An Approach to the Patient with Vertigo Cynthia Phelan PGY 1
advertisement

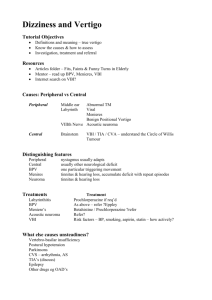
An Approach to the Patient with Vertigo Cynthia Phelan PGY 1 2003 10 23 Vertigo A false sense of moving or spinning or of objects moving or spinning, usually accompanied by nausea and loss of balance. Chief Complaint: “Dizziness” Vertigo Light Headedness Weakness Faintness Mental Confusion Headache Gait disorder Paresthesias Abnormalities of Auditory Canal • • • Benign Paroxysmal Positional Vertigo Labyrinthitis Otitis Interna Herpes zoster Meniere`s disease Vestibular nerve inflammation Trauma Neurologic • Multiple sclerosis Neoplasm Migraine Circulatory CVA Vertebrobasilar insufficiency Trauma Skull # with labyrinth injury Psychiatric • Panic disorder Pharmacological • • Alcohol Aminoglycosides Illicit drugs Environmental • Motion sickness History Description of symptoms Timing Onset, duration, frequency, diurnal variation Positional Dependence Associated symptoms Alleviating and Aggravating Factors Past Medical History Medications Recent trauma. Risk Factors for Causes of Central Vertigo Physical Exam Vitals Pay attention to BP (orthostatic) and Pulse HEENT EOMs - NYSTAGMUS Hearing CVS Rate, rhythm, bruits, murmurs Neurologic Cranial nerves Reflexes Cerebellar Exam Gait Proprioception Peripheral Vertigo Central Vertigo Associated Symptoms Nausea & vomiting, diaphoresis Associated Symptoms - Neurologic Diplopia, dysphagia, facial numbness, ataxia, hemiparesis Auditory Complaints - tinnitus, hearing loss Auditory Complaints - infrequent Intense Symptoms Less Intense Symptoms Abrupt onset Gradual Onset Association with head trauma Not Usually Associated with Head Trauma Nystagmus Horizontal or Rotary by gaze fixation Direction constant Nystagmus Vertical or Multidirectional by gaze fixation Varies with direction of gaze Causes of Peripheral Vertigo • BPV Due to deposition of calcium carbonate crystals in the posterior semi-circular canal Repeated attacks of vertigo lasting a few seconds Aggravated by changes in posture, typically turning ones head while lying in bed No hearing loss or tinnitus Usual onset in the 60s – 70s Dix-Hallpike diagnostic and often therapeutic Rotary nystagmus Rx – Gravol, eply maneuver Causes of Peripheral Vertigo • Labyrithitis Viral infection of labyrinth, rarely associated with otitis media Severe vertigo associated with hearing loss Tx - Self limited, Gravol, decongestants • Meniere`s Disease Due to endolymphatic system dilation and degeneration of cochlear hair cells. Recurrent attacks of severe vertigo, vomiting and tinnitus Associated with progressive deafness Typical presentation is patient with progressive hearing loss who develops sudden severe attacks of vertigo which last for 30min to several hours before abating severity and frequency of attacks decrease as deafness increases Tx - Bed rest acutely, ENT, surgical ablation of labyrinth Peripheral Vertigo • Vestibular Neuronitis • Illness of suspected viral origin, may be mild encephalitis usually follows URTI Vertigo without hearing loss +/- tinnitus Abnormal caloric testing Tx - Time limited, residual symptoms may last for weeks. Vestibulococclear Nerve Lesions, CP angle tumors Acoustic schwannomas, meningiomas Preceded by hearing loss, associated neurologic symptoms ipsilateral corneal reflex impairment, facial weakness, cerebellar signs Patients complain of unsteadiness more than vertigo Tx – Neurology / Neurosurgery consult Causes of Central Vertigo 1. Cerebellar Hemorrhage or infarction 2. Vertigo, ataxia, headache May have conjugate eye deviation to the opposite side of the lesion Patients unable to maintain body position Neurology consult and MRI/CT head STAT Brainstem 3. Infarction or hemorrhage of brainstem produces vertigo as one of a large constellation of symptoms...dysphagia, dysphonia, facial numbness, absent corneal reflex, ipsilateral Horner`s, deficits in CN VI, VII, VIII. STAT neurology/neurosurgery consult…often little can be done for these patients Prognosis poor Multiple Sclerosis Vertigo can be produced by demyelinating lesions in the brainstem Vertigo is the presenting symptom in 5% of cases MISC Disequilibrium Syndrome ill-defined dizziness resulting from multiple sensory abnormalities Usually in elderly Hyperventilation Syndrome Anxiety Near Syncope, hypoglycemia Migraine Aura Drugs / Ototoxins Aminoglycosides, saliculates, ethanol, phenytoin, quinine, benzene, arsenic Treatment Therapy depends on the etiology of the vertigo. 1. Symptomatic relief Rehydration - esp. in patients with vomiting and the elderly Bed rest in comfortable position Medications for symptomatic relief antihistamines, anticholinergics, antiemetics and benzodiazapies 2. Eply Maneuver for BPPV First Dix-Hallpike test performed – patient’s head rotated 45 degrees to the right Once nystagmus stops, rotate head until body is face down (hold 10-15 sec) Bring patient back to seated position with head turned over left shoulder 80% success rate in BPV 3. Reassurance…symptoms of vertigo though distressing are usuall benign and self limited. Take Home Points 1. Determine what the patient’s symptoms truly are – vertigo vs lightheadedness 2. Central vs Peripheral origin 3. Symptomatic treatment for benign, selflimited conditions 4. Referral for any suspected intracranial lesions