Patient: JS Age: 43 Gender: Female
advertisement

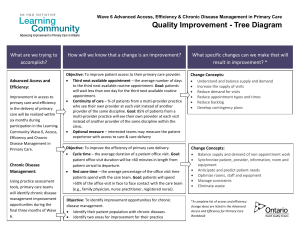
Patient: JS Age: 43 Gender: Female I. Clinical Summary: a. Chronic pain: Began in September 2011. Has experienced both low back pain, likely due to L5-S1 anterolisthesis, and shoulder/neck pain of unclear etiology. Has been managing pain with physical therapy exercises and as needed NSAIDs and muscle relaxants. b. Depression: Began following father’s death in 2009. Prolonged period of bereavement with frequent crying spells. Treated with Lexapro briefly, which stopped her crying, but did not make her feel “better.” She feels that her perspective changed after that experience. c. Asthma/Exercise induced bronchoconstriction: Diagnosed 11/8/12 (on the day of our interview) after experiencing increased dyspnea on exertion over the preceding months. She was started on an albuterol inhaler PRN and Advair daily. d. Pituitary microadenoma: Diagnosed during evaluation for blurry vision this year. Felt not to be causing vision or other symptoms. e. B12 deficiency: Unknown etiology, treated with monthly B12 injections. Currently asymptomatic. II. Questions raised by preceptor: a. My preceptor was particularly interested in the role that changes in JS’s family life have played in her health care. i. How did the death of JS’s father affect her mental health and her health overall? Are there resources nearby that could have helped her manage that transition more easily? ii. What strategies can JS use to control her pain? iii. How is JS dealing with her mother’s current health problems? Is she experiencing increased stress due to being a caregiver? III. Reflections on Attempting to Understand the Patient I met JS on my second morning in clinic, when she came in for an exercise tolerance test due to increasing shortness of breath on exertion. I was surprised that Dr. McManus had recommended her as a patient for the CARE assignment, because she was a young, athleticappearing woman, hardly the stereotypical image of the patient with multiple chronic medical conditions. But Dr. McManus was interested in how some recent social stressors had affected her health, and we agreed to meet later in the day to talk. That afternoon, I asked JS to tell me a little bit about herself, she did not hesitate to tell me all about growing up in the area and meeting her husband in her first year of college. She was effusive when talking about her family life growing up and clearly proud of her 18 year-old son and 21 year-old daughter. She lit up when talking about the business she owns and operates in Sanford. When asked about prior health issues, JS felt that she had been extremely lucky. She said she had always been healthy, without any chronic medical complaints. She had a lawn mower accident in 2000, which resulted in leg and back pain, but this resolved quickly. Then, her father was diagnosed with cancer. She and her family took care of him diligently throughout his illness, traveling back and forth to the hospital and spending time with him whenever possible. Despite their hopes, he passed away suddenly three years ago after succumbing to infection. For JS, it was, not surprisingly, a major blow. “No one will ever love me like my daddy did,” she told me. After months of taking care him, she felt the let-down even more acutely. “In a crisis, I’m fine,” she added, “it’s the part afterwards that’s hard.” In the aftermath, she experienced a prolonged bereavement. Dr. McManus trialed her on Lexapro during the holidays, which she said did not change her mood, but made her feel “stifled.” While I did not ask about mood symptoms, she said that her father’s death had changed her perspective, and that, “I’ve got plenty of years left to work and do things but I sort of…don’t want to.” On top of all of this, her back and leg pain returned in November of last year, to the point that she was limiting her activity, both at work and at home. Her job involves being extremely active, and she has felt the need to hold back and allow others to take over parts of the job that she enjoys doing. She currently manages her pain with a combination of NSAIDs and physical therapy, but finds that she often does not have time for physical therapy between taking care of things at home and at work. As she said to me, the more stressed she feels at work, the less she keeps up with her PT, and the worse her back feels. Though her mother has recently been dealing with worsening health, JS says that she is mostly concerned about her mother being alone after losing the great love of her life. She was teary over the thought of her mother spending hours in her house at a time, with “nothing to do” and no one to speak to. This feeling of guilt over her mother’s situation has only added to her recent stress. From my time with JS, I got the impression of a woman very committed to others in her life, potentially to her own detriment. She feels pulled in multiple directions ever since the death of her father, trying to make enough time to spend with family while not sacrificing the work that she loves. She is also the type of person who will tolerate issues without complaint; she describes herself as a patient person who does not seek help until things begin to “interfere” with her life. IV. THREE Key suggestions (in order of priority) to improve the care of individual patient: a. Exercise should continue to be a major part of JS’s treatment plan, both for her chronic pain and for mood symptoms. The Institute for Clinical Systems Improvement (ICSI) guidelines on the treatment of chronic pain state that a graded exercise program should be part of initial treatment in all patients to both improve function and decrease pain1. Likewise, the most recent American Psychiatric Association (APA) guidelines on the treatment of depression suggest that exercise can provide benefits for mood symptoms2. JS has always enjoyed being an active person, and gets exercise both at work and through Cross Fit. She should be encouraged to continue to enjoy these activities and not be limited by her recent diagnosis of exercise induced bronchospasm. Incorporating the movements she learned during her previous physical therapy into her normal exercise routine may help her to manage her symptoms more consistently using stretches that she has found effective in the past. b. If JS is interested in working in a more structured environment, cognitive behavioral therapy (CBT) might be a useful tool for doing so. CBT is one of the cornerstones of treatment for depression, and is effective as monotherapy for mild depression or in combination with pharmacotherapy1. While its use for depression is broadly recognized, it’s effectiveness in the treatment of chronic pain may not be as well known. However, CBT may improve function and reduce pain in patients with chronic pain2. Since stress appears to play a significant role in JS’s life, CBT focused on stress reduction would likely be very effective. Multiple providers in both Siler City and Sanford provide CBT, so JS would be able to find a provider she feels comfortable with. Dr. McManus has already begun some cognitive behavioral interventions in the office by acknowledging JS’s pain and asking her to take an active role in its management. c. When we spoke, JS mentioned that she does not mind taking medications, but would prefer other strategies for controlling her pain. Complementary and alternative modalities may thus be a good option for managing her pain. Good evidence exists for the effectiveness of massage for the treatment of low back pain, with RCTs showing a benefit over patient education alone3, although this benefit exists largely over the short term (6 weeks or so). The studio Rejuvenate is less than a mile from Dr. McManus’s office in Siler City and provides massage therapy for all types of indications. Even just a few sessions may provide a long-lasting benefit for JS. Another modality that may be of use for the treatment of JS’s pain is acupuncture. While the evidence is less strong than it is for massage, acupuncture has been shown to be of benefit in patients with back pain1. Acupuncture may also be of benefit for depressive symptoms, although the APA does not currently recommend it for treatment2. Stillpoint Acupuncture is actually found in the same location as the Rejuvenate massage studio in Siler City. They offer a community clinic weekly on Wednesdays from 2-6 in which multiple patients are treated at the same time, with fees on a sliding scale. This would be an affordable way for JS to receive non-pharmacologic treatment for her back pain and, potentially, her depression. V. Chart Review a. The charts of a group of ten patients with chronic pain and depression were reviewed. Generally speaking, they were older women with multiple medical problems. Nine out of the ten patients were female, with an average age of 77.2 years. Each was on an average of 6.8 medications. b. The patients in the group studied averaged 12.3 visits per year, more than one a month. VI. ONE Key suggestions(in order of priority) to improve the care of the patient as part of a population: a. The patients in the group studied averaged 12.3 visits per year, more than one a month. Given that they were medically complicated, many of these visits were necessary. However, some might be effectively and efficiently replaced with a group visit for patients with similar problems. The current evidence suggests that group visits are relatively effective as part of a treatment plan for chronic pain5. Though depression has not been directly studied, group visits do not appear to be as effective in its treatment, though they have been repeatedly found to improve quality of life in patients with chronic illness6. Group visits certainly present a great deal of effort up-front, during implementation, but may provide long-term savings in terms of time. The Greater Lawrence Family Health Center has a guide for practices seeking to set up group visits, which can be obtained at the following URL: http://goo.gl/qcjsK. Our clinic has a large conference room that would comfortably fit 20 patients and has several times throughout the week that it is not in use. The group visit model would also be a great way to introduce patients to exercise. As discussed above, exercise has proven beneficial for both depression and chronic pain. Given the average age of the patients reviewed, many of the patients could benefit from the group exercise classes at the Western Chatham Senior Center, currently scheduled for 11 AM each Tuesday, Wednesday and Thursday (http://goo.gl/QlLAc). Asking patients to sign up to go on particular days might boost their motivation by providing them a group with whom to share the experience, and might form the connections to facilitate the introduction of group medical visits. I also spoke with the staff at the senior center and they would be willing to do an introduction for a class of patients at my preceptor’s office. They could do one class for free and then $20 each additional class. References 1. 2. 3. 4. 5. 6. Hooten WM, Timming R. Health Care Guideline: Assessment and Management of Chronic Pain. Fifth ed: Institute for Clinical Systems Improvement; 2011. Gelenberg AJ, Freeman MP, Markowitz JC, et al. Practice Guideline for the Treatment of Patients With Major Depressive Disorder. Third ed: American Psychiatric Association; 2010. Cherkin DC, Eisenberg D, Sherman KJ, et al. Randomized trial comparing traditional Chinese medical acupuncture, therapeutic massage, and self-care education for chronic low back pain. Arch Intern Med. Apr 23 2001;161(8):1081-1088. Maizels M, McCarberg B. Antidepressants and antiepileptic drugs for chronic non-cancer pain. Am Fam Physician. Feb 1 2005;71(3):483-490. Gaynor CH, Vincent C, Safranek S, Illige M. FPIN's clinical inquiries. Group medical visits for the management of chronic pain. Am Fam Physician. Dec 1 2007;76(11):1704-1705. Jaber R, Braksmajer A, Trilling JS. Group visits: a qualitative review of current research. J Am Board Fam Med. May-Jun 2006;19(3):276-290.