Mistreatment Response Program
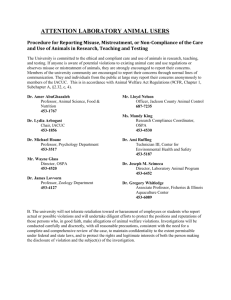
advertisement
Planning and Implementing a Mistreatment Response Program in an Acute Care Setting Acknowledgement: From original materials prepared by Corrine MunozPlaza, MPH and Jan Capps, MPH, The Beacon Program, UNC Healthcare. History. The Beacon Program was funded in 1998 by the North Carolina Governor’s Crime Commission to develop the Effective Practices for Healthcare Response to Domestic Violence project. The goal of the project was to provide technical assistance to five healthcare organizations throughout North Carolina in the planning and development of each site’s own domestic violence response program. While this website addresses the issue of elder mistreatment, mistreatment happens to persons of all ages. The information in this guide applies to a program in an Acute Care setting for all ages. Chapter 1: Plan Chapter 2: Develop Chapter 3: Implement Chapter 1: Plan PLANNING FOR A Mistreatment Response Program IN THE ACUTE CARE SETTING Gain Administrative Support Gaining “buy-in” from your organization administrators is a necessary step to success. Healthcare organizations have a responsibility to respond to both patients and employees who are mistreated or are victims of domestic violence. Which administrators might be included: President or CEO Director of Patient Services Director of Women’s and Children’s Services Clinic Managers First Meeting Topics Reason for healthcare response – Explain why you think the organization needs a response program for issues of mistreatment and domestic violence. Present statistics from your organization or from the community that demonstrate the need. Tell administrators what other data you need and how you plan to collect it before you proceed. Cite community need and current response. Accreditation standards and guidelines – Outline standards from organizations such as the Joint Commission for the Accreditation of Healthcare Organizations (JCAHO) and guidelines from the American Medical Association. [PROVIDE WEB CITATIONS] Domestic violence program components – Provide examples of other response programs functioning in organizations similar to yours. Implementing a plan – Present a plan for a response program. Include the personnel, time and funds it will take. Form a Multidisciplinary Planning Team Inside the acute care setting – A team made up of interested people from various disciplines representing multiple departments will know about different issues that need to be addressed and will have different solutions to offer. If possible, one employee should be allowed time away from regular duties to coordinate and lead the team. Outside the acute care setting – Include representatives of community agencies who have expertise in the mistreatment and domestic violence. Assess the Situation Assessments take time and can use precious resources. Your organization may believe they know what they need to do, but proceeding without an assessment may lead to wasted effort and overlooked possibilities. Assessing the current situation and the needs for improvement will: Provide a picture of the current response to mistreatment and domestic violence Determine gaps in the existing services Assess how best to allocate available resources Determine the availability of community resources Start a dialogue with agencies who serve those who are mistreated or are the victims of violence. Patient Assessment Ask patients to determine the type of system that will respond to their needs. Determine who (male/female, young/old, racially diverse) and how many patients to sample. You will want to explain why you are asking these questions. Questions might include: Would you discuss mistreatment or domestic violence (someone hurting you or someone you care about and/or someone not providing the care they should) with your healthcare provider? What might keep you from talking to your healthcare provider about mistreatment or domestic violence? Have you ever been asked about mistreatment or domestic violence by a healthcare provider before? Who would you could call for help if you or someone you know were a victim of mistreatment or domestic violence? Possible barriers to patients reporting mistreatment or domestic violence Fear that the abuser will find out Fear that others will find out Shame that this has happened Concern that the healthcare provider would not believe them or not care Belief that talking won’t do any good Think the topic is too personal From a 1998 survey of piloted by the Effective Practices for Healthcare Response to Domestic Violence in 4 NC healthcare organizations. Clinician Assessment Survey a sample of staff that has contact with patients, not just physicians and nurses. Ask about their knowledge of and encounters with mistreatment or domestic violence, especially in regards to patients, to determine what the staff knows and what they do when they encounter a patient who they believe has been mistreated or is a victim of domestic violence. Plan to train these staff when a response program is in place. Questions might include: What do you ask patients about being mistreated or if anyone is hurting them? What might keep you from asking about mistreatment? What do you do if a patient tells you they are being mistreated or hurt? What groups, either in the organization or in the community, help people who are mistreated or are victims of domestic violence? Do you refer patients to these groups? What do you consider your ethical or professional responsibility in identifying, assessing and providing appropriate referrals to patients who are mistreated or are victims of domestic violence? Most patients surveyed think their provider should ask about mistreatment or domestic violence and said they would be comfortable talking to a provider. Patients want their providers to give them information and advice about resources (including going to a shelter or to the police). From a 1998 survey piloted by the Effective Practices for Healthcare Response to Domestic Violence in 4 NC healthcare organizations. Healthcare Organization Assessment Assess the organization to determine what services are currently offered and what new services are needed. These questions might be directed at the administrator who has greatest knowledge about the current services. Questions might include: How does the organization serve victims of mistreatment or domestic violence? What improvements does the organization need to make? What resources are available to address the need? Between 32% and 75% of providers agree that clinicians should ask women patients about abuse as part of the physical exam or history taking. Yet only 5% to 19% believe they are well prepared to counsel abused women and 9% to 23% are well prepared to assist with a safety plan. From a 1998 survey by the Effective Practices for Healthcare Response to Domestic Violence in 4 NC healthcare organizations. Community Resources Assessment Call on community agencies and organizations who address the issues of mistreatment and domestic violence. Support from these agencies may prove invaluable in developing a successful program in the healthcare setting. Some questions to ask include: What services do you offer? What gaps in services exist? What can the acute care setting do to meet the needs of patients? How can we best collaborate? Intervention Models Primary Providers Healthcare providers are trained to ask their patients about mistreatment and domestic violence, assess their safety and needs, document the abuse, and provide referrals and follow-ups as part of routine care for patients. To provide this level of care, healthcare providers are trained in communication and counseling skills and knowledge on a range of issues specific to mistreatment and domestic violence. Providers can refer their patients to local programs to provide follow-up counseling and support programs. Existing Staff A sufficient number of designated hospital or practice staff (e.g., patient advocates, case managers, social workers, nurse clinicians) are specifically trained to provide crisis intervention, safety assessment and planning, counseling, referral and follow-up as part of their clinical duties. The primary providers refer identified patients to members of the response team. Mistreatment Response Program Healthcare providers inquire about abuse and refer patients to an on-site program for further assessment and intervention. (The Beacon Program uses this model.) While the primary provider can offer initial assessment, documentation and referral, an advocate can provide more extensive services as needed. If an advocate is not available 24 hours a day, providing access to initial crisis intervention and advocacy over the telephone is another alternative. Pros and Cons of Each Model Primary Providers Pros A good choice for agencies with limited resources. Requires a strong working relationship between the healthcare agency and the local service agencies. Cons Providers must provide assessment, intervention and counseling services in the healthcare setting in addition to their other duties and without dedicated staff to assist and follow-up. Existing Staff Pros Limited staff and financial resources are necessary Providers identify the need and triage the patient to the staff designated to provide comprehensive services in the organization. Cons Busy staff must add these duties to those they already perform. On-Site Advocacy Program – a Mistreatment Response Program Pros A designated staff person is on call and responds to referrals from primary providers throughout the healthcare organization. The advocate provides assessment, intervention, documentation and referral services. Takes the pressure off providers by having a staff member handle many services. Streamlines the services offered rather than relying on a large number of primary providers who may have differing methods and abilities regarding the issues. Cons Requires sufficient financial resources to fund specialized program staff and services. Paying for the program Chapter 2: Develop DEVELOPING A Mistreatment Response Program A Mistreatment Response Program in the acute care setting will improve the health not only of patients but also the community. Before you begin, ask yourself the following questions: What services currently exist for patients who experience mistreatment and domestic violence? Do the services which exist meet the need? If not, what additional services are needed? What can the acute care organization do to improve the identification, assessment, and intervention with patients experiencing mistreatment and/or domestic violence? How can the acute care organization raise awareness among providers and community members about mistreatment and domestic violence and about the resources for patients? Program Components – Steps to Developing a Mistreatment Response Program 1. Mistreatment Multidisciplinary Planning Team 2. Mistreatment Policies and Protocols 3. Clinical Intervention Services Identification Assessment Intervention Documentation of Abuse Discharge planning 4. Follow-up with Patients 5. Staff Training and Education 6. Patient Education 7. Community Linkages 8. Determining Program Success Domestic Violence Multidisciplinary Planning Team The team should be an ongoing source of support, consultation, and guidance for the Mistreatment Response Program. The success of the program may rest on the involvement and interest of the people chosen to be on the team. The team may need to meet more frequently in the beginning to plan and set clear goals and objectives for the program. List of team activities Select key personnel from various disciplines who are interested in working as team members. Schedule the first team meeting at a time and place convenient for most members. Let members discuss openly their ideas and develop a plan to move forward. Develop appropriate committees to address various aspects of the program, e.g., policies and protocols, staff training, services to the patients and families. Choose a team leader. Sometimes the choice is obvious and other times it may be necessary to share leadership. The leader should have time to oversee the work of the team and work well with colleagues and the community. Develop a schedule for regular meetings. Supplement meetings with electronic communication. Domestic Violence Policies and Protocols This step will establish written policies (general statements outlining how the organization plans to address mistreatment and domestic violence) and protocols (procedures providing instructions on how to respond to a specific situation). Determine how the organization defines policies and procedures and the process used in your organization to develop, approve and distribute them. An example of a policy: We screen all patients for mistreatment and domestic violence. An example of a protocol: To assure that patients have multiple opportunities to report mistreatment and domestic violence, questions are asked at multiple times: Each patient is asked at admission by the admitting personnel. Each patient is asked within 48 hours of admitting again by a nurse assigned to the patient. Patients are asked in a private, confidential setting with no family present. Questions include: o Is anyone hurting you? o Do you feel safe at home? o In the past year, have you been hit, pushed, shoved, kicked, slapped or choked by a family member or caregiver? o Follow-up questions will be added if a patient answers affirmatively. Policy: An official and consistent healthcare response to mistreatment and domestic violence. Policies should address the organization’s response on behalf of employees as well as patients who are victims of mistreatment and domestic violence. Policies should include a definition of mistreatment and domestic violence used by the organization, the organization’s mission and objectives that relate to mistreatment and domestic violence, the reason the organization addresses mistreatment and domestic violence, and the organization’s plan to address mistreatment and domestic violence – screening, confidentiality, documentation, reporting requirements, services, etc. Healthcare Organizations should develop policies that: Affirm that mistreatment and domestic violence are important health issues. Require staff to respond appropriately to victims. State that protocols are accessible to staff. Require staff to attend training. Assure patient confidentiality. Assure patient and staff safety. Protocol: The expected standard of care for patients who are mistreated or are victims of domestic violence or have a history of mistreatment or domestic violence. Protocols provide step-by-step instructions for providers and staff on how to address specific situations when treating domestic violence patients. Local area family violence groups may help with screening tools and intervention guidelines. Mistreatment and Domestic Violence Protocols should include: The purpose and rational for the protocol. A brief statement as to how the protocol can be used and by whom, as well as why the specific protocol has been developed for this setting. Define roles for various staff including physicians, nurses, social workers, security, and patient admitting staff. Procedures and tools for routine screening. Include that all patients will be screened, when they will be screened, and where they should be screened. Procedures and tools for assessment. Tools to determine the lethality of the victim’s situation should assess the risk for further abuse and the needs that the victim may have. Safety planning tools should be available for all victims. Tools in the language of the patient with appropriate translation services will serve those who do not speak English. Procedures and tools for documentation. Decide what information will be included in the patient’s medical record (accessible to all the organization’s providers) or kept separately. Determine what documentation is legally required for those who report that they are victims. Procedures and tools for referral. Develop procedures and tools for reporting information to referral agencies. Have referral information available for victims. Community resources that might be included are safe shelter, counseling, childcare, legal services, social services, etc. Clinical Intervention Services A patient may seek medical care because of injury from mistreatment or because of other illness or injury. The patient may be uncomfortable discussing mistreatment and may have never discussed it with anyone else. Staff needs to learn techniques of asking and listening for patient concerns about mistreatment and to validate and support the patient’s situation, not trying to “cure” the problem with simple advice. Things to say: I’m sorry this happened to you. You’ve really been through a lot. You’re not to blame. Things not to say: Why don’t you just leave? I wouldn’t stand for that. What did you do to make him mad? Steps to Clinical Intervention Identification – Finding out who has been mistreated. Ask all patients about mistreatment and domestic violence (male and female, young and old) directly (rather than on a written form). Talk in a private setting. Assure confidentiality. Develop tools with questions designed to elicit various types of mistreatment. Use gender-neutral questions that do not assume heterosexuality. Ask questions directly and non-judgmentally Document the patient’s responses Possible Questions: Our staff is concerned about our patients’ safety and health so we are asking all our patients these questions. Physical abuse: 1. Is anyone hurting you? 2. Does anyone threaten to harm you in any way? 3. Do you believe someone controls (or tries to control) you too much? 4. In the last year, have you been hit, pushed, shoved, punched, or kicked by anyone? 5. Are there weapons in your house? Do you feel threatened by someone with weapons? Sexual abuse: 1. Has anyone forced you to do something sexually that made you uncomfortable? 2. Does anyone ever force you to have sex or perform sexual acts against your will? 3. Has anyone ever forced you to have sex when you didn’t want to? Emotional/psychological abuse: 1. Are you afraid of anyone? 2. What happens when you disagree with (partner/caregiver)? 3. Who makes decisions about things in your life? 4. Has anyone prevented you from leaving the house, seeing friends, working, or going to school? Financial abuse: 1. Do you control your money? 2. Has anyone spent your money on things you didn’t agree with? 3. Are you giving money against your will to anyone? Assessment: The foundation of services that are planned. Assess the safety and risk for future mistreatment: Questions regarding imminent danger: Is the person who mistreated the patient there now or likely to be there? What would the patient like you to do if the person mistreating them tries to get the patient to leave the acute care setting? Does the patient want you to call security or the police? Does the patient want to leave with the abuser or go to a shelter? Does the patient need to call someone (family member, trusted friend, religious advisor)? Does the patient have a protective order? Questions regarding long-term safety: Talk calmly and objectively about the potential for future mistreatment. Do not try to frighten patients into doing something (such as leaving their abuser) that they are not ready to do. Empower the patient to make decisions for themselves. Cover issues that have been identified earlier but in more depth. Begin to help the patient plan. Issues of particular concern that may indicate future abuse include. Access to weapons Threats of violence Substance abuse Use of violence in other situations Controlling behavior Assess coping mechanisms: Ask patients how they cope with mistreatment. Determine if they are abusing alcohol or drugs to handle physical or psychological pain. Substance abuse makes it difficult to make rational decisions and improve things for the long term. Assess health status: Document the patient’s physical health, noting any complaints that stem from mistreatment. Document other physical symptoms which may have a connection with mistreatment, e.g., headaches, abdominal pain, musculoskeletal pain. In addition to possible substance abuse, determine if the patient is depressed. If mistreatment has been sexual, evaluate for sexually transmitted diseases. Intervention Recognize the Stage of the Victim’s Relationship Not all individuals are ready to make a change even though they are being mistreated. There are several stages of recognizing the situation and changing it: The individual cannot admit that there is a problem. The victim may not see themselves as victims and may need help understanding the danger of the situation they are in. The individual admits abuse but is not ready or able to change or leave the situation. The victim may need to hear that they do not deserve the abuse and that there are resources to help. The individual is in process of changing or leaving the situation. The victim will need support for his/her decisions and may need referrals for long-term assistance such as education, childcare, and housing. Intervention may include developing a safety plan. The individual recently changed or left the situation. The victim may need support (counseling/support group) and may still need a safety plan. Develop a Safety Plan – Anyone who has been mistreated needs to have a safety plan. Refer to Appropriate Services – Let the individual know what is available in the acute care setting. Refer them to community groups who have programs to help them. TYPES OF REFERRALS THAT MAY BE NEEDED Emergency Housing Transitional Housing Food Cash Clothing Healthcare Services Substance Abuse Counseling Financial Counseling Job training and career opportunities Childcare Legal Assistance Social Services Peer Counseling/Support Groups Professional Mental Health Services Safety Plan The following suggestions may be helpful in developing a safety plan. When preparing to leave: Decide where you will go when you leave. Make arrangements before you leave for a place of refuge. Determine who would be able to let you stay with them or lend you money. If possible, do not stay with a friend of the opposite sex. This could be used against you. Open a savings account and/or a credit card in your name. Agree upon a coded message with friends and family to signal your departure. If you have children, rehearse departure with them. Plan to depart at a time when the person who is mistreating you is not present. Hide money, an extra set of house and car keys, and a bag with extra clothing. Have available the following items: o Social Security Numbers o Rent and utility receipts o Birth Certificates o Drivers license o Bank account numbers, checkbook, ATM card o Insurance policies o Marriage license o Valuable jewelry o Important phone numbers o Medications To protect yourself during violent incidents: Stay away from weapons and try to stay in a room where there is an exit. Confide in a neighbor. Ask the neighbor to call for help if you are being mistreated. Remove weapons from the area. Advise children to stay out of the conflict. Teach them how to call for help. Devise a code word to use with children, family, friends, and neighbors when you need help. Safety Discuss safety with children, family and friends. Let neighbors know the situation and ask that they call for help if they observe unsafe activities or hear a code word you have agreed on. Inform children’s school or day care about the situation. Inform someone at your workplace about the situation. Notify building security. Leave work with a co-worker or security person. Vary your routine and routes of travel. Change the times and locations where you do errands. Adapted from “Responding to Domestic Violence: A Guide for Local Health Departments.” North Carolina State Department of Environment, Health and Natural Resources. May 1996. Documentation of Mistreatment Goals of Documentation – Preserve evidence of mistreatment. Work with law enforcement if evidence may be used in legal proceedings. Provide a legal record by documenting mistreatment clearly and accurately. Demonstrate objective findings and outcomes. Maintain confidentiality of patient medical records. Types of documentation Written materials Use neutral language to describe the statements about the cause of injuries, e.g., “the patient reports” or according to the patient.” Use active language, not passive, e.g., “The patient reports. . .” rather than “The patient was punched. . . “ Tape-record statement Record a brief statement from the patient regarding the history of mistreatment. Medical test results Record current and past injuries that are identified during the physical exam. Include x-rays and/or CT scans showing injuries. Note the exact location of each injury in relation to fixed body landmarks. Look for and record specific patterns of injury. Photographs – Photographic documentation is difficult to dismiss and can compensate for the inadequacies of written descriptions and memory. Even if legal action is not anticipated, photographs may be invaluable later. Guidelines include: Photograph injuries after obtaining informed, signed consent. . Photographs should accurately reveal the extent of all injuries. Label each photograph with the name of the patient and the photographer, the patient’s identifying number, and the date. Keep the photographs in a sealed medical record. Body map – A body map can be used as an alternative method for documenting injuries that may not show up well on photographs. Simply identify all injuries, new and old, on the body map. Consent to photograph The undersigned hereby authorizes name of agency And the attending physician to photograph or permit other persons in the employ of this organization to photograph name of patient While under the care of this organization, we agree that the negatives or prints shall be stored in the patient’s medical record (sealed in a separate envelope so that they may be used later for evidence). These photographs will be released only to the police or the prosecutor when the undersigned gives permission to release the medical records. The undersigned does not authorize any other use to be made of these photographs. Date Patient’s Signature Witness Patient’s Parent or Legal Guardian’s Signature Street Address City State Zip Code Adapted from “Responding to Domestic Violence: A Guide for Local Health Departments.” North Carolina State Department of Environment, Health and Natural Resources, May 1996. Discharge planning Consider whether the patient has a safe place to go. If not, help the patient contact family, friends, or a local shelter. If the patient decides to go back into the place where mistreatment happened, help the patient develop a safety plan. Click here for sample plans. Trust the patient’s judgment about the situation. Follow-up with Patients Offer to schedule future visits or times to contact the patient. Make notes about how and when to contact the patient to maintain confidentiality and safety. Staff Training and Education All staff should receive training and education about mistreatment and domestic violence and related policies and procedures specific to their particular healthcare setting and role. Training should occur upon being hired and then appropriate regular intervals thereafter, as well as when job duties are changed or expanded. The breadth and depth of training should be informed by the expected clinical responsibilities and anticipated work setting for each employee and healthcare provider. Clinical staff: Physicians Nurse Practitioners Nurses Physician Assistants Paramedics Lab Technicians Physical Therapists Occupational Therapists Pharmacists Dentists Social Workers Psychologists Training should help providers achieve three goals: Acquire a core body of knowledge on mistreatment and domestic violence. Master the specific clinical skills for identification and intervention. Gain awareness of local community organizations and resources. Non-clinical staff: All staff with direct patient contact should receive training appropriate to their role in the healthcare setting. The context of training should be appropriate to the specific professional or vocational responsibilities of the individual. Training management personnel can be very effective in raising institutional consciousness about domestic violence and gaining the support of those who have influence in policy and decision-making. Other staff: CEOs Clinic Managers Security Administrators Supervisors Risk Managers Employee Assistants Human Resources Staff Training Topic Areas Core knowledge Definitions and prevalence of mistreatment Tactics of abuse, e.g., physical, sexual, emotional/psychological and economic Special populations, e.g., older adults, pregnant women, substance abusers Health-related effects of mistreatment on victims and their families Healthcare providers’ role in addressing mistreatment Legal rights of victims and the legal responsibilities of healthcare providers Personal safety for victims and for healthcare workers Clinical Skills Framing and asking mistreatment screening questions Recognizing signs and symptoms of distress in victims of mistreatment Assessing the patient’s situation by obtaining a history of mistreatment, determining the patient’s immediate risk of danger, and assessing the patient’s mental health needs Providing support in a respectful and non-judgmental manner Documenting properly Developing a safety plan and intervening without placing patients in greater danger Relationships with community organizations Local agencies and organizations that handle mistreatment, domestic violence and sexual assault Example of successful healthcare and community models for addressing partner violence Patient Education: Distribute information widely wherever patients and staff can see it. Distribute information to all patients when screening for mistreatment Provide information in prenatal, childbirth, parenting and health education classes Make information available in waiting areas and exam rooms. Post information in rest rooms – particularly on the door inside the stall Exhibit information on mistreatment at health fairs. Host a resource table during Domestic Violence Awareness Month (October) and participate in the Family Violence Prevention Funds’ Health Cares about Domestic Violence Day. Community Linkages Aim to make the Mistreatment Response Program part of the larger community response to abuse, neglect and domestic violence. Develop a good working relationship with community groups who address these issues. Collaboration is the key to improving the healthcare system and community response to mistreatment and helps deliver the services that are needed with the limited resources available. Creating a healthcare-based Mistreatment Response Program with input from local programs can help build trust and communication. The community response should include community and professional education, advocacy for the responses available, and advocacy for needed policy changes. Effective community education will promote A change in community attitudes about mistreatment Earlier intervention for victims and perpetrators Prevention of future mistreatment Determining Program Success As part of the planning process, establish how the healthcare organization will evaluate the success of the Mistreatment Response Program. This information can be used to validate the value of the program to the patients and to the community and can be helpful in gaining funding outside the healthcare organization. Types of Data to gather Regarding patients and their families (comply with HIPAA rules) The number of patients served Demographic information on patients served The types of mistreatment reported Services delivered Referrals to outside services Evaluation of patients of the Mistreatment Response Program Regarding the staff How many people are trained? What disciplines are involved? How many work hours are used in response to need? Regarding training Who will train the clinical staff? Who will train the non-clinical staff? Who is available to consult on questions not covered in training? How many hours does training take and how frequently is staff trained? Regarding the organization Is there firm support from the administration for the Mistreatment Response Program? Is there staff to help obtain external funding? Regarding community collaboration With which community organizations does the Mistreatment Response Program collaborate? Document the cooperative nature of the relationship. Task Review Policies and Protocols Review Program Documentation Interview Staff Interview Patients Interview staff from Community Agencies Evaluate Training Review Patient Charts Develop Patient Tracking Form Benefits of Task for Determining Program Success Assess program Measure change in Determine patient implementation clinicians’ behavior satisfaction X X X X X X X X X X X X X X X X Chapter 3: Implement IMPLEMENTING THE PROGRAM After a period of planning, the healthcare organization is now ready to start a Mistreatment Response Program. Clinicians, administrators, and staff should remember that implementing the program will take time and issues may arise that have not been addressed. The Multidisciplinary Planning Team needs to meet periodically until the program is functioning well. There are five primary phases to program implementation. 1. Develop a budget and acquire necessary resources 2. Institutionalize routine screening 3. Administer provider training 4. Market the program 5. Determine program success Developing a Budget and Acquiring Resources Programs vary in size, the services they offer and in other characteristics. Their budgets will also vary based on the intervention model chosen, the number of staff hours involved, and the services they provide, as well as other factors. Some funding may come from the healthcare organization itself. Finding additional funds may be the hardest part of starting a program. Each funding agency has funding guidelines, eligibility criteria, funding cycles and submission dates. It will take time and effort to apply for the funding. Possible sources of support Kate B. Reynolds Charitable Trust http://www.kbr.org/html/healthcare/hcdiv.html North Carolina Governor’s Crime Commission http://www.ncgccd.org/Planning/announcement/funding.cfm The Duke Endowment http://www.dukeendowment.org/grants_healthcare.cfm Once funding is secure, the staff who will work on the program needs to be assigned or new staff hired. Look for staff that are interested and have experience working on mistreatment issues, e.g., domestic violence or sexual assault. Determine any additional resources that are necessary, e.g., office space, equipment and supplies. Administering Provider Training Staff training is key to implementing screening and appropriate services. Administrative buy-in should include support for the requirement that staff attend the appropriate training sessions. Staff needs time away from their usual assignments to attend training. Develop a schedule which repeats training at several times. Start with staff that will be most receptive and/or most critical to the success of the program’s screening and service mission. Institutionalizing Routine Screening Protocols and procedures for routine screening need to be implemented for the program to begin. A systematic plan should be developed to set priorities and phase-in the implementation of screening. Consider the flow of patients in the organization and gather input from staff as to how to best institutionalize screening. Marketing the Program Consistent and effective marketing of the Mistreatment Response Program is key during the implementation phase. Promote the program to staff, patients, community agencies and the public. Marketing Checklist Request top management write letters of support for the program to providers. Meet with clinic managers to discuss training and protocol development. Present information about the program at staff meetings. Post program information in staff and patient restrooms, lounges, and snack bars. Place flyers about the program in all staff mailboxes or pay stubs. Email information to those who are connected electronically. Promote the program to various community agencies that serve mistreated people. Market the program through local news releases and letters to the newspaper editor. Determining Program Success Proof of the program’s effectiveness may be needed for continued funding and community support. In addition, healthcare providers will likely desire evidence that the intervention helps before they are willing to incorporate it into their practice. The planning team should not be afraid to change components that aren’t working. Questions that can assess the overall program include: Is the program being implemented as planned? If not, why not? Are the clinicians doing what was planned? If not, why not? If not, what changes can be made to improve the clinical response? What are the benefits to the patients from the program? Are changes needed? Try to identify potential problems as soon as possible so that they can be addressed and rectified. Additional questions regarding program quality and effectiveness are: What differences are there in program implementation across the healthcare organization? Which aspects of the program are implemented? Which are not? Are certain departments or staff members unable or unwilling to participate fully in the program? If so, what can be done to change this? Data about program success can be found by: Reviewing program documentation, e.g., patient use records, staff attendance at training records, written materials about the program. Interview staff to determine if the program is being accomplished. Identify whether or not policies and protocols have been developed and implemented. Observe training sessions and obtain feedback regarding training relevance and effectiveness. Interview patients to determine if they were asked about mistreatment and if they were offered services if they indicated they were mistreated. Review patient charts for documentation.