into the lungs measured at the airway opening. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. pAWO CstW RAW RAW L qAWO pA CstL L CstL qAWO pPL pPL pAWO pA CstW pBS pMUS + pMUS pBS (a) (b) Figure 9.2 Models of normal ventilatory mechanics for small-amplitude, low-frequency (normal lungs, resting) breathing (a) Lung mechanical unit enclosed by chest wall. (b) Equivalent circuit for model in Figure 9.2(a). © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. Figure 9.3 Pneumotachometer flow-resistance elements (a) Screen. (b) Capillary tubes or channels. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. Figure 9.4 Pneumotachometer for measurements at the mouth (a) Diameter adapter that acts as a diffuser. (b) An application in which a constant flow is used to clear the dead space. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. Figure 9.5 Volume ranges of the intact ventilatory system (with no external loads applied). TLC, FRC, and RV are measured as absolute volumes. VC, IC, ERV and VT are volume changes. Closing volume (CV) and closing capacity (CC) are obtained from a single-breath washout experiment. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. Rotational displacement sensor Other signal processing Strip-chart recorder Counterweight Kymograph Bell Water seal One-way valves PS TS FS x VS Uabs Mouthpiece Soda-lime canister Thermometer for spirometer gas temperature TL PA QAWO Spirometer system Blood flow VL Ubs FA x Pulmonary system Figure 9.6 A water-sealed spirometer set up to measure slow lung-volume changes. The soda-lime and one-way-valve arrangement prevent buildup of CO2 during rebreathing. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. 100% O2 One-way valves TS TL VL FSN2 Spirometer FAN2 VS O2 + N2 + CO2 Nitrogen analyzer Figure 9.7 Diagram of an N2 washout experiment The expired gas can be collected in a spirometer, as shown here, or in a rubberized-canvas or plastic Douglas bag. N2 content is then determined off-line. An alternative is to measure expiratory flow and nitrogen concentration continuously to determine the volume flow of expired nitrogen, which can be integrated to yield an estimate of the volume of nitrogen expired. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. (dPM)0 (dPB)0 (PM Patm ) PM Shutter closed PB Shutter Figure 9.8 A pressure-type total-body plethysmography is used with the shutter closed to determine lung volume and with the shutter open to determine changes in alveolar pressure. Airway resistance can also be computed if volume flow of gas is measured at the airway opening. Because atmospheric pressure is constant, changes in the pressures of interest can be obtained from measurements made relative to atmospheric pressure. QAWO QAWO VL PA TL NL -QAWO dQAWO dPB Shutter open VB PB TB NB Pump VP PB (PB –Patm) Calibration VP VP = PB BPB © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. PB V L TLC Less stiff Normal TLC Normal VC Normal VC FRC RV Slope of linear approximation to curve (static compliance) VT Normal FRC TLC VC FRC Normal RV Stiffer lung RV PL = PAWO –PPL Figure 9.9 Idealized statically determined expiratory pressure-volume relations for the lung. The positions and slopes for lungs with different elastic properties are shown relative to scales of absolute volume and pressure difference. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. -QAWO (Expiration) VL TLC VL < 0.8 TLC (Inspiration) (PAWO –PA) Figure 9.10 Idealized isovolume pressure-flow curves for two lung volumes for a normal respiratory system. Each curve represents a composite from numerous inspiratory-expiratory cycles, each with successively increased efforts. The pressure and flow values measured as the lungs passed through the respective volumes of interest are plotted and connected to yield the corresponding curves. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. QAWO Maximal expiratory Flowvolume (MEFV) curves (Expiration) Effort independent TLC (FVC QAWOdt) TLC Reduced FVC Normal FVC Effort independent 0 1 2 3 4 Time vital capacity (TVC) spirograms Time, s Figure 9.11 Alternative methods of displaying data produced during a forced vital capacity expiration. Equivalent information can be obtained from each type of curve; however, reductions in expiratory flow are subjectively more apparent on the MEFV curve than on the timed spirogram. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. Figure 9.12 Essential elements of a medical mass spectrometer. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. Figure 9.13 General arrangements of the components of an infrared spectroscopy system. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. Figure 9.14 N2 analyzer employing emission spectroscopy. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. Readout scale Light source Sample in A Pressure sensor D F J E Magnets Dumbbell-shaped test body Point of suspension (a) B (b) Figure 9.15 Oxygen analyzers (a) Diagram of the top view of a balance-type paramagnetic oxygen analyzer. The test body either is allowed to rotate (as shown) or is held in place by counter torque, which is measured to determine the oxygen concentration in the gas mixture. (b) Diagram of a differential pressure and a magneto-acoustic oxygen analyzer (see text for descriptions). © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. C Figure 9.16 Distributions of volume and gas species at RV and TLC for a vital-capacity inspiration of air or pure oxygen. © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998. Conducting airway filled with 100% O2 Well-mixed alveolar compartment (a) Figure 9.17 single-breath nitrogen-washout maneuver (a) An idealized model of a FEN2 lung at the end of a vitalcapacity inspiration of pure O2, preceded by breathing of normal air. (b) Single-breath N2-washout curves for idealized lung, normal lung, and abnormal lung. Parameters of these curves include anatomical dead space, slope of phase III, and closing volume. Normal slope 0.02/500 ml Ideal lung Abnormal slope >0.02/500 ml Normal lung I II III Abnormal lung 0 750 1250 IV CV Expired volume, vS (ml) Anatomical dead space volume, V' D TLC Lung volume, vL RV (b) © From J. G. Webster (ed.), Medical instrumentation: application and design. 3rd ed. New York: John Wiley & Sons, 1998.