Patient: Mr PP Age: 50
advertisement

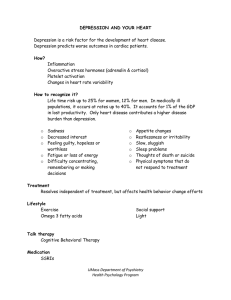
Patient: Mr PP I. Age: 50 Gender: Male Clinical Summary: HTN, Systolic HF, and CAD: Mr PP has had multiple issues with his heart starting in the mid 2000s. He has had a heart attack, three stents, cardiac ablation 3/08, and currently requires a pacemaker. He has had 5 cardiac procedures in the last year including replacing his pacemaker. Mr PP has been on disability for a few years now stemming from his cardiac issues. Systolic HF: Patient is ACC/AHA Class C and NYHA Stage III which gives him a SORT A recommendation for taking digoxin1. Patient also has a pacemaker due to EF<35 and recommendations consistent with the NICE guidelines2. His EF as of 1/11 is 20%. HTN: Based on patient’s diabetes and CHF, patient is currently meeting SORT A recommendations for BP control of <130/80 using an ACEI as first line treatment and loop diuretic as second line3. Patient’s BP was 120/70 on last office visit. CAD: In addition to a beta blocker, patient is also taking lipid lowering agents for his CAD. Patient is taking omega 3 fatty acids which has a SORT C recommendation and has been shown to reduce mortality specifically in patients whose lipids are controlled on other medications and have had an MI in the past4. Medication Regimen: Patient currently takes digoxin 0.125mg 1 q am, carvedilol 6.25 BID, furosemide 80 mg BID, metolazone 5 mg prn, atorvastatin 20 mg qhs, potassium chloride 20meq 1 qhs, nitrostat 0.4mg prn, omega 3 fatty acids 1000mg q am. Atrial Fibriliation: Patient has paroxysmal afib s/p cardioversion and multiple cardiac problems detailed above. His CHADS2 score is a 3 giving him a moderate risk of a thromboembolic event and guidelines support treating these patients with Warfarin instead of clopidogrel plus aspirin due to bleeding risk SORT A5. Though warfarin has been shown to be superior to aspirin plus clopidogrel, patient is currently on triple therapy due to the need to prevent stent thrombosis while maintaining longterm anticoagulation. This triple therapy, not surprisingly, increases risk of bleeding6. His current medication regimen includes coumadin 2mg M,F and 1mg every other day, clopidogrel 75mg tablets qam, 81mg aspirin, amidoarone 200mg qam Type 2 Diabetes: Diagnosed 9/10, patient’s A1C was 6.1 on 7/12. Mr PP began having vision problems and blood sugars in the 300s on 11/12 stemming in part from not being able to afford his medication for a short period of time. Patient is due for repeat blood work in week to assess if he’s at goal for AIC of <7 SORT B and goal LDL of <100 SORT A7. Mr PP has also had a relatively stable but elevated creatinine of about 1.5 and has not been on metformin for that reason. Patient takes Ramipril 2.5mg bid, Lispro 40 units TID after meals, Glargine 45 units q am, 3pm, and 85 qhs. Anxiety/Major Depression: Diagnosed 7/12 stemming from major life stressors including a recent release from prison with ongoing legal troubles, estrangement from wife and family, and loss financial income related in part to being disabled. Patient seen at Holly Hill Mental Health Hospital 1/5/13 for evaluation of his depression and at UNC’s ED on 1/7/13. Patient currently endorses anhedonia, sleeping over 20hrs a day, crying spells, fatigue, guilt, and sadness. There have been no studies showing the superiority of any antidepressant agent class over another8. Mr PP was referred to a psychiatrist on his last office visit to help manage his depression/anxiety. There are SORTB recommendations to augment a current medication regimen for depression with another class8 which was done about a month ago adding buproprion to Mr. PP’s current regimen. He is currently taking Citalopram 20mg q am, Buproprion ER 150 2 q am and 1 qhs, Temazepam 30mg qhs for sleep, Diazepam 5mg BID. II. III. Questions raised by preceptor: Patient is constantly tearful on visits and it has been difficult to get his chronic medical problems under control with his depression controlling his life. Are there any suggestions to better control his depression? Patient has been having a lot of financial trouble making it difficult for him to get his medications. We have him on a medication assistance program but are there any other community resources available to help him with his care? Reflect on the Patient: I first met Mr PP on 1/9/13 for a depression f/u. He cried most of the interview as he told his story about having many chronic illnesses which led from him going from a high paying engineer job to being on disability. He struggled to make ends meet on disability so he chose to grow marijuana for distribution in his basement though he denies ever using it. The police later found out and he and his second wife were arrested on felony charges. After using all his funds including money saved up for his children in his first marriage, he was released from jail but was now alienated from all his family members who refused to have anything to do with him. Patient states his greatest fear is being alone and he has tremendous guilt, sadness, and anhedonia. The interview ended that day with his physician and me recommending he get more involved in his church, consider couples counseling and we referred him to a psychiatrist. I went and visited Mr. PP at his home the next day with the intention on giving him some more resources for his depression but focusing this visit on his chronic medical problems which have not been well addressed in several months due to his depression and recent release from prison. Despite having an appointment with the patient, I had to call and text over 8 times before he picked up the phone. He had been sleeping his usual 20hrs that day. I came over to visit the patient and it was clear to me that depression was clouding all his thoughts and focusing this visit on his depression was going to be the best use of his time. So I let him talk and we did for about an hour in which he was mostly tearful. I learned more about why he felt so alone for his parents and only sibling had died years ago, his wife won’t look at him, and he had just ended his relationship with his only and closest friend due to a misunderstanding between the friend and Mr. PP’s daughter. Mr. PP values family above everything and wants to do anything he can to have his family back. I tried some motivational interviewing on this patient with limited success but left the encounter giving him some goals before his next office visit. Patient felt grateful that I let him talk for so long, and I left that encounter with a great appreciation for why it’s so difficult to control patient’s multiple comorbidities when their lives are simply so hectic and clouded by depression. IV. V. THREE Key suggestions to improve the care of individual patient: Animal Shelter: Recommend that patient attends local animal shelter at least once a week. Patient feels alone and “doesn’t even know how to make friends and talk to people.” He says he loves dogs and was considering getting a pet so that he doesn’t feel lonely. Mr PP is having significant difficulty taking care of himself and his finances do not allow him to realistically own a pet at this time but visiting the animal shelter and doing some sort of unofficial animal therapy could be very beneficial. Animal therapy has the potential of drawing attention away from Mr. PP’s problems, and giving him a chance to feel accepted by another living creature. Some of the details of what animal therapy is can be found here: http://www.helpfordepression.com/article/ alternative- methods/animalassisted-therapy. In addition, this could help him get out of the house and not spend over 20 hours a day in bed. Management of Anxiety and Sleep: Patient has had difficulties sleeping in the past but his current depression symptoms seem to be associated with increased somnolence. Patient is also having difficulties affording all his medications and reducing or even discontinuing his benzodiazapines may be a viable option for reducing his costs and improving his health. Cognitive behavior therapy has been shown to be as effective as medication and producing more sustainable outcomes concerning insomnia SORT B9. Cognitive behavior therapy also has a SORT A recommendation for initial treatment of insomnia9. If patient is using benzodiazapines for anxiety component, would still recommend using SSRI or SNRI instead for they have been shown to be more beneficial for generalized anxiety disorder than buspirone or benzodiazapines SORT A10. Addressing other medical problems: Until patient’s depression becomes better controlled, it is going to be very difficult to manage his other medical problems. Patient’s current financial issues and ongoing legal battle complicate the situation but he is currently in Medicare Part A from disability and a pharmacy assistance program to help with the cost of his medicines and health care. With the exception of the patient’s depression, his other medical problems are relatively well controlled as long as the patient has access to his medicines. Besides better control of depression, would recommend patient joins his local YMCA in Garner. The YMCA offers financial assistance programs and many of their health classes are free. Patient currently has a car so driving to the YMCA and trying to regain some of his cardiovascular stamina and improve his overall physical and mental health through exercise could be extremely beneficial: http://www.ymcatriangle.org/membership/financial-assistance-membership. Yoga, Tai Ch, and meditation have been shown to be a SORT B therapeutic option for depression and anxiety11. Exercise is also an effective treatment option for depression in adults but only minimal evidence to support its use in anxiety 11. Chart Review a. These suggestions was based on a registry created using all the males seen in the practice since implementation of EHR (4 months ago) who had the diagnosis on DM2, HTN, Depression/Anxiety for a total of 10 patients. b. My chart review showed no objective measurements of the patients’ depression symptoms c. Every patient that fit the parameters of my registry was either obese or morbidly obese (BMI 31-43.2). VI. ONE Key suggestions (in order of priority) to improve the care of the patient as part of a population: Diabetes Registry: With the new electronic medical record being less than 6 months old, the practice is still adjusting to using the system, transitioning paper charts, and capturing data in a way that it can be tracked by meaningful use and coded correctly. In the next few months as providers and staff become more knowledgeable about the system and its capabilities, I recommend the next step being creating registries for diabetic patients to consistently track, improve, and assess provider’s management of their population’s diabetes. By using registries, providers can better coordinate care and treat their patients. Systems can eventually be put in place allowing staff to easily find patients who are not at goal on a certain diabetes measures or not up to date on a screening exam and f/u with these patients. These registries can also be used to help the practice have a diabetes recognition program with the National Committee on Quality Assurance and improve provider’s payment rates. I would also recommend using registries that generate automatic letters to patients for they have been shown to be more effective than registries that do not generate these automatic letters14. As of right now, it is very difficult to do a chart review and quickly find out patient’s last A1C, LDL, eye exam, foot exam, etc. Making sure that these pieces of information become inputted in the computer system in a way that it can auto populate will be the next challenge the practice faces. More information on how to set up a registry can be found here: http://www.aafp.org/online /en/home/ membership/initiatives/pcmh/qualitymeasures/installsystem/patientregistry.html. In addition, patients with diabetes are at higher risk for depression. As of right now, there is no systematic process in place for the management of patients’ depression and a chart review showed no objective measurements of the patients’ depression symptoms. A registry could also help keep track of screening and treatment. The US preventative Services Task Force in 2009 recommended screening adults for depression when staff-assisted depression care supports are in place but recommended against screening when these supports are not in place. Since staff-assisted depression supports are currently limited, I recommend routine screening only for patients with a PMH with a diagnosis of depression. This could be implemented by have nursing staff ask the PHQ-2 to these patients and following up with a PHQ-9 if positive. The PHQ-2 is quick and would not put a significant burden on staff to have another assignment added to their responsibilities and the PHQ-9 could be filled out while patients wait for the provider so it does not slow the flow of the clinic. The sequenced treatment alternatives to relieve depression trial (STAR*D) showed that measurement based care of depression is feasible in primary care. Men are believed to have the same prevalence of depression as women but are diagnosed and treated less often13, having a staff-assisted depression support system in place would be a great long term goal for the office to help eliminate this discrepancy in the sexes as it concerns depression. VII. References: 1. Spencer A Morris. Digoxin Therapy for Heart Failure: An Update. Am Fam Physician. 2006 Aug 15;74(4):613-618. 2. Mara Lambert. NICE Updates Guidelines on Management of Chronic Heart Failure. Am Fam Physician. 2012 Apr 15;85(8):832-834. 3. American Diabetes Association. Executive summary: standards of medical care in diabetes— 2009 [published correction appears in Diabetes Care. 2009;32:754]. Diabetes Care. 2009;32(suppl 1): S6-S12. 4. Dietary supplementation with n-3 polyunsaturated fatty acids and vitamin E after myocardial infarction: result of the GISSI-Prevenzione trial [Published correction appears in Lancet 2001;357:642]. Lancet. 1999;354:447–55 5. Cecilia Guitierres, Daniel G Blanchard. Atrial Fibrillation: Diagnosis and Treatment. Am Fam Physician. 2011 Jan 1;83(1):61-68. 6. Khurram Z, Chou E, Minutello R, Bergman G, Parikh M, Naidu S, Wong SC, Hong MK(2006) Combination therapy with aspirin, clopidogrel and warfarin following coronary stenting is associated with a significant risk of bleeding. J Invasive Cardiol 18:162–164. 7. Executive Summary: Standards of Medical Care in Diabetes—2012. Diabetes Care January 2012 35:S4-S10; doi:10.2337/dc12-s004 8. Stephen M. Adams, Karl E Miller, Robert Zylstra. Pharmacologic Management of Adult Depression. Am Fam Physician. 2008 Mar 15;77(6):785-792. 9. Parul Harsora, Jenniver Kessmann. Nonpharmacologic Management of Chronic Insomnia. Am Fam Physician. 2009 Jan 15;79(2):125-130. 10. Generalized Anxiety Disorder: Practical Assessment and Management. Am Fam Physician. 2009 May 1;79(9):785-791. 11. Atezaz Saeed, Diana Antonacci, Richard Block. Exercise, Yoga, and Meditation for Depressive and Anxiety Disorders. Am Fam Physician. 2010 Apr 15;81(8):981-986. 12. Anderson L, Lewis G, Araya R, Elgie R, Harrison G, Proudfoot J, Schmidt U, Sharp D, Weightman A, Williams C. Self-help books for depression: how can practitioners and patients make the right choice? Br J Gen Pract. 2005 May;55(514):387-92. 13. Royal College of Psychiatrists (1998), Men behaving sadly. Available: www.rcpsych.ac.uk/pdf/MenBehavingSadly.pdf 14. Stroebel RJ, Scheitel SM, Fitz JS, Herman RA, Naessens JM, Scott CG, Zill DA, Muller L. A randomized trial of three diabetes registry implementation strategies in a community internal medicine practice. Jt Comm J Qual Improv. 2002 Aug;28(8):441-50. 15. University of Oxford (2009, March 20). Moderate Obesity Takes Years Off Life Expectancy. ScienceDaily. Retrieved January 29, 2013, from http://www.sciencedaily.com /releases/2009/03/090319224823.htm 16. Wing RR, Phelan S. Long-term weight loss maintenance. Am J Clin Nutr. 2005;82(1 suppl):222S–225S 17. Jennifer Croswell, Shelly Luger. Screening for and Management of Obesity in Adults. Am Fam Physician. 2012 Nov 15;86(10):947-948. 18. Samule Grief, Rosita Miranda. Weight Loss Maintenance. Am Fam Physician. 2010 Sep 15;82(6):630-634. 19. Matt Brown. Medicare Will Pay for Obesity Screening, Intervention, Says CMS:Financial Impact on FPs Still Unclear. http://www.aafp.org/online/en/home/publications/news/ newsnow/practice-professional-issues/20111207obesitypay.html