Infertility UNC School of Medicine Obstetrics and Gynecology Clerkship Case Based Seminar Series
advertisement

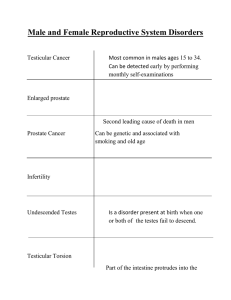
Infertility UNC School of Medicine Obstetrics and Gynecology Clerkship Case Based Seminar Series Objectives for Infertility Define infertility Describe the causes of male and female infertility Describe the evaluation and initial management of an infertile couple List the psychosocial issues associated with infertility Definition Failure of a couple to conceive after 1 year of regular intercourse without use of contraception Primary infertility – No prior pregnancies Secondary infertility – Prior pregnancy Prevalence Infertility affects 10-15% of reproductive-age couples in the U.S. Approx. 85% of couples achieve pregnancy within 1 year Conception rate (fecundability) 25% conceive within 1 mo. 60% conceive within 6 mo.’s 75% conceive within 9 mo.’s 90% conceive within 18 mo.’s Etiology Successful conception requires a specific series of events: 1. 2. 3. 4. 5. 6. 7. Ovulation of competent oocyte Production of competent sperm Juxtaposition of sperm and oocyte in a patent reproductive tract Fertilization Generation of a viable embryo Transport of the embryo to the uterine cavity Implantation of the embryo into the endometrium Etiology Major causes of of infertility: Female factor – 60% Ovulatory dysfunction Abnormalities of female reproductive tract Peritoneal factors Reproductive aging Male factor – 20% Abnormal semen quality Abnormalities of male reproductive tract Idiopathic – 15% Infertility in ~ 20-40% of couples has multiple causes Infertility: History Female Duration of infertility and prior evaluation or therapy Menstrual cycle (length and characteristics) Symptoms associated with ovulation (e.g. breast tenderness, bloating, mood changes) Full OBHx and GynHx Prior pregnancies, surgeries, or STD’s Sexual history (frequency of intercourse) Chronic medical illness Family history (infertility, birth defects, genetic disorders) Social history (smoking, EtOH, drugs) Infertility: History Male Prior children Genital tract infections Genital surgery or trauma Chronic medical illness Medications (e.g. Furantoins, CCB) EtOH, drugs, or smoking Sexual history (frequency of intercourse) Infertility: Physical Exam Female Height, weight , BMI Pelvic exam Masses Tenderness (Adnexa, Cul-de-sac) Structural abnormalities (Vagina, Cervix, or Uterus) Male (Urologist referral) Evidence of androgen deficiency Structural defects (e.g. varicocele, hernia) Male factor: Evaluation Male Factor Initial evaluation Further evaluation Semen analysis Urologic evaluation FSH, LH, and testosterone level Genetic evaluation Epididymal sperm aspiration (PESA, MESA) Testicular biopsy Male factor: Evaluation Semen analysis Following 2-4 day period of abstinence Repeated x1 for accuracy Element Reference value Ejaculate volume 1.5-5.0 mL pH > 7.2 Sperm concentration > 20 million/mL Motility > 50% Morphology > 30% normal forms Male factor: Evaluation Urologic evaluation Physical Exam Varicocele Congenital absence of vas deferens (CAVD) Transrectal ultrasound Vasography, Seminal vesiculography Epididymal sperm aspiration (PESA or MESA) Male factor: Evaluation Endocrine evaluation Indication: Oligospermia (< 10million/mL) or sexual dysfunction (decreased libido, impotence) FSH, LH, testosterone Genetic evaluation Indication: Azoospermia (no sperm) CFTR mutation Karyotype (Klinefelter’s, Y chromosome deletion) Testicular biopsy Indication: Nonobstructive azoospermia Palpable vasa Normal testis volume Normal FSH/LH Female factor: Evaluation Factor Initial evaluation Further evaluation Ovulation History and physical exam Basal body temp charting Ovulation predictor kit Mid-luteal phase progesterone level Endocrine testing Endometrial biopsy Reproductive tract (uterus or fallopian tubes) Hysterosalpingogram (HSG) Ultrasound Saline-infusion sonography Hysteroscopy Laparoscopy Peritoneal Laparoscopy Reproductive aging FSH, estradiol, or AMH Female factor: Menstrual Cycle Female factor: Evaluation Ovulation Initial evaluation: Basal body temp – rise for > 10 days indicates ovulation Ovulation predictor kit – detects LH surge in urine Further evaluation: Mid-luteal phase progesterone level - level > 3 ng/mL provides qualitative evidence of recent ovulation Endocrine testing (TSH, prolactin, FSH, LH, Estradiol, DHEA-S) Endometrial biopsy Not routinely performed Female factor: Evaluation Reproductive tract Initial evaluation: Hysterosalpingogram (HSG) Detect uterine anomalies (septate or bicornuate uterus, uterine adhesions, uterine leiomyoma) Detect patency of fallopian tubes (occlusion, hydrosalpinx, salpingitis) Ultrasound – alternative to HSG to evaluate uterus Female factor: Evaluation Reproductive tract Further evaluation: Saline-infusion sonography (SIS) Hysteroscopy Laparoscopic chromotubation Female factor: Evaluation Peritoneal factors Laparoscopy Endometriosis Pelvic/adnexal adhesions Female factor: Evaluation Reproductive aging Indications: > 35 years of age 1st degree relative with early menopause Previous ovarian insult (surgery, chemotherapy, radiation) Smoking Poor response to ovarian stimulation Unexplained infertility Candidate for IVF Female factor: Evaluation Reproductive aging Cycle day 3 serum FSH and estradiol Abnormal (“diminished ovarian reserve”) FSH > 10 IU/L Estradiol > 75-80 pg/mL Clomiphene citrate challenge test Cycle day 10 serum FSH Serum antimullerian hormone (AMH) Idiopathic Infertility Prevalence ~ 15% Factors that cannot be identified Sperm transport defects Inability of sperm to fertilize egg Implantation defects Infertility: Management Male Factor Avoidance of alcohol Scheduled intercourse Ligation of venous plexus for significant varicocele Intrauterine insemination (IUI) with washed sperm Intracytoplasmic sperm injection (ICSI) + IVF Donor sperm insemination Infertility: Management Anovulation Oral medications: Clomiphene citrate Dopamine agonists (Bromocriptine) - hyperprolactinemia Injectable medications: Gonadotropins (FSH/hMG, hCG) Laparoscopic “ovarian drilling” Complications: Ovarian hyperstimulation, Multiple pregnancy Infertility: Management Reproductive tract abnormality Uterine: Myomectomy, Septoplasty, Adhesiolysis Tubal: Microsurgical tuboplasty, Neosalpigostomy Peritoneal: Laparascopic treatment of endometriosis, Adhesiolysis Idiopathic infertility Ovarian stimulation + IUI Clomiphene or gonadotropins (hMG, hCG) IVF Infertility: Management (IVF) Used for: Severe male factor Tubal disease Couples who failed other treatments Requires Controlled ovarian hyperstimulation Retrieval of oocytes In vitro fertilization and embryo transfer Procedures IVF + embryo transfer (IVF-ET) Intracytoplasmic sperm injection + embryo transfer (ICSI-ET) Donor egg IVF + embryo transfer Psychological The psychological stress associated with infertility must be recognized and patients should be counseled appropriately. Bottom Line Concepts Infertility is defined as one year of unprotected coitus without conception. Infertility may be primary or secondary. Multiple causes must be considered for infertility diagnosis and treatment. Male and female reproductive tract anatomy and physiology should be reviewed in order to generate a full differential diagnosis. Components of an initial infertility workup include a thorough history and physical examination. Laboratory investigations include a semen analysis, documentation of ovulation, and hysterosalpingogram. Dysfunction of the hypothalamic-pituitary-ovarian (HPO) axis and medical illness, including thyroid disease and pituitary tumors, can cause ovulatory disturbances. Success rates with IVF depend on the etiology of infertility and the age of the female partner. References and Resources APGO Medical Student Educational Objectives, 9th edition, (2009), Educational Topic 48 (p102-103). Beckman & Ling: Obstetrics and Gynecology, 6th edition, (2010), Charles RB Beckmann, Frank W Ling, Barabara M Barzansky, William NP Herbert, Douglas W Laube, Roger P Smith. Chapter 38 (p337-346). Hacker & Moore: Hacker and Moore's Essentials of Obstetrics and Gynecology, 5th edition (2009), Neville F Hacker, Joseph C Gambone, Calvin J Hobel. Chapter 34 (p371-378).