Things That Bring Me In At Night (Vascular Emergencies)
advertisement

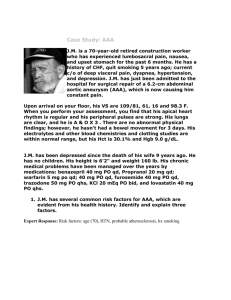
Things That Bring Me In At Night (Vascular Emergencies) Abdominal Pain 69 year old male Sudden onset abdominal pain, passed out at work PMH: HTN PSH: Hartman’s procedure for diverticulitis Meds: None SH: Retired, plays golf daily PE: BP 65/40, HR 120 Lungs: Coarse Heart: Tachy Abd: Hugely distended, midline scar Ext: Weak pulses Referred from outside hospital, 45 minutes in ambulance AAA Prevalence 2-5 % Men 4:1 Rupture Risk Size does matter • • • • 5-5.9 cm 5% per year 6-7 cm 6.6% per year > 7cm 20% per year Grow at 0.5 cm/year Etiology of Ruptures Aortic wall contains vascular smooth muscle as well as elastin and collagen Gradual reduction of medial elastin layers and collagen content • Medial thinning and intimal thickening Elastin is principal load-bearing element that resists aneurysm formation Collagen acts as “safety net” to prevent rupture Excessive collagenase activity/ elastase activity Laminated thrombus lines aneurysm Law of Laplace Relationship between tangential stress (T) tending to disrupt the wall and radius ( R) and the transmural pressure (P) T=P*R Diagnosis High index of suspicion is critical < 15% know they have AAA prior to rupture Mean time from Sx to ER is 37 hrs Lower back, flank or groin pain Pulsatile abd mass, hypotension, anemia No imaging in an unstable pt Treatment 60 % of ruptures die prior to arrival 48 % operative mortality Overall ~ 90% mortality for ruptures Take promptly to OR “I feel no significant attempt should be made for blood volume resuscitation until the time of operation. The SBP should be maintained 50-70 mm Hg until the aorta is clamped.” Prepped/draped then anesthesia Bulging Groin 79 year old male History of bulge right groin, recent difficulty walking, no recent trauma Poor historian PMH: COPD, HTN PSH: No vascular surgeries Meds: Inhaler FH: No aneurysms PE: Thin black male 148/87 No acute distress RRR CTA Pulsatile mass right groin Cool lower extremities, no palpable pulses Embolization L hypogastric 12/20 EVAR of L Iliac aneurysm 12/22 R femoral aneurysm repair 12/31 Bilateral AKAs 2/19 Returns 7/04 with enlarging pulsatile mass in left groin Head Aneurysms AAA identified in 6-9% of men over 65 Family history discernible in up to 20% Specific genetic defects only identified in 5% of familial AAA Pathology of aneurysm wall: Decreased elastin (especially in Marfan’s) Altered type III collagen (Ehlors-Danlos) Endogenous proteases produced by inflammatory cells Matrix metalloproteinases (esp. MMP-9 and MMP-12) • Activity reduced by doxycycline with decreased aneurysm formation in rat models Alpha-1 anti-trypsin association in familial AAA Lipoprotein (a) increased levels in familial AAA Aneurysms Isolated iliac/femoral artery aneurysms rare Usually associated with aortic aneurysms Both more common in men For iliac, incidence is 1% that of AAA (500/year US) Common > Internal > External Natural history not well known, although rupture rare if <3 cm Rupture more common than embolus or thrombosis, especially if greater than 5 cm Treatment must consider likelihood of AAA development in the future Aneurysms Femoral Type 1 CFA only, Type 2 involves origin of profunda Rare, seen in only 3% of AAA Of pts with CFA aneurysm • 95% have second aneurysm • 92% had aortoiliac aneurysm • 59% bilateral femoral aneurysm -Dent et al. Arch Surgery, 1972 Natural history also not well known Thrombosis more common than rupture, 12-40% estimated GSW Left shoulder 37 year old female GSW to left shoulder Hemodynamically stable Previous GSW abdomen BP 150/70 R, 70/30 L Left hand cool Etiology Emboli vs Thrombosis Emboli primarily from the heart (AAA’s) Thromboses occur most freq in setting of aortoiliac occlusive dz • Low flow states (dehydration / decreased CO) Intraplaque hemorrhage Hypercoaguable states Dissection / Trauma Diagnosis Six p’s of acute extremity ischemia Severity dependent on extent of thrombus, distal embolization, adequate collaterals Focus on neuro deficits often cause delay Presence of abd pain, severe HTN, anuria suggest renal and mesenteric involvement Utility of imaging is uncertain • Dossa: helpful in 2/24 • Littooy: helpful in 1/6 Treatment Requires prompt definitive treatment • Severity of ischemia correlates with outcome more than duration Several case reports of endovascular tx • Reserve for high-risk, minimal sx Nonoperative Tx carries > 80% mortality Heparin at time of Dx (except with HAT) Measure bilateral upper extremity BP’s Treatment Thromboembolectomy • All pts should undergo initially unless severe aortoiliac dz is known Axillobifem • “Simple” with potential lower mortality • Inferior long term patency (5 yr 37-81%) vs (8090%) • Potential for clot propagation Summary Outcome Mortality 23-53% High Complication rate (70%) Limb salvage approaches 95% in surviviors Pts with embolic occlusions noted to have 27%-37% recurrent emboli – underscores need for long term anticoagulation 52 yo AA male c/o left foot rest pain PMHX: pancreatitis, arterial occlusive disease PSHx: Bilat iliac stents, Left CFA endarterectomy, L SFA stent Meds: tylenol, coumadin Social: Heavy tobacco history Exam: Alert, responsive No JVD, no bruits RRR, no murmurs Abd soft, no masses Palpable femoral pulses Palpable distal pulses on right Non palpable distal pulses on the left Acute Arterial Occlusion Sx depend on level/severity of obstruction and existence of collaterals Pts without hx of claudication or previous reconstructions – most likely embolic 6 “P”s Ischemic manifestations usually most severe one joint space distal to occlusion Pain – sensory deficits – numbness – paralysis Pallor – blanching mottling – nonblanching mottling Management Embolism: Thromboembolectomy Pts with preexisting vascular disease are much more complicated Heparinization Arteriography when cause is uncertain Emboli: Meniscus sign, lodge in bifurcations, multiple filling defects Doppler exam: help determine patent distal outflow tract Bypass Fasciotomy Capillary leak after prolonged ischemia and reperfusion As compartment pressure rises, tissue perfusion decreases Inflammatory mediators and free radicals Neutrophil adherence to endothelium leads to oxidant release 20 mmHg: impaired < 30 mmHg from DBP, flow is sig decreased Need for fasciotomy increases with > 6 hours Arterial and Venous injury Soft tissue crush injury or Fx Fibinolytic agents Streptokinase Combines with plasminogen to form activator complex which acts within the clot and in circulating plasma Urokinase Directly converts pasminogen to plasmin Higher affinity for clot bound plasminogen tPA – even greater clot specificity Case Presentation 65 yo male with acute slurred speech and loss of vision in the inferior field of the R eye PMH: B carotid stenoses on recent US, HTN, CHF, hypercholesterolemia PSH: appendectomy Social: quit smoking 1973 Meds: plavix, norvasc, lisinopril, simvastatin Case Presentation Exam: B carotid bruits (L>R), heart regular, visual deficit inferior hemifield of R eye, normal speech, no focal weakness EKG: sinus rhythm Echo: no thrombus or vegetation Head CT (admission): negative MRI (day 2): multiple infarcts involving R frontal lobe, L caudate nucleus, and L occipital lobe Amaurosis Fugax R superior retinal infarct Ophthalmic artery (1st branch of ICA) Retinal arteries Visual Deficit R inferior hemifield deficit R superior retinal infarct Carotid Duplex Class 1 2 3 4 5 Category 0-39% 40-59% 60% 60-99% occluded Vp (cm/s) <160 >160 >160 >160 0 Vd <80 <80 80-109 >110 0 R Carotid Duplex Class 3 L Carotid Duplex Class 4 Arch vessels R carotid arteries R carotid arteries L carotid arteries Controversies in Carotid Surgery General anesthesia vs. local anesthesia Intraoperative monitoring of cerebral ischemia Selective shunting vs. routine shunting Primary closure vs. patch angioplasty Carotid Endarterectomy with Intraluminal Shunt Complications of Internal Shunts 1-3% complication rate Damage to the arterial wall Embolization Arterial Closure Following Shunt Placement Measurement of ICA Stump Pressure PICA ~ PMCA Local Anesthesia with Mental Status Monitoring “The time-honored technique is trial occlusion with local anesthesia.” (Rutherford Vascular Surgery) Considered the gold standard Carotid occlusion for 3 minutes with evaluation of speech and contralateral movement 85-90% pass this test, but 10-15% require a shunt This technique yields the lowest stroke rate and lowest rate of shunt use Common Indications for Shunt Placement 1. 2. 3. 4. 5. Deterioration of mental status exam or contralateral extremity function EEG changes ICA stump pressure <40 (range 25-50) Recent stroke Complete occlusion of contralateral ICA