Document 17954105
advertisement

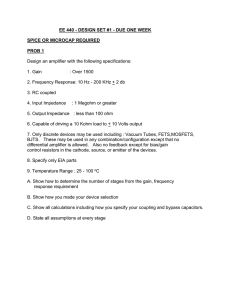
>> Gabe Cohn: Yeah, alright, so I’d like to … I’m really excited to introduce our speakers today. We have four researchers who’ve come all the way from Lübeck, Germany, and they seem to be awake at the moment—so that’s good. So our speakers today are Steffen and Ankit, and we have their colleagues also in the room: Roman and Gunther. And they… each of them has a little bit different background, either in electrical engineering or may … biological … >>: Biomedical. >> Gabe Cohn: … biomedical engineering. And they’ve come together to build some really interesting hardware systems that look at making really precise and accurate measurements of electrical signals in the body. And so they’re gonna talk today about one of their systems that looks at biological impedance, as well as some of the other researcher … research that they’ve done in their lab. So I’ll let you go ahead and get started. Thanks a lot. >> Steffen Kaufmann: Yes, hello, everybody. Thank you, Gabe, for the nice introduction. I’m going to speak about a high-accuracy bioimpedance measurement system for time-resolved measurements, and I also will give an outlook about the campus we have at Lübeck and other ongoing research at … project in our lab. And let me start with what is brand new in Lübeck; we have this BioMedTec campus—it’s called Wissenschaftscampus—so something of research campus we have in Lübeck, and the marketing argument is: “A strong alliance between science and industry” and “A long-term cooperation becomes institutionalized.” What does it mean? It mean we have research on campus, and seven members of the BioMedTec campus are, for example, the University of Lübeck, the Lübeck University of Applied Science—they’re the two universities we have in Lübeck which sharing one big campus—and we have the Research Center in Borstel; we have the Fraunhofer MEVIS image reconstruction group; we have a few companies—like EUROIMMUN, and Fraunhofer EMB, and also Möller-Wedel—which work all on this campus and have all researchers on this campus in Lübeck. And we have—for this BioMedTec campus—there are some services which are so-called co-apten … co-opted campus partners, for example: the Medisert company, the FHL research company, then there’s Olympus Winter and Ibe again is part of this partners, as well as Oncampus, the Technology Center Lübeck—which is mainly facilities— the Chamber of Industry and Commerce, and also the university clinics of Lübeck. Through all this cooperation partners, we have teaching synergies through coordinated course structures on the BioMedTec. It’s all connected by biomedical engineering, and you may know by … biomedical engineering is in fact electrical engineering, mechanical engineering, and medicine. We also have medicine courses there—we can also study on human medicine at Lübeck—and medical engineering science, and so on, so forth. A few clusters we have in … at the BioMedTec campus are the clinic cell technology, the medical software and system engineering group, and the … a group we are all come from is TANDEM—so the Center of Excellence for Technology and Engineering in Medicine—and we also have the Smart City research group—a research center—and the software systems engineering group. All it’s coordinated on a … in a way, as a commercialization is over the Medisert company, which is a corporation of the … both universities, and the share is about seventy-five percent university and twenty-five percent University of Applied Science, and it’s some kind of a contact point to industry over this company. And they’re also doing the … all of the back-office for the Center of Excellence for Technology and Engineering in Medicine. Yeah, and they also do some service agency stuff, like conference measurement … management, travel management, et cetera. And to focus on biomedical engineering, on TANDEM: TANDEM is the bundle of expertise and know-how in the field of medical engineering from the both universities, and we have about twenty institution involved—so the twenty different institutes—from medical engineering over physics to electronics. And where we directly come from: from all this different spots here is the LME, which is the Laboratory for Medical Electronics, and we are focusing on a noninvasive measurements of cardiovascular parameters. In fact, you see a program or patient on the left side, and then you have easy, acquirable signals, like ECG, like the photoplethysmogram, or also the impedance signal—where we will focus today. And it’s all about the heart, the center, and the different modalities which you can acquire to estimate different parameters of the body and the state of healths. Okay, let’s start now with the talk I promised. Let me first introduce a bit what is electrical impedance, because I was told that the audience is mainly computer science, so I want to start a bit with the basic of: what is electrical impedance? Electrical impedance—as you … what you may know from school—is the opposion which a current gets when it’s traversed through a resistance, and this is the normal DC definition; the AC definition is pretty much the same. You have the complex impedance Z, which is defined by the division of the complex voltage and the complex current, and you may see on the figure what a typical measurement so could look like. You have an excitation source; you have a resistor; you have … you put a voltage—or a current—through the resistor; and either current or voltage can be measured. And when you do this not for a single frequency or for DC, you only do it over complete spectrum, then it’s called impedance spectroscopy. And when you switch from electrical impedance to bioimpedance, you can think about that bioimpedance is just the electrical impedance of living tissue, and it’s proved to be a vital tool in life science and in biomedical engineering, because it can tell you a lot of information about the structure and the composition of the tissues you are investigating. And what is well known is, maybe, the body composition estimation when you’re … when you have a weight scale, or there’s also blood flow estimations and a cardiac cycle—not cardiac cycle—cardiac output estimations possible, based on impedance measurements. And the best thing about it: it’s noninvasive, and it’s has no known hazards, as long as you follow the rules of the IEC 60601’s in terms of: you limit the maximum current you apply. And therefore it has a high clinical acceptation. So where does the electrical impedance come from? The electrical impedance comes from—basically— from the cells. I … you can see here an equivalent circuit. I’m … no, it’s not … no, it does not have an … >>: Fingerpoint [indiscernible] >> Steffen Kaufmann: Yeah, and fingerpoint, yes. Although basically, you see here the cell—a single cell, a human cell—and the equivalent circuit, and you have the cell membrane, which behaves pretty much like a lossy capacitor—you have a capacitor and a resistor shunting in parallel. Then you have the inner part of the cell, which is basically an resistor [indiscernible] and then you have another membrane. And when you go from one cell to a bunch of cells, you would also have some extra cell liquid which is also assumed to be resistive. Of course, this is a pretty basic equivalent circuit, but in the frequency range from about ten kilohertz to four hundred kilohertz, this is pretty good-fitting—which is also the range where you will get the most information about the cell composition or the tissue composition. And this is called beta dispersion—this pera … this range. But when you want to measure bioimpedance, you have two problems: that you somehow get access to the body, and you have to have an interface between the ion conduction inside the body and the electrical contact … the electron conduction outside the body. For that, you need electrodes, and electrodes create, in connection with the body, the so-called electrode-skin impedance, and the electrode-skin impedance pretty much behaves also like the tissue—has the same equivalent circuit or an comparable equivalent circuit. You have a Cp and Rp, and then you have the series resistance Rs—which representing a different effects when you have the electrodes attached. So you have … there are the skin layers, and then you have the electrode layers, and then you have a ham hall stopper layer in between, and therefore, you also have a voltage, because you have an … a developing half-cell potential. And the big problem with the electrical … electrode-skin impedance is that it’s variable; it is comparable big; and it changed when you … with movement—so it’s not constant. And a typical value for that—for example—at twenty ohm at about three hundred kilohertz with good electrodes, but it can also be two kilo-ohm at low frequencies when you have a bad electrode—so the loose-fitting electrodes or electrodes which used to be wet, but then become dry, for example. So you have the basic measurement problem when you have electrodes: so we have the impedance we want to measure here—ZT for Z tissue—and you have the two electro-impedances, and when you think about what you now have is when I told you ZE1 and ZE2 are much bigger that ZT, you make a big measurement error. And you just have two point measurement, and you want to estimate the tissue impedance. And to get around this, there’s a standard method; it’s the so-called four electrode setup. In the four electrode setup, you don’t only have two electrodes, you have four electrodes, and in the inner electrode, you measure the voltage, and the outer electrodes you use to push a current through the tissue, and then you can measure the voltage drop above the tissue or across the tissue. And with that, you can pretty good … estimate a pretty good measure the tissue impedance you’re interested in. When you think about a possible measurement setup, you will come to an equivalent circuit which, more or less, look like this. You have—on the top left—you have the current source, which is modelled as an real current source … as an ideal current source with two parasitic components—a resistor and a capacitor—which limit the output impedance of this current source. Then you see ZE1, which represent one electrode—the current electrode. Then you see—when you go from top to bottom—you have the tissue impedance, which is here named Z, and you have another electrode where it camps out, and—the current out—and then you have an … a shunt resistor for measuring the current. So when you look at this slide, it’s exactly … so we have the current source, the two electrodes, and what is extra is now the shunt resistor. And from the shunt resistor, you have just an … a measurement block which measures the voltage across the shunt resistor. When you know the shunt resistor in size and value, you can then calculate the current, and for the voltage measurement—here, in this case—is a programmable gain amplifier. You have the other two electrodes for the voltage measurement, and here, what is crucial is you have here, also, parasitics—R and C—which are mainly composed of the cables you use. So you have the electrodes; you have some measurement equipment; but you need a cable in between, and normally, you want to use a shielded cable—so unshielded cable has a capacity, so you add a capacity. Additionally—sorry—you have the PGA; the PGA is also not ideal and will also have some input capacities and some input resistances. And you may see here on a first glance, you may then get a problem here—you could do … build a voltage divider between this point and this point—and as lower as this impedance become, as more voltage rub you will have on the electrodes, and this lead to measurement error. And the measurement error is a function of the electrode impedance, and in … of the input capacity, mainly of the PGA—so also the cable impedance is important. And when you think about: you have about thirty pikofarad cable impedances, and you can make the—there’s a bit maths and a bit analyzing of the circuits—you can formulate this equation, which gives you the measured impedance, ZM, as a function of the real impedance, Z, multiplied with the two error terms which represent the voltage error—so the error that you make at the PGAs … voltage PGAs, and the current error you make here, because you have an error current, also, here, which flows into the PGA. And then you can—when you just put some numbers for ZE’s in, and you … when you assume that all ZE’s are the same and all Zp’s are thirty pikofarad, which is pretty realistic for cables, cable lengths shorter that two meters—you end up with a lot of formulas, and you see on the left … a lot of values, and you see—on the left side—you see that, for example, fifty ohm electrode impedance, you have a theoretic overall error which is in magnitude less than zero point zero one percent, in phase less than one degree. When you increase the electrode impedance—as important is that’s at five hundred kilohertz—the important thing is when you now increase the ZE, for example, to two kilo-ohms, then you have an magnitude error of one point seven three percent—sorry—three point three seven percent and zero point one degree—one nine degree—you see, actually, that the phase error becomes smaller, because this … when you look through … or when you go through it, you see there seem to be some kind of an optimal point in between, but only for the phase, not for the magnitude. So it’s kind of a tradeoff. It’ll end up what you want is you want to have low electrode impedances. Then you have the best chance to have accurate values. Another thing which is also important with bioimpedance measurements—it’s not all this theoretic setup—we have, also, problems—for example, when you have a clock jitter on your measurement equipment. So when you think about: you have … you measure here—after this PGA—you measure current signal as a voltage, and here, you measure the voltage signal as a voltage with an ADC. Yes? >>: So I don’t know if you tried shield drivers to better … >> Steffen Kaufmann: We do. >>: You do? >> Steffen Kaufmann: We do. With shield drivers, you can reduce it around a factor of ten—at least the cable capacities. And then you … another problem you have is then the jitter, and the jitter can—with a bit of formulation—you can estimate that a jitter must be smaller than nineteen point four pikoseconds, when you have an ADC with fourteen-bit resolution. And when the jitter is bigger, then the error you make because of the jittering around the sample point—so when here’s a sample point, so ideal sample point, it jitter arounds—and you can make an error in the range of one lsb of the ADC, so you have to be smaller than ninety point four pikoseconds. Another crucial point with that is also the output impedance of the current source, because when the current source … when you go in frequency higher, then the output impedance of the current source drops, and the currents you drive through the objects become smaller, which is—from the measurement accuracy—a smaller problem, because you measure the current, but you need to have a current source which maintain an … a suitable high current, also at high frequencies. And when you … what you see here is the study we make … made in 2012, and a study in 2014, which is … it’s a [indiscernible] ongoing, where we compare different commonly-used current sources. And you see that when you’re starting at one hundred kilohertz, then you see a decrease in the behavior of the current source. We have a pretty flat behavior before, and then it start decreasing, which is some kind of the turning point where bioimpedance measurements become more crucial for the … from the part … from the terms of the current source, and also from the voltage measurement, because all the capacities in the system become—starting then—becoming dominant or more dominant. So we can conclude that bioimpedance spectroscopy is aimed in a frequency range to ten to four hundred kilohertz, as the tissue impedance is much smaller than the ISRE—therefore, you need the four electrode setup. And what I also told you: that there’s a medical standard for … which limits the current—maximum current that you apply to a patient—which is a RMS value of about one hundred forty-one microamp at one kilohertz—which can be increase to up to ten milliamp at one hundred kilohertz—and this basically limits the signal-to-noise ratio you can achieve while you’re doing bioimpedance measurements. With increasing frequency … with increased frequency, the stray capacities become more dominant, and they prevent—basically—the accurate phase measurements, but also the amplitude measurements—or the magnitude measurements. And also jitter is … has an in … but could have an impact; when you think about: you have multichannel bioimpedance measurements, they have to be pretty good synchronized—that you have the same phase—not to make a big error. And to maintain a suitable high accuracy, the current source must also be a … must also have an high output impedance, and the voltmeter must maintain, also, a high common-mode rejection ratio—this one point I didn’t show before, but I can explain it here. When you look at this slide, it’s basically the same. You have here, the current go through the object, and here you have … you need to have an high common-mode rejection ratio, because you have a common-mode voltage at this point, which is given by the shunt resistor in addition to the electrode impedance. And when the electrode impedance increases, then you have a common-mode error. This is basically the idea how to set up … how to measure a complete impedance spectra. So when you look at the top left, you have the DAC; then you have a voltage-to-current converter—which is normally a voltage-controlled current source—then you have the impedance under test you want to measure—in this figure, the I … the electrodes are neglected—and you have the current shunt to measure the current. After the PGAs, you digitize the voltage and the current signal. Then you do an FFT; then you have the spectrum of the voltage, the spectrum of the current, and by a simple division, you get then the impedance spectrum. But to acquire incomplete impedance spectrum, you need to have to sample multiple points—for example, when you’re thinking about a sinusoidal excitation, then you have one frequency, this next frequency, and so on, so forth—but this will take a lot of time. You just take one frequency; then you—you know—configure your system; then you have a transient phenomenon. And another idea is then you can overly … overlay phase-optimized different sinusoidals, but then, you have, also, the problem that the R … maximum RMS current is limited. And the third option would be: you can think about a complex waveform, like a triangle or rectangular, but when you remember your system insist … signals and system class, you will remember that the … we have a decay for higher frequencies. So … and the last thing, which is more or less pretty obvious, is: you can use a chirp excitation, so you have a sinusoidal signal, which increase in frequency over time, and this is—in the easiest case, in the case we are using it—this is a linear chirp. And the linear chirp starts at a pretty low frequency, and over time, increases at frequencies—the equation is shown above. So you can see here that the current frequency is linear increasing over time. And the really nice property of a chirp is that the spectrum is pretty constant in the excitation … in the range of interest, so—yeah—you can tweak a bit the start and stop frequencies, and then you can adjust the stop spectrum in the range you want it. And the chirp we choose here—have chosen here—has the energy concentration between twelve and four hundred kilohertz, and I think it’s like ninety-nine percent of the energy are concentrated in this particular spectrum. Good. So now we have the idea; we had a prism … a measurement circuit, and this is how a possible signal system could look like—this was our first demonstration board. You can see the block diagram here with an FPGA on the left side; you have the … a signal generation with direct digital synthesis; you have—inside—you have an FFT and averaging block, and you have a down sampling block, and you have control logic inside the FPGA. Externally, you have the DAC, which makes from bits analogues … an analogue signal; then you amplify the analogue signal; and then you have the voltage-controlled current source—VCCS—and then you drive current through the electrodes, through the impedance you want to measure. On the other side, the current come in, is measured over the shunt, and then digitized with an ADC, and the voltage here—across the tissue—is measured over the electrodes and a PGA, and is then also digitized with an ADC. The firmware build-up in the first step looked pretty much like that. So you have—inside the FPGA—you have a soft-core microcontroller, which is programmed in C; then you have different interface module … model … modules for the DAC, for the PGA, and for the ADC, which just directly interface with the external components, which is—as I think I said—in VHDL. Then you have a FIFO in memory, and you have an USB transfer to the PC, while on the PC, we add a MATLA … we add a C interface, which handles USB communication, and a MATLAB interface for all display and high-level control. This firmware is then a bit … was then a bit optimized in terms of … we still have the microcontroller, which works as a state machine for all the different modules; we have the DDS and DAC interface; we have the PGA interface, so you can—from the PC—you can send commands to the FPGA; and with these commands, you can set a different gain in the PGAs; you can control the sampling frequencies of the ADC; you can control the actual signal amplitude, and so on, so forth. We have a test data module, which just produce test data to the PC that you can test the communication; we have an FFT module, which directly—yeah—trans … makes an FFT transformation on the hardware; and we have the ADC module, where have also the possibility to send ADC data directly to the PC for debug reasons, and you C-write directly the DAC signal. What is also new here is the AFE block, which is a communication for an analogue front end I’ll show you in a minute, and all the communication is then handled here by a multiplexing and packet-building block, which basically packs all the data in a block for before transmitting it to the PC. This is a first hardware … first PCB of the hardware. You can see, on the right side here, G; you see the voltage interface, so you have BNC connectors, and then you can directly put the cables. Here are the screen drivers—here and here—for the voltage screen, and you can see, then, a bit analogue filterer— filter circuits—the PGAs, and D, as in the DAC … ADC, sorry. And from the ADC, it goes then in A—which is the FPGA—and here’s the current source and the—where you put the current—electrodes; and here is the DAC—and then you have a bit of USB interf … you have a USB interface, obviously; a few LEDs for debugging purposes; and a small power supply for the board. So what we did with this board was we did some measurements on the electrode-skin impedance. For this measurement, we took commercially-available carbon rubber electrodes with a—sorry—with a size of about forty millimeters— say, forty-five millimeters—and we glue this—or we fixated this—on the lower forearm with a distance of two centimeter each, and then we could basically measure the impedance between this point and this point with a four electrode setup. And with a two electrode setup, we can measure, then, two electrode-skin impedances, and the other way around. So when you put current from one to four, and you measure the voltage from two to three, then you can measure the tissue impedance, which is between this two points, right? And when you do a two electrode setup between two and three, you measure the tissue impedance, and you measure two electrode impedances, and when you want to calculate on ISI—so take the average—and then you say, “Total impedance minus the tissue impedance over two,” and then you have the average electrode-skin impedance. Yes? >>: So it looks like those electrodes have two wires coming out of them … >>: But it’s the same. >>: … what are the two wires? >> Steffen Kaufmann: Actually, Gunther, why do we have two wires? I think it’s because of the four … >> Gunther Ardelt: There are four cables. >> Steffen Kaufmann: Yeah, when you have the four electrodes, and when you measure two electr … when you measure the two electrode setup, you need four cables. >>: So they’re the same? >> Steffen Kaufmann: Yeah, they are the same. They’re short-circuit. And with this study, we made a bit … yes? >>: Yeah, I wonder how you calibrated it. You either built a phantom, or is there a commerciallyavailable device that’s the gold standard? >> Steffen Kaufmann: The calibration is basically done on resistors. So you have a … have resistors, and you know they have zero phase, and then you can calibrate the magnitude. >>: But you can build a phantom like you showed in early slide that [indiscernible] >> Steffen Kaufmann: Yeah, the problem with a phantom is you only get capacitors with a tolerance of one percent. When you have really lot of money, you can maybe point one percent, but then you will … you don’t get the values you need. So basically, normally, impedance measurements are calibrated just with resistors—then you know it’s a zero phase—and when you just calibrate the phase, the phase will … is just linear—the phase shift is just time. >>: But there are devices to measure capacitors and then define … >> Steffen Kaufmann: Yes, but then you would calibrate the system with another system, and then you … what … you don’t have any gain from that. So when you calibrate the system with exactly-known resistors, then it’s fine. But we also did studies, and in the papers, there are a few measurement—I think—published, where we calibrate this against an commercially-available system as a … versus phantom. But for the calibration for these measurements, we did it only with resistors. And the ISI: you can see here—from left to right—or the a and b is a study of the—it’s magnitude and phase—of the ISI with dry electrodes; so the electrode were just dry and put on the patient … on the subject, and then we … and the measurements are taken after five, eight, eleven, thirty, and—thirty minutes—and two and a half, and three and a half hours. And what you can see is that, as expected, the ISI drops over time; you have a big—comparatively big—rubber electrode on the skin, and what we assume is they just have some sweat water under it, and therefore, the ISI decreases, because the skin is then moistened. In c, you see the same setup with a pre-moistened electrodes; so they were premoistened with sodium chloride—point … zero point nine percent, so the standard, what you get in a pharmacy—and what you can see is that the ISI change then is pretty small, and you can see, actually, it’s increasing—the ISI—over time, so it’s a dry-up process. And … but what you can see is that the ISI is much, much lower then; then, we have a boundary of about hundred and ten ohm, where before, we had a … up to six hundred ohm. And on the right side, you see the same measurements with pre-gel ectrodes—so that commercially-available pre-gel electrode you put on the skin—and then you see that the impedance of the pre-gelled electrodes is much lower. So this is some kind of the optimal way you can do. Then, we also did a study on what is with the current density, ‘cause what you read in literature is always that electrodes have a current-density-dependent behavior. But what we found out is: with an excitation current of one hundred twenty-five microamp to five milliamps, there’s no visible decay in … differ … like, no visible change in the current-density-dependence, at least with these electrodes. And after that, we did a study on fifteen different subjects, where we measured the electrode-skin impedance with pre-moistened skin after five minutes after application. And what you can see here pretty good is that the ISI is totally variable. So it’s about … almost fifty percent from seventy to one hundred ten ohm around at low frequencies, and at high frequencies, it maintains this broad span, but what we can learn from that is that even for a broad group of subjects—and I think they were ranging from sixteen to thirty-six or something like that … sixty-three, sorry, sixty-three—you can see that you have an average ISI which is below two hundred ohms, and—which is good, when you remember the first … the slides before, then the ISI is highly … the error is highly dependent on the ISI. So what can be learned is that for fast … for good and reliable access, you need a low ISI, and this you can achieve with pre-moistening or pre-gelling of the electrodes, and even with pre-moistened electrodes, the ISI varies very … variance was bigger than fifty percent in our study, and … but it stays always below one hundred twenty ohms. When you—even at lower frequencies—when you think about a classical ECG electrodes, they will always have a better—not always, but when you glue them properly—they will have, also, impedances which are below that. So from a theoretic point of view, we can achieve pretty good measurements—so with zero point one percent in magnitude and below one degree of phase. And the current density obviously does not show an effect, at least in the current range we use for biomedic … bioimpedance measurements. And what we found out here is—what is not shown in the pictures before—is that the tissue impedance you saw had a variance over time, and this variance looked pretty much like this. So it starts at a top point, and it decays, and you have some notch or something like that, and then, it goes up and down. And when you compare this to measurements of the pulse wave of the photoplethysmogram—what you see on a finger—it looked pretty much the same. And when we looked a bit through literature, then we found out this was already published—I think in ’78—and it’s called impedance cardiography, and the basic idea behind it is that you measure the impedance from the neck to the belly, and then you see … get this curve, and then you assume that the blood is increasing and decreasing during the heart cycle. And with a basic formula, then you can estimate—based on this impedance shape and on the values—you can estimate the cardiac output of the heart. And from that point, we decide when we … this is interesting, and maybe we should spend some more work on that, and for that purpose, we thought about adding more electronics to the device, and this is the moment Ankit will take over. >> Ankit Malhotra: The moment I come into the picture? So after this, we already had an impedance meter, and we came up with this idea that maybe this could be used to find the stroke volume or the cardiac output of the heart. So we developed a system by combining the impedance meter with all the known modalities presented now. So it consisted of: ECG module; we had four channels for PPG, because we wanted to see the pulse in different parts of the body, because they vary with the morphology—so you have a different PPG on a small artery and you have a different PPG on a bigger artery—so we had four modules for PPG; and then, we—at that time—we had another concept of getting the signals from inside the ear, which is the auditory canal, so we tried to use a normal headphones to get the pressure signal inside the ears, which also vary because of the blood being circulated near the arteries or the part … or the ordery canal of the ear; and we left one for general purpose, so we could add something else in the later on if we find something important. All these parts were connected to the ADS 1298, which was from Texas Instrument; it was an eight-bit … eight … it had eight ADCs inside it, so we could convert all the signals at the same time, so the … all the signals were at … had the same time reference. And everything was connected to the cardiometry module, which is just the impedance meter only, and the whole hardware was controlled by the FPG, and the data was transmitted to the PC and was further analyzed in the MATLAB. So this is what … how the new hardware looked like; it was a PCB which was around, in dimensions, one thirty-five mm into one forty-five mm and had more than seven hundred components. And as you can see, the assembly of the PCB: the green part is the analogue part, which contained all the ECG, PPG circuits, and the blue was the digital part, which was originally from the impedance meter which Steffen just showed, and then we had a power supply for different parts of the PCB, and all the connectors are shown in the red. So on the right inside, the four BNC connectors are for the impedance measurement and three new BNC connectors for ECG. So this is how the setup looked like for the research: we had these; we had a subject—which was a healthy subject—and we connected him like this. So we had two blue electrodes, which were the current electrodes; and two red electrodes for voltage electrode for thorax impedance; and then we had two ECG electrodes; and we put PPG on the index fingers as well as near the ear, where the headphones were placed so that we can have a reference that the signal being shown in the headphone is how much similar to the signal being acquire by PPG. So this is how all the signals looked like when we acquired. On the first, you have a … we just gave a rectangular pulse so we can see the time—how the time is happening—and then we have different signals coming out. So the first signal is the impedance signal, which Steffen showed in a bigger way, but it’s here; it’s just a bit small, and the next two signals are the PPG signals which were acquired from the fingers. Then, we had this headphone signals, and then again, two PPG signals, and in the last phase, you can see the ECG signal. So all these signals are time-referenced; all are simultaneously taken and could be further used for analysis. And this is … was how the—originally—the signal looked like for impedance measurement, and we excited the patient with a chirp signal instead of a single frequency, but here, we just show for the frequency of the chirp was varying from twelve to three hundred fifty kilohertz, and—five hundred twelve kilohertz, okay—and so the … as you can see, there’s a change in the impedance also. So we can find the pulse present in the phase of the impedance signal, and this was very interesting, and I think it was never reported before. But still, we are looking forward, like how the frequency and the change in the frequency plays role in the change in the impedance. >>: This is actually a little different, right? This is—instead of the impedance across a thorax—it’s just a forearm. >> Ankit Malhotra: Yeah, this is not impede—yeah—this is on the forearm—sorry—this is—or was—on the forearm, not across the thorax, but probably, we’ll get the same kind of effect over the thorax also. >>: But it’s really interesting you can see … >> Ankit Malhotra: You can see a change in the phase. The system is like … it has a very good resolution. And after collecting all this data, the main point was to use these existing modalities to find something new, which could not be found by normal ECG and PPG—or the information they lack. So we did some—really—mathematics or MATLAB in it, and first thing we calculated was to try to estimate the stroke volume and cardiac output—and I will tell you about the results. Then, next thing we did was heart rate variability, which is very important barometer in sports and everything, but normally, ECG is only used for heart rate variability. So we tried to compare heart rate variability with impedance as well as the PPG signal, because all were taken at the same time. Third thing we do was called PAT and PWV—this is another new thing which is called pulse arrival time and pulse wave velocity—right now, there’s a lot of research going on in this field, and it’s a prognostic marker for cardiac disorders if someone has an idea. And then, we also calculated the number of respirations from the … from some of the modalities we already took. So this is how the flow of the software was … flow of the implementation of software was. So we imported the signal from the BMS system; then, we de-noised it and removed the baseline wandering; and then, we did some signal processing, and we calculated peaks and valleys on different physiological signals. These peaks were stored, and then, all other parameters were calculated by using different signals for different modalities, and then we displayed it and stored it for further use. So for de-noising and baseline removing, I used Wavelet, and one of the use of the Wavelet was to calculate the respiration rate also, because the sick … the electrodes which were near the heart or something always had this baseline wandering because of the movement of the chest—expansion. So in Wavelet, you can easily remove this into different signals, and like you can see on the right-hand side, the first figure shows a PPG signal which is being … which has a lot of baseline wandering, and you can just remove the baseline wandering and you can use the removed signal, just to find out—the peaks will give you the respiration … amount of respiration happening in the body. And these are the—some of the—results that we got from all the three subjects, which we tested with all the measurements we had. And I would just like to point out on stroke volume and cardiac output— which was the main aim in doing this research—but the results are not that good. So they are a bit out of the range. This could be … the one reason behind this could be because the physical model behind … for calculating the cardiac output and the stroke volume from impedance meter—or the impedance measurement—lacks certain things. So it has so many constants, like hemotocritic value, height, and weight, which play a … which also play a very important role in the calculation. So this was one of the reasons, like, for, like, subject three, the output was … cardiac output was like ten point two liters—this is not possible; this is something wrong over here. And we calculated PAT values and PW values, which were all in the range for a healthy subject—there was no problem in it, even the number of respirations. And heart rate variability by differing modalities—like, for ECG and PPG are just shown—and they are quite similar, so there’s no difference if you use ECG, or PPG, or impedance, you will get the same result for heart rate variability. Yep? >>: [indiscernible] you’re using is, say, the gold standard to compare this to … is that you know now it’s out of bounds? >> Ankit Malhotra: The gold standard we used was the standard, like for … we know the standard values—like, there are so many paper being published which has these PAT values and PW value … PWV values, according to differing subjects of different health or something … >>: That isn’t an instrument. >> Ankit Malhotra: No, we didn’t compare it with some instrument; we just compared the physiological values given in different journals or something. >> Steffen Kaufmann: To give Texas point, this is … was a proof of concept—that we measure the impedance, and we take a published formula for estimating the cardiac output, and it’s black magic, huh? So there’s so many parameters in it, you could tweak pretty much everything, and—at least from these basic parameters—and we don’t have an invasive gold standard method to test this against. >> Ankit Malhotra: Because for a [indiscernible] >> Steffen Kaufmann: It’s just a proof of concept. >> Ankit Malhotra: … for stroke volume and cardiac output, there are three gold standards: one is thermal dilution method; other one is ultrasound; and one is Fickle method—all three are invasive. You have to get the subject into a CAT lab and monitor it, so it cannot be done real-time. So this is … that’s why it is one of the most important research also. >>: Well, that would be a goal—right—for … >> Ankit Malhotra: This could be a gold also, in the future. >>: Yeah. >> Ankit Malhotra: And so then, we came up with the idea or the—it’s not an idea; so we just wanted to improve our system—so we came up with the new Bioimpedance Measurement System, in which we just had new hardware development and enhanced some parts out of it. So now, we have two different PCBs: one containing the impedance meter, which contains the FPG, and the other is the daughterboard, which contains all the analogue circuits—like, it has headphone jacks as well as heart sound jacks, now we introduce into it. So before, we just had two headphones in the ear; now, we had an … we have a … to measure the heart sound, also, on the chest, and we had three ECG electrodes and—I think—three PPG circuits now, instead of four. And this have a better current source; Steffen didn’t spend too much time on the current source, but now, it has AD8130-improved current source, and yeah. So it was just made much more easier and looking much more cool. Okay, so this was how the BMS looked like, and from now on, Steffen will again take it. >> Steffen Kaufmann: Yes, hello. A bit to make the point is … what I have the feeling which was not really transported during the presentation is: we made an awesome accurately measuring device. So we … Ankit showed on the slides: we can measure phases of zero point zero one degree—at least … not absolute, but relative phase changes. So what we could show is that we can measure on the lower forearm … in this setup, we showed … we measured an impedance variation which was plus/minus fifty milliohm, and we can have a phase resolution which is zero point zero one degree—we could see the difference. And we can measure this in a frequency range between twelve and, basically, we can measure up to five hundred twelve kilohertz with the chirp which is, at the moment, implemented, whereby, at higher frequencies, the signal energy goes so down that the signals don’t look that good, so we only show to three hundred and ninety kilohertz, but to that, we could measure pretty accurately. And you can see here the newest generation of the impedance measurement device, which is—before, we always named it Impedance Meter, and this is really the Bioimpedance Measurement System— which is here. What you may remember—recall from the slide which in black and white, where it shows this—it looks pretty much the same; the difference is: it has a much bigger FPGA; a much higher, improved firmware; the current source is increased—improved—and … or the accuracy is improved. And then, we have here the two future interface ports, and with these interface ports, you can connect different analogue front ends. So at the moment, what I can say is we had this analogue front end, but it’s possible to simply connect everything to that. It’s an SPI interface which is implemented, and it’s an FPGA, so you can think about arbitrary interfaces you can implement, and connect to the impedance measurement, and synchronize. And this is a crucial point: we can measure the impedance, and we can synchronize this with PPG; we can synchronize this with ECG and with this headphone signals, which I will introduce in a minute. And what we also did is we had, also, a pressure sensor, which we had connected before; then you can measure blood pressure, for example, also with this system. So what we did is we made this device, and we verified it against—oh, I can give you a paper reference where we explain the calibration in detail. The system is accurate in the range of twelve to five hundred ten kilo … allo works in the range of twelve to five hundred ten kilohertz with the given chirp. It’s possible to go, also, down with the frequency to—let’s say—one kilohertz, and you can also go up to, maybe, six or seven hundred kilohertz, but then you have the problem that the stray capacities become dominant and also the common-mode rejection ratio is not that high enough to compensate the error. The possible excitation currents ranging from about ten microamp to five milliamp, whereby the high accuracy is only possible at five milliamp, and the overall uncertainty’s staying below one percent for the impedance magnitude and below point one percent … point on degree for the phase in most measurement ranges with an effective resolution down to seventy … twenty-three milliohm. This is raw data, so when you think about: I told you that we have about four—I hope I told you—that we have about four thousand impedance spectra that we can acquire per second. You can think about: when you have some low-frequency phenomenon, like heartbeat, you can do a lot of averaging, and then you can improve the effective resolution by factor of ten, factor of fifteen—depend on how long you average—and the same is true for the phase. Additionally, we have the possibility to measure—at least in the current setup—one ECG; three PPG signal—which is photoplethysmography—and we have two pressure signals we can acquire; and we have two microphone channels; and the analogue … and this analogue signals, we are interfaced with this analogue front end, and we can sample, then, up to four kilohertz; and also here, we can, then, oversample, whereby the analogue front end has twenty-four bit resolution. So you can—pretty good—measure, and—yes—and we did, already, a few interesting and promising measurements; we also have made some heart sound measurements—so not only impedance, you can also combine it via the microsound jacks, for example, for measuring heart sounds and put this in time reference with impedance signal. One thing we did—which was basically my PhD thesis—is electrical impedance tomography. You can think of an electrical impedance tomography as a multichannel bioimpedance measurement. And the basic idea of that is that you measure currents and voltages, and you can calculate from that transfer impedances, and based on that, you can estimate the impedance distribution or the conductivity in distribution inside an object. The idea is from Henderson and Webster, and you could solve first images in 1984 in this paper. And as bioimpedance measurements are, it’s noninvasive, painless, and it’s a fast, functional imaging modality. So it’s … you have almost re … or you have real-time, so you can have up to thirty frames per second—so even more. The drawbacks are: it has a poor stability; it has a low resolution and large computational effort. And what you … what is available is a machines for showing the ventilation of the lungs, so you can see the … how the lung is ventilated, and which part of the lung have air inside, and which are not. And the basic idea of this reconstruction is if you have a current injection in the offs … in the object, and you have the so-called forward and inverse problem. The forward problem is: you know the impedance as a conductivity distribution; you know the current injection; and then, you can calculate the boundary voltages around the body, for example, when you have it around the chest. The inverse problem is what we have; we have the boundary voltages; we have the current injection; and then, we want to calculate from this the electrical conductivity distribution. So … and when you look on this equivalent circuit … or on this schematic block diagram, you see on the left side, you have a current source and a lot of voltage measurements around the object—for example, the thorax—and the most easy measurement principal is: you have just one current source; you have one voltmeter; and you have a multiplexer, which multiplex then a lot of cables. And based on these measurements, you can then reconstruct images. I will just skip the mathematical formulations because of time reasons and show you how we … how it looks in practical setup. You … for the practical setup, you need a forward model—so you need a model how your patient or how the object you investigate look like. For example, for a thorax you could do … use an CT scan from the thorax to generate this forward module—you have here the thorax; you have here the two lungs—and then you can somehow bait … build a basic forward model. What we did is we have made a tank study in the first place, and you can see here the tank; you had the electrodes around; the tank was filled with salt water; and then we did two measurements. We do an empty measurement on the left side—so an empty tank, just with … filled with salt water—then, we put two phantoms in, and what you can see—after the acquisition of the different measurement data and after the fancy medical image reconstruction—you can see if you … an increase in impedance—so a decrease in conductivity—here and here. Looked bit like this on the test build-up; we have here the EIT system, which is in fact like … something like impedance meter and multiplexer. Then we have here a cable adaptor with a lot of shield drivers, and then we have here the electrode tank or the water … the tank with a saline solution. And—yeah— the tank with a [indiscernible] with the two phantoms, and here’s a close-up of the system with cables. We also did this in a small scale with small tank phantom, which is—from electrical point of view, electrical injuring point of view—pretty nice, because this just VIAs here in the PCB, which are drilled as a wire—drilled wires—and then it’s milled around, so you used, basically, a wire in the PCB as electrodes. And one thing I want … also want to show you: this is an … a measurement we took from a healthy human chap … subject, and you see his breathing cycle. So we took an measurement from the patient … from the subject, and the patient breathe in breathe out, and what you can see here is that he starts breathing out, and then you see an increase in conductivity … a decrease in conductivity—sorry— and when he—breathe out, breathe in—and then he breathe in, and then you see it’s the opposite. And then you can see here—partly—you can see a bit of two lungs, but mainly it’s an artifact. But already, you can see there’s something visible in breathe out and breathe in. And then it looks—when you take the overall impedance, so you sum up all impedances—then you have something like this; so you breathe out, breathe in, breathe out. It’s exactly what you see here. Breathe out, breathe in. Okay, so let me now switch the topic to in-ear pulse wave velocity measurements—this is another thing we did. The basic idea is: pulse wave velocity is based on the artery system; when you think about … you have the heart; the heart is contracting and doing the contraction; there is blood flow coming out from the heart; it’s going to the aorta, and from the aorta to the different parts of the body. And you may know that the aorta is elastic, so the heart pumps; the aorta opens and takes a blood volume; and then, the aorta goes at a … closes; and then, the blood is pumped out from the aorta. So aorta helps the heart to pump the blood through the body so that you somehow have a constant blood flow over the heart cycle. And the elasticity of the aorta is a important prognostic marker for the age of the vessels, and there’s a so-called Moens-Korteweg equation, which says that the pulse wave velocity is given somehow by the elasticity module, and the arterial wall thickness, the vessel radius, and the blood density. So what you can do, then, is you can estimate the elasticity of the artery … of the aorta; you can measure by a time difference—by a pulse wave velocity. So you measure, for example, the heart starts pumping blood out, and then you measure—for example, in the ear—how long does it take until the blood reach the ear? Then, you can measure the distance; you can measure the time; then, you can calculate how stiff the arteries are. And … yes? >>: So how do you measure this? See, you don’t have access to those vessels. >> Steffen Kaufmann: No. That’s kind of the problem. When I start as an electrical engineer, I thought, “Oh, come, everything is same; you just taken a linear, and then you measure everything from the outside,” but we have a physicist in the—not a … a physician—in our team, and he said, “No, it’s not that easy, because every artery looks a bit different.” But the good point is that when you from … look from here to re … the most dominant part is the aorta, and this is thick, and this goes straight—almost straight. So you make an error, but the error’s pretty small—as a … not pretty small, but it’s small enough to have … stay reasonable values. So … and what we want to do is we want to have exact measurements; we want to have comfortable measurements; and we want for continuous measurements. The gold standard is: you put a cuff around the arm; and then, you basically measure the pulse wave velocity on the morphology of the waveform, because you have an outcoming wave as a pulse wave; and then you have a reflecting wave, where it’s reflected; and then, with a bit of maths, you can calculate the difference out of that; and then, you can calculate from that—with a known model of the arterial system … or with an assumed model of the arterial system—you can calculate the pulse wave velocity. And what we think is we are much more accurate, because we don’t measure somewhere here with a reflection and back and forth; what we measure is the … from here to here—so in the ear—and here, where the aorta is. So we have a pretty straight connection, with pretty close connection, and the good thing is we don’t have a cuff—and the cuff has pressure, and you have … release the pressure, increase the pressure; you cannot do this often, because then, you’re just … you press out water from the tissue. So you know this, maybe, from blood pressure measurements at home: when you do it ten times, the arm hurts, and the measurement change. This we … this problem we don’t have. So our idea is we measure this in the ear, and how does it work to measure the pressure in the ear? When you think, you have here the inner ear; you have here the eardrum; and here, the auditory canal; and here, the outer ear. We have a pressure sensor, which pretty much look like an headphone—in fact, we can use a headphone; this is why we have these two headphone channels—and we put the headphone channel in the ear … or the headphone … this sensory in the ear, and then we have a closed cavity here, which is in your canal, and this pressure inside here is pulsating. You may know this effect: when you put your head under the water when you … on the bath tap, you hear your own pulse; when you lay on the pillow, sometimes you hear your own pulse in the ear, and this was the basic idea—when you can hear it, an earphone can also hear it. And so you put the pressure sensor—which is in fact an headphone—in the ear, and then you can exactly measure the pressure change. So what does it mean we have an … when you have a change here—pressure change—where can the pressure change come from? The pressure change must come from some artery, and it must come from the pulsating of the artery, so in fact, it’s blood coming in from the heart. So what we have, then, as the heart pumps, the blood flows, and then we can measure here the incoming blood. So we have exactly the diff … the distance as a … it’s a time reference. And then we have a system which looks like this for the measurement setup. We had a pressure sensor in the ear; we have the headphones—well, not at the same time; after each other, it does not fit both— for reference, but we have the headphone, therefore the pressure sensor; we had a PPG sensor behind the ear and a PPG sensor inside the ear, that we can so measure … that we were able to measure … take some measurements to somehow data mine which artery is providing the signal—that you can data mine how big the artery is and how long the distance is. And for that, we built this ear mold, which is a custom ear mold for—yeah—which is personal ear mold, so have … it’s lot of work to have this ear mold—this is mainly Gunther’s work—and you can see we were able … Gunther were able to fit a PPG sensor inside. There’s a photo detector and an LED here; and then there’s a tube coming out; and then we have a commercial-available pressure sensor, which can measure in millibar; and then you have here the electrical connection. And the—well—the SPI interface, its electrical connection is: who can guess it—to what it was connected? To our impedance meter—so the BMS—and also the headphone signal, of course, also connect, and then we could compare some measurements. Specially for that setup, we also made another device, which is then called iGunther—so Gunther made all the work, so we made the iGunther—and it’s has an ECG, the pressure sensor, a PPG inside, a temperature sensor—which was also included in front; smallest thing, you cannot see it, but these are the two wires for it—to get … you can measure the core temperature in the ear—or almost the core temperature of the body. And we also had an acceleration sensor, so you can basically see if the subject is standing, is falling, is moving— so basic measurement system. Looked like this, and—yeah—we have a … we made a small box for it with a battery, and then you can wear it. It also Bluetooth connection. We also made a software for it—then you can see the measurement in real-time—and you can export it, also, to MATLAB, and then you can also configure the system via the GUI here. And these are the—basically—the signals you get, which is pretty interesting. You have here an ECG, which looks like an ECG in … from emergency room—yeah, from the TV show—then you have the pressure on … in … on the left ear, and then you have a PPG on the left and the right ear, and then you see here—oh, no, sorry—this is pre … PPG left, right and this is pressure. And what you can is that signals are almost the same, right? So the pressure and the PPG—and PPG measures a volume—have the same morpholog … simple, comparable morphology, but they have the same starting point, so therefore, we can be sure that the pressure signal we measure is heartbeat-related and is based on the artery volume. And then we had … the next step in from iGunther, we come to EarGunther, and this is really credit card size—or smaller than credit card. Here, this is the nine-volt block battery—I’m not sure if it’s also available here in the States? Okay. So it’s pretty small and can simply mount it behind the ear—at least, our idea—then you can measure over long period of time, and it’s pretty much the same as iGunther—the same functionality—but smaller. And here are, then, some measurements we’re going to present on a … in one week? Roman is going to present it in a German medical conference. And we have here the ECG, and you have then here the pressure curve, measured with the headphone—with a slightly modified headphone—and you have here the PPG—that’s A. Temporalis Superficialis; this is in here, right? >>: Yeah, it’s in … >> Steffen Kaufmann: Yeah, it’s rolling around in front of the ear. And what you can see is it’s—except for the dicrotic notch, which is missing here—this is exactly the same signal, and based on this, you can then measure the pulse arrival time as the time between the ECG peak and then the arrival of the wave in the ear. And with easy maths, you can then calculate from the distance and this abstraction of the pulse arrival time from the pre-ejection interval … or period—so the time from the ECGR peak until the heart starts pumping. You can then calculate the pulse wave velocity, and a few measurements we did, having six point four meters per second for pulse wave velocity, and this is—oh, for males below thirty or around thirty—it’s totally fine and totally in the range. We also compare it with a few measurements of older people, which increase, then, in pulse wave velocity, which indicates that it’s pretty much goodworking, but to catch the next question about the gold standard verification, we didn’t do this so far, but in this case, we’re planning to do this soon. So we’re able to detect the pulse wave in the ear, and we have a time-continuous measurement there that’s comfortably wearable. It’s cheap; basically, it’s a headphone which is slightly modified. Then, we have as what we are not sure is about where the signal genesis is really from. Before, we thought it’s maybe the tympanic membrane moves a bit; then in between, it was: it’s the auditory canal is pulsating, but the auditory canal is a bony and cartilage structure, so it’s unlikely that it’s pulsating; and I think the current idea is that it’s really the outer part—is where the Superficialis is—that it’s just pulsating, so here’s a devagos, and all this is just pulsating, because this pulsation that even the pressure sensor’s a bit moved, but this is not mud-clear so far. And the good thing is we are thinking about enhanced methods which can … which we can correct for the pre-injection interval, which is here fixed to seventy milliseconds—so we just assumed—and we have one method in the pipeline which allows us to measure this directly. In an outlook, which we also think about is: so far, we just have sensors to the body—so we just measure what the body is producing—maybe we can enhance this with a few actuators. For example, when you think about a calf—for example—so one thing is what we … we have a research project is to knock on arteries. So you have a calf, and then you knock on the calf, and then you produce a pressure change, and then you can measure the pressure change, and what you can do is: you can do system identification. You know, they have an artery which is unknown from its behavior, so then you make a pulse—an external pulse—and then you can measure the reaction; you can do the system identification of this artery. Yes, this was basically my talk; thank you for your kind introduc … attention, and I’m totally open for questions. [applause] >> Gabe Cohn: So we can take question from the audience. So while we all think, I’ll ask a question. So it looks like you built a lot of really interesting hardware that you can now do some exciting, new medical research with. >> Steffen Kaufman: Yes. >> Gabe Cohn: So—you know—where is your interest? Is it just in the hardware? Is it also in the medical science? >> Steffen Kaufmann: Basically, I’m electrical engineer, so I’m interested in hardware. [laughter] So my part was: I built this hardware; I verified the hardware in terms of the electrical signals; and this is where my interface is. And Ankit was biomedical engineer, so he starts from analytic … electronics, and do all the verification, hence and tests, “No, this is the wrong artery; it does not”—say—“make sense. No, a vein cannot produce a pulse,” you know? [laughter] And this is always the stuff that comes from Ankit, and so far, we also have this medical clinic in Lübeck, which we can cooperate with to do some clinical trials, but in fact, we’re losing manpower—we’re lacking manpower—so we are a few people only, and this is … >> Ankit Malhotra: [indiscernible] time comes when in [indiscernible] >> Steffen Kaufmann: … or we can continue. >> Ankit Malhotra: [indiscernible] ethics. >> Steffen Kaufmann: This is one thing. >> Gabe Cohn: Do you collaborate a lot with medical partners? >> Steffen Kaufmann: We’re … in fact, we have a medical partner in our group, which is also active in the German asso … um, what is it? >> Ankit Malhotra: [indiscernible] >> Steffen Kaufmann: Aterial stiffness? German Society for Arterial Stiffness … whatever, and DeGAG is the other version. And yes, so … but this is a collaboration in terms of: we have advice from him; we have an exchange of thoughts, but no more so far. So we have to begin at the beginning; we have the measurement system, and now, we have to go to verify it, or to … this with the gold standard. >> Gabe Cohn: Questions here? >> Steffen Kaufmann: Yes? >>: Very cool. >> Steffen Kaufmann: Which part? [laughter] >>: The noninvasive pulse wave analysis that you’re able to do. It’s very invasive by putting a pressure sensor inside a vein or an artery. >> Steffen Kaufmann: Yeah, this is the gold standard, in fact, yes. >>: Well, the Eastern medicine—namely Chinese—have known this for many, many, many years. Western medicine just hasn’t caught on, so … >> Steffen Kaufmann: In fact, we have a cooperation with a Chinese university, and then we all say, “Yes, we’re doing pulse wave analysis,” and then the Chinese professor respond, “Yeah, we do this for two thousand years, about.” [laughter] >>: But it’s subjective, though, so you got to get those grey-haired palpation … >> Steffen Kaufmann: Yep, exactly, and then they put the fingers on, and then I think that they decide three or four different pulse waves—feelings. Matter of fact, the morphology changed a lot over the age and over the stiffness; you don’t have sense of dicrotic notch anymore, then just … this is just a big wave or a big pulse. >> Gabe Cohn: Any more questions? Alright, let’s thank our speaker again. [applause]