Biology 242 – Lab LAB #2 2
advertisement

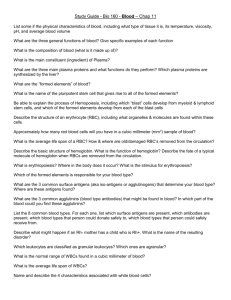
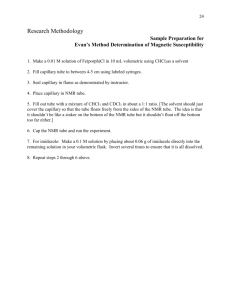
Biology 242 – Lab LAB #2 (2nd/19 Lab Sessions for Winter Quarter, 2008) TOPICS TO BE COVERED: »Blood Cytology: Terminology for Hematology »Perform a Hematocrit test on a sample of dog’s blood »Blood Smear and Wright’s Stain Technique »Microscopic exam of the formed elements of blood »ABO and Rh blood groups (including genetic considerations) DESIRED OUTCOMES: After completing the activities described for this lab session, students should: »Be able to recognize / use proper terminology / notation when filling out a Hematology Lab Slip »Understand the process of preparing a blood specimen for microscopic exam »Be able to identify all the formed elements of the blood »Be able to explain what is a CBC, Differential White Count, (“Diff count”), and an Hematocrit »Explain the ABO and Rh blood groups and the genetics of blood types. MATERIALS NEEDED: »Dog’s blood in 3ml vials (at least 6 vials – one per lab bench) »Microscope Slides »Small Pipettes »Paper Towel “placemats” »Diff Quick Staining Trays with Procedure Prompt Cards »Distilled water Wash Bottles »Heparinized Microhematocrit Capillary Tubes » Microhematocrit Centrifuge »Wet paper towel per bench »Critoseal »CritoCards (Hematocrite Reader cards) »Tray of Hematology Kodachrome slides »Wall Charts of the Formed Elements of Blood and of the ABO Blood Groups Activity #1: Blood Cytology: Terminology for Hematology Blood is a fluid connective tissue that flows through the vessels of the cardiovascular system. Blood is composed of cells and cell fragments that are collectively called the formed elements; these formed elements are carried in an extracellular fluid called blood plasma. Blood has many diverse functions and capabilities, all relating to supplying your cells with essential materials and maintaining the internal environment. A very special quality of blood is that, in response to injury, it has the intrinsic ability to change from a liquid to a gel so as to clot and stop bleeding (hemostasis). The blood controls the chemical composition of all interstitial fluid by regulating pH and electrolyte levels. Red blood cells (erythrocytes)transport respiratory gases to trillions of cells in your body. White blood cells (leucocytes) are part of the immune system and protect you from microbes by phagocytosing foreign cells and producing antibody molecules. Platelets (thrombocytes) assist in platelet plug formation and coagulation. Using one of our own “Pierce College” Hematology Lab Slips as our “guide”, you will be learning various terms specific to each of the formed elements of blood to describe their quantitative and qualitative features. On the next two pages is a brief list of some of those terms: Biology 251 – Lab LAB #2 Page Two TERMINOLOGY FOR BLOOD WORK I. RBC CONSIDERATIONS A. Morphology 1. SIZE (Anisocytosis: “variation in size” (Gr. anisos = unequal) ) a. Normal size: 6 – 8 µ b. Microcytic: 0 – 5 µ c. Macrocytic: 10 - 20µ Too much anisocytosis indicates pathology. 2. SHAPE (Poikilocytosis: “variation in shape” (Gr. poiki = varied) ) a. Burr cells (RBC membrane has “kinks” in it) b. Tear drops c. Helmet d. Ovalocytes e. Elliptocytes (1) One stage to Sickle Cell shape (2) Sickle Cells f. Spherocytes (No room for expansion; very little tolerance for different blood tonicity.) (Spherocytosis is an inherited tendency.) B. Coloration 1. Polychromasia: when RBC’s look bluish; indicative of young, immature cells. 2. Hypochromasia: characterized by a big, pale area in the center of RBC; indicative of too little hemoglobin. Of clinical note, is that microcytic hypochromasia is the classic iron-deficiency anemia picture.) 3. Basophilic stippling: very abnormal; related to polychromasia seen with lead-poisoning. 4. Howell-Jolly Bodies: small, round or oval structures (pink or blue in color) observed in RBC’s of various anemias and leukemia. These probably represent little remnants of the nucleus (from reticulocytes) which become inclusions in the circulating erythrocytes. C. Other 1. Nucleated RBC’s: 1 nucleated RBC/100 RBC’s (that is, 1%) is very abnormal. Such a finding is indicative of metarubricytes (aka: the blast-form of erythrocytes) being released prematurely from the myeloid into circulation. 2. Reticulocytes: immature red blood cells. “Retic. Counts” are done to evaluate the erythropoietic rate and to monitor anemia treatments. 3. RBCs enter the circulation at the astonishing rate of 2 million per second (a pace that Just balances the equally high rate of RBC destruction. (Remember: RBCs live approximately 120 days once in circulation) II. WBC CONSIDERATIONS A. Criteria for telling one WBC from another – there are 4 major criteria used to differentiate one WBC type from another. Here is a brief elaboration of each of these 4 criteria: 1. Overall perimeter (size) of the cell: Platelets smallest; RBCs next smallest; Lymphocytes (well-contracted vs. “floppy” – may vary from barely larger than an RBC to twice as large); Basophils, Neutrophils, Eosinophils are all about the same size as each other and all are nearly twice as large as an RBC (Basophils are generally slightly smaller than Neuts or Eos.); and Monocytes are the largest of all WBCs – easily three-four times the size of an RBC. 2. Nuclear morphology (that is, “shape” of the nucleus) a. Large, generally round, dark bluish-purple nucleus = Lymphocyte 2. b. Largest, “dinged”, pinky-purple nucleus = Monocyte (Blood Work Terminology, Page Two) c. Dark nucleus is quite visible, NOT round, but of uniform width or “lobed”: (1) Uniform width and shaped like a “c”, “n”, “s”, “u” = Banded Neutrophil (aka “Bands”) (2) The older the Neutrophil gets (that is, the longer it is in circulation), the more “segmented” the nucleus becomes. The once uniform nuclear material starts to attenuate (pull apart) and to form lobes; but always a thin strand of nuclear material attaches one lobe to another. There may be as many as 7 – 8 lobes. Even with only 2 lobes, as soon as distinct lobes are visible, the cells are now called Segmented Neutrophils (aka “Segs”). d. Dark nucleus is not distinctly visible; because it is “masked” by the cytoplasmic granules: (1) Nucleus completely covered by large, dark-blue granules = Basophil (2) Segmented nucleus is not totally obscured by large, orangy-red granules – Eosinophil. Note: the visible nucleus is OFTEN (not always) segmented in such a way as to have two large lobes with a much smaller third lobe in between them: This is referred to as a “spectacles nucleus” for its obvious similarity to a pair of eye-glasses. 3. Presence (or absence) of Cytoplasmic Granules a. When granules ARE present in the cytoplasm (all the way out to the perimeter of the cell) then the cell is one of three Granulocytic WBCs (aka: a granulocyte): Neutrophil, Eosinophil, or Basophil. (*Now, see 3c below to further differentiate these from one another) b. When NO granules are present in the cytoplasm, then the cell is one of two Agranulocytic WBCs (aka: an agranulocyte): Lymphocyte or Monocyte c. If granules are present, then it is the color of the granules that further differentiates the granulocytes one from the other: Dark blue/purple granules = Basophil; Orangy-red granules = Eosinophil; or “Freckle-like” (barely visible granules) = Neutrophil 4. Color of cytoplasm, nucleus, granules (if any) One must take into account the overall color and texture of the major components of each formed element - although color is the least reliable of the criteria because, over time, the coloration fades/changes; or the Wright’s stain may be mixed a little different one time than another. Special Note: All WBC granulocytes (that is, Neutrophils, Eosinophils, and Basophils) may be referred to as PMNs (polymorphonucleocytes) because they are nucleated cells, each of whose nucleus assumes many different morphologies (shapes). As the cell ages, the nucleus becomes more and more lobed (aka “segmented”). B. WBC “Diff-Count” Terminology 1. Two suffixes denote increased numbers of: a. –philia (used for blood cells whose name ends in –phil ie. the granulocytes: neutro-, eosino-, + basophils) b. –cytosis (used for blood cells whose name ends in –cyte ie. The agranulocytes: lympho-, + monocytes; as well as for erythrocytes and thrombocytes.) 2. One suffix denotes decreased numbers of: a. – penia (used for ALL blood cells; for those ending in –cyte: either by first dropping the –cyte ending and adding –penia or by adding –penia after the ‘cyte’ syllable; and For those ending in –philia: by replacing ‘philia’ with -penia.) 3. Therefore: neutrophilia = increased numbers of neutrophils neutropenia = decreased numbers of neutrophils eosinophilia / basophilia =________________; eosinopenia / basopenia = ______________ but lymphocytosis = increased numbers of lymphocytes lymphopenia or lymphocytopenia = decreased numbers of lymphocytes monocytosis = ________________________; monocytopenia = ______________________ What is leukocytosis?________________________; What is leukocytopenia?_____________________ See Table 19.3 (P. 680 of Text): Summary of Formed Elements in Blood for the normal quantitative information about each of the blood cells; including normal differential white count (the “diff count”). Biology 251 – Lab LAB #2 Page Four Activity #2: Perform a Hematocrit test on a sample of dog’s blood The hematocrit (Hct or “crit” test), or packed cell volume (PCV), measures the volume of packed formed elements (cells and platelets in the blood) per volume of whole blood; it is always expressed as a percent. Since RBC’s far outnumber all the other formed elements, the test mainly measures the volume of red blood cells. To perform the test, a drop of blood is collected in a heparininzed capillary tube. Heparin is an anticoagulant and prevents blood from clotting inside the capillary tube so that the RBC’s can be separated from the plasma. A microcentrifuge is used to spin the blood sample at a very high speed for approximately four minutes. The gravitational forces produced by the rotation of the centrifuge pack the cells into one end of the capillary tube, therefore the term packed cell volume. On completion of centrifugation, the sample is placed on a tube reader, and the percentage of packed blood cells is measured – the result being read directly off the Critocard. Hematocrit results provide important information regarding the oxygen-carrying capacity of the blood. A low hematocrit value indicates that the blood has fewer RBC’s to transport ozygen. Normal hematocrit values for males range from 40% to 54%, with 47% being an average; for women the range is lower, from 37% to 47%, with 42% being an average. PROCEDURES: 1. Blood was drawn from one or more of the very health dogs in the Veterinary Technology Program downstairs. This is the blood in the 5 ml vacutainer provided at your Lab Bench in the small beaker. From this vial, each student will need to prepare a capillary tube by filling the tube at least two-thirds full with blood. But first, each student should have a paper-towel placemat at his/her desk AND a wet-but-wrung-out paper towel ready. (This moistened towel will be used to clean off the outside of your capillary tube once prepared as follows:) 2. One student at a time, takes a sterile heparinized capillary tube and inserts it into the vacutainer of blood and allows the blood to “wick-up” the tube by capillary action; it must fill at least two thirds of the way up OR MORE. 3. Now, carefully seal one end of the tube with the critoseal clay, being sure NOT TO FORCE THE DELICATE CAPILLARY TUBE BY PRESSING DOWN ON ITS TOP END, for it may break and cause you to jam glass into your finger or hand. 4. Next, seal the other end of the capillary tube by inverting the critoseal tray and pressing it onto the upper end of your capillary tube. 5. Clean any blood (it will probably be dried on by now) off the outside of your capillary tube with the moistened towel at your desk. (This will make the tube easier to read accurately when ready; and will also keep our equipment cleaner.) 6. Place your tube in the microcentrifuge with the filled side toward the outer margin of the chamber. Because the centrifuge spins at high speeds, the chamber must be balanced by placing tubes evenly in the chamber. Upon loading the samples into the chamber, always counterbalance your capillary tube by placing another sample directly across from yours; ie, if you start by loading the first tube in cradle #1; then put the second sample directly across in cradle #12. Then, #2 and #13; #3 and 14; etc. Make a note of the groove number into which you placed your tube. 7. Screw the inner cover on with the centrifuge wrench. (Do NOT over tighten this lid.) Close the outer lid and fasten the latch. 8. Set the timer to 4 – 5 minutes, and allow the centrifuge to spin. Do NOT attempt to open or stop the centrifuge while it is turning. Always keep loose hair and clothing away from the centrifuge. Biology 251 – Lab LAB #2 Page Five 9. After the centrifuge turns off and stops spinning, open the lid and the inner safety cover to remove the capillary tubes. Your blood sample should have straw-colored plasma at one end of the tube and packed red cells at the other end. 10. Place the capillary tube in the tube reader. Because there is a variety of tube readers, please follow the specific directions of your Lab Instructor for exact placement of the tube on the card and confirming that the positioning is correct before reading your result. 11. What is the hematocrit of your blood sample? Is it within the normal hematocrit range? (Your Instructor will share what a normal average (and ranges) value should be for a healthy dog! As you might expect, the values are slightly different than for humans.) Activity #3: Blood Smear and Wright’s Stain Technique Your Instructor will have peripheral blood smear slides prepared for you (using the dog’s blood from the Vet Tech Program) which will already be dry and ready for staining. Your Instructor will also explain briefly the technique used to prepare blood smears, starting with a single drop of blood which is then dispersed over the length of the slide in such a fashion as to “run out of blood before running out of slide” and thus creating a “feathered edge” effect. It is in this feathered-edge area of the slide that the formed elements of the blood are in a single layer suitable for viewing once stained. (In the other areas of the smear, the formed elements are mounded up on each other and there are too many layers of cells for effective viewing of individuals cells.) If any student cares to prepare his/her own smear, your Instructor will demonstrate the proper technique. All students will have a slide and will use the “Diff-Quick” staining stations at several locations in the Lab. (Note that each staining station is positioned adjacent to a sink – this is because you will be rinsing these slides and MUST be where there can be a drain for the water rinse.) At each station there is a laminated card that summarizes the steps involved in proper application of the Wright’s Stain. The steps are outlined here as well: 1. Holding your slide with your fingers closest to the end on which the blood is thickest and thus with the feathered edge away from you, you will first introduce the slide into Coplin Jar #1 with the turquoise-blue staining solution. As per instructions, you will dip the slide 5 times for 1 second each time into Jar #1. Be sure to come up out of the Jar between each 1-second dip. 2. You will now blot the excess turquoise-blue stain off on the paper-towel blotters provided at the staining station by dabbing the thin edge of the glass microscope slide onto the paper-towel. (This step insures that the solution in Jar #2 is not contaminated or diluted by too much excess of stain #1 being transferred to it.) 3. Still holding your slide with the feathered edge away from you, you will next introduce it into Coplin Jar #2 with the orangy-red staining solution. As per instructions, again dip the slide 5 times for 1 second each time into Jar #2. Be sure to come up out of the Jar between each 1-second dip. 4. Again, you will now blot the excess orangy-red stain off on the paper-towel blotters provided by dabbing the thin edge of the glass microscope slide onto the paper-towel; for the same reason as previously stated. 5. Still holding your slide as before, you will finally introduce it into Coplin Jar #3 with the very dark navy-blue staining solution. As per instructions on the card, you will dip the slide 10 times for 2 seconds each time into Jar #3. Biology 251 – Lab LAB #2 Page Six 6. After the 10th 2-second dip into Jar #3, you will position yourself over the sink and using a very gentle stream from one of the Distilled Water Rinse Bottles, you will begin at the top of your slide (closest to where you are holding it) and rinse your slide (both sides!). BE SURE NOT TO HOLD THE NOZZLE TOO CLOSE TO YOUR SLIDE, or you will risk having the stream of water lift the entire blood specimen off the slide. Rinse until no more blue color comes away with the rinse water. 7. Now, BEING SURE TO PLACE YOUR SLIDE SPECIMEN-SIDE UP, place it on your own paper-towel Place-mat at your lab desk to let it dry completely. 8. Once the slide is completely dry, you may place it on your microscope stage and begin the microscopic exam of the formed elements. See how well the staining process was tolerated by the RBCs: in other words, are the RBC’s crenated? Are they swelled into spherocytes? Does their morphology look normal? Judging the RBC’s to be normal (remember, RBC’s are NOT stained by Wright’s stain – they are already reddish color because of the pigmented portion of the hemoglobin molecules. The Wright’s stain (aka “Diff-Quick”) is taken up only by the WBC’s and platelets; however, if the staining solutions were hypotonic or hypertonic and affected the RBCs’ morphology , then the WBCs and platelets would be affected, too. If overall morphology looks good – then proceed trying to identify platelets and each of the individual types of WBCs. If morphology is poor in your slide, then trade it for one of the Explanomount prepared slides to begin your quest to identify each and every WBC you encounter in your fields of view. A differential WBC count is performed to determine the percentage of each of the five types of WBCs in a blood sample. When attempting to learn which WBCs are normally present from the greatest to least percentages, it is helpful to remember the following mnemonic: “Never Let Monkeys Eat Bananas” (N = Neutrophils; L = Lymphocytes; M = Monocytes; E = Eosinophils; B = Basophils). Because the normal percenetage of each WBC type is known, any significant abnormality in these percentages, elevated or depressed, can be indicative of particular disorders. (Numerical values for the normal range of WBCs may vary depending on the reference source, and each hospital, clinic, and textbook has slightly different read-outs on “normal ranges”.) As per our Tortora textbook, we will use the following ranges for “normal percentages of WBCs”: Neutrophils 60% – 70%; Lymphocytes 20% - 25%; Monocytes 3% - 8%; Eosinophils 2% - 4%; and Basophils 0.5% - 1%. (Note: it is impossible to find one-half of one basophil white blood cell; therefore, this is the SAME as 0% - 1%. It is NOT uncommon to find absolutely NO basophils in a single normal peripheral blood smear.) Whatever the percentage values are for the different WBCs in any one smear, the additive sum of all the percentages MUST equal 100%. This is because a “Diff count” (differential WBC count) is based upon counting 100 WBCs. The total number of each type of WBC counted, then, is its percentage in the blood sample; ie. 26 lymphocytes counted means 26% of the WBCs are lymphocytes. Activity #4: Microscopic exam of the formed elements of blood Formed elements, which make up the cellular portion, or “living matrix”, of blood, account for about 45% of the volume of whole blood. Each class of formed element has a distinctive appearance, some with uniquely colored cytoplasmic granules, and all with a characteristic shape of the nucleus (except for RBCs which are anucleated cells). Formed elements can be divided into three classes: 1. Erythrocytes (Red Blood Cells): have the function of carrying oxygen on an iron-containing molecule called Hemoglobin (when hemoglobin binds O2, it is called oxyhemoglobin). 2. Leucocytes (White Blood Cells): play a role in the immune system. The two subclasses of leucocytes are: (a) Granulocytes: cells containing visible cytoplasmic granules, including neutrophils, eosinophils, and basophils. (b) Agranulocytes: cells lacking cytoplasmic granules, including lymphocytes and monocytes. Biology 251 – Lab LAB #2 Page Seven 3. Thrombocytes (Platelets): cellular fragments involved in blood clotting. All of the formed elements have unique morphological characteristics, which can now be used to view individual cells on a blood slide called a peripheral blood smear. For this exercise, use either your own stained slide, or one of the Explanomount preparations. Be sure to examine it on high dri power (TM = 400X) and scroll through it attempting to find each of the formed elements. Note: you may have to find a second slide to locate certain cells, because some types, such as basophills and eosinophils, are rare to find even one! Refer to Figure 12.34 in your Atlas for reference. Activity #5: ABO and Rh Blood Groups Your blood type is determined by genes inherited from your parents, and it does not change during your lifetime. Each blood type is due to the presence or absence of specific molecules on the surface of the erythrocytes. These molecules, called antigens, are like cellular name tags that inform the immune system that your cells belong to “self” and are not “foreign. The surface antigens on erythrocytes can also be called agglutinogens. Each blood group also has antibody molecules, called agglutinins, present in the blood plasma. The agglutinins (antibodies) will attach to agglutinogens (antigens) of foreign blood cells and cause hemolysis of the erythrocytes. More that 50 different blood systems occur in the human population. In this section, you will study the two most common blood systems: the ABO and the Rh blood groups. Each blood group is controlled by a unique ene so that your ABO blood type does not influence your Rh blood type. There are four blood types in the ABO system: A, B, AB and O. Two surface agglutinogens, A and B, occur in different combinations to determine the ABO blood type. Type A blood has the A agglutinogen on the erythrocyte surface; Type B blood has the B agglutinogen, Type AB blood has both A and B agglutinogens, and Type O blood has neither A nor B agglutinogens. (Please note here that the “O” for Type O really stands for “neither”, “nada”, “zip”, “zilch” in terms of agglutinogens of the A or B variety. THERE IS NO “O” agglutinogen! ) So, blood types are named for the agglutinogen(s) PRESENT ON THE ERYTHROCYTE surface. But, this is just half of the story: Also, present in the blood plasma are agglutinins. Your plasma agglutinins will not react to your own erythrocytes. However, if a different type of erythrocytes is introduced into your bloodstream, your agglutinins will attach to the agglutinogens of the foreign blood cells and cause the cells to clump or agglutinate. Hemolysis (or bursting) occurs, and the intruding cells are destroyed. Type A blood has A agglutinogens on the RBC membrane surface and type anti-B agglutinins in the plasma. (The anti-B antibody will not react with the type A antigen.) Type B blood cells are covered with the B agglutinogen, whereas the plasma contains the anti-A agglutinins. Type AB blood is unique in that each red blood cell contains both the A and B agglutinogens on the RBC membrane surface. Type AB blood lacks the anti-A and the anti-B plasma agglutinins. Type O blood cells lack both agglutinogens, but has both anti-A and anti-B plasma agglutinins. To determine an ABO blood type, the presence of agglutinogens is detected by adding drops of anti-sera that contain either the anti-A or the anti-B agglutinins. The serum agglutinins will react with the coarresponding agglutinogen on the RBC surface. For example, the anti-A agglutinins will react with the A agglutinogens found in type A blood. The blood will clum or agglutinate as more antibodies react with the antigens. The Rh blood group is named after the Rhesus monkey because this is the organism in which the blood group was first identified and isolated. Rh blood groups include Rh positive (+) and Rh negative (-). Although this Biology 251 – Lab LAB #2 Page Eight blood system is separate from the ABO system the two are usually used together to identify a blood type. For example, a blood sample may be A+ or A-, AB+ or AB-, etc. Unlike the ABO system with two cellular agglutinogens, the Rh system has only one cellular agglutinogen, called the D agglutinogen – and your cells either have it (+) or they do not have it (-). A single Rh plamsa agglutinin also occurs, designated anti-D. The D agglutinogen is only present on RBCs that are Rh positive; Rh negative individual lack the D agglutinogens. Rh positive blood cells are covered with the D agglutinogens, and, of course, their plasma lacks the anti-D Rh agglutinins. Interestingly, the Rh negative individual also lacks the anti-D agglutinins. However, if the Rh negative blood is exposed to the Rh D agglutinogens in Rh positive blood, that person’s immune system will produce the anti-D agglutinin! (This becomes clinically significant in cases of and Rh negative woman becoming pregnant with an Rh positive fetus. Rh positive women WILL NOT ever have to deal with Rh incompatibilities in their pregnancies, because an Rh positive person’s immune system will not ever produce anti-Rh agglutinins.) In terms of the genetics of your blood type, remember that in the study of genetics for any trait, there are two properties that one must keep in mind: (1) Phenotype – the physical expression of a specific trait, such as hair color or blood type, based on genetic and environmental influences. Traits such as “brown hair” and “blue eyes” refer to an individual’s phenotype. To determine the phenotype of blood cells, we perform blood typing with antisera (as discussed above). The result of that blood typing procedure (for example, A+, O-, or AB -) is the phenotype. (2) Genotype – the genetic makeup, as distinguished from the physical appearance, of an organism. It is what the cell looks like genetically. If you were to perform DNA analysis, the genotype is what you would be investigating. Also remember, our cells (except for gametes) are diploid (2n) cells: that is, for all genes in the body, we have two copies of each gene: one from our maternal side and one from the paternal side. For blood, we cannot determine the precise genotype without doing DNA analysis. But, if we know the phenotype, we can determine possible genotypes. We know the following facts: a. From each parent, we can inherit one of the following ABO genes (alleles): (1) IA: codes for A agglutinogens; (2) IB: codes for B agglutinogens; or (3) i: codes for neither A nor B agglutinogens. b. From each parent, we can inherit one of the following Rh factor genes: (1) Rh gene: codes for the Rh agglutinogen, denoted as “+”; or (2) No Rh gene: does not code for Rh agglutinogen, denoted as “-“. Let’s use the following table to summarize the information about which phenotypes accompany which possible genotypes. Fill in the remainder of the table, following the pattern from the first two examples: GENOTYPE(S) A A I I ++, IBIB++, A A A PHENOTYPE A I I + -, I i++, I i+ IAIA- -, IAi- IBIB+ -, IBi++, IBi+ - A+ AB- i i ++, ii+OAB+ IAIB- -