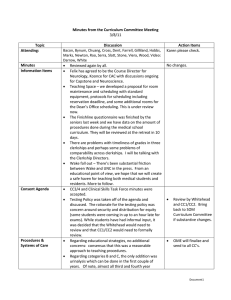
Minutes from the Curriculum Committee Meeting Topic Discussion Action Items
advertisement

Minutes from the Curriculum Committee Meeting 9/3/10 Topic Attending: Annual Review of Outcomes Discussion Bacon, Byerley, Chuang, Cross, Dent, Dreesen, Enarson, , Farrell, Fields, Gilliland, Perry, Rao, Slatt, Steiner, Stone Viera, Guest: Wurzelmann (Dan – MSIII); Not There: Bankaitis, Bynum, Clarke-Pearson, Felix, Heck, Johnson, Shaheen, White Powerpoint is attached, we welcome additional comments. Action Items Comments: o o o o o o Where are we and what are the big lessons? Diversity remains a major commitment, as underscored by the replacement of Larry Keith. In particular, we may need to focus on Hispanic and possibly rural/low SES students. We need to pay attention to struggling students. This is both a mechanism – how to track people with comments below the Dean’s lines - but also making sure that people who can be doctors are doctors. Balance of workforce – we need to have an appropriate balance. Of note, Erin Fraher will be focusing on that as we move forward in the future. What we are missing is an evaluation at the end that our doctors are ready to go on to residency pulling it all together. This is akin to what residency directors do at the end of residency but it’s got to be one person who knows the patient being able to say that. Do we really know how well people practice at the end? We’ve got OSCEs but not an integrated whole. Furthermore, most of the faculty in Document1 How can the UNC mission guide our assessment of outcomes? the third year don’t know them well enough to be able to say – here is one of the places where the Asheville project can guide the way for us. o How well are we doing in terms of keeping people in the state? Do we prefer people coming in? Do they attract and stay here – analogous to the residencies? What other data do we need to look at? o Both residency director and former medical student self assessment at a year out, and possibly later than that. o Long-term outcomes of the MD-MPH program and the MD-PhD program. They are both prominent and important. How can we know whether or not they’ve made a difference? o What schools are we bringing people from? This is important to our discussion of keeping people within the state. o Better knowledge of specialty by specialty outcomes. We need better graphs but also information across that board. We are above average in Ob/Gyn and Pediatrics. Where are we below average - ? Surgery, ? Medicine. o We need to have a sense of how many are solid clinicians at the end. o National practitioner database – can we get that information as a sign of professionalism? o Can we track balance of specialty, not just particular specialties? Alan Cross participated in the process. Comments included: o o o Should there be a fourth category of service? Should education come before patient care? A lot of emphasis on education and research and not as much on other aspects of education. Document1 o Competency Milestones We need to think about metrics and the current mission. o To create a community of educators would be attractive. o Emphasize our diverse students and products. General issues that were addressed: Ongoing Program and Curriculum Management All send specific comments to Warren, Lisa and Cam. How well do we know that fourth years are competent? We need to make sure that some of our competencies are not actually too elevated for medical students- more appropriate for residents or fellows. Syncing competencies so that they are all at the same time in the first year is important – this is particularly important since we’ve made a decision to push more clinical care into the first year. We need to come to agreement about elements that can be in more than one place – there’s some knowledge that can be both in medical knowledge as well as others, although we have to be very careful about the message that we transmit or items that could be population health or other elements. Reviewed above and overall process affirmed with additional data and time for discussion. Overall management of the curriculum – Newton presented the framework in the memo and there was commentary. Major comments included: o In the clinical years, evaluations can be tracked to the competencies and then rolled up. This should be a major way of tracking how well we’re doing, both for individual patients as well as for the curriculum. We discussed the need for formal assessment at the end of the third and fourth year with people who know the students. Should we do this earlier in the curriculum also? o Clinical evaluations need to be integrated across the four years so that they are coherent and Document1 sequential. GQ feedback can go into course reviews as well as reviews of student programs. Clinical Log – Newton presented the principles from the subcommittees. Please note that the Appendix sent out with the minutes was not the right Appendices. What we have in mind, was a sample of what the competency committee developed as an Appendix. Additional comments: We need to be careful about complexity of the list which is important. It needs to be user-friendly. We have experience with this in Asheville. The balance will be challenging. On the one hand, clearly the conditions should be ones in which we should be embarrassed if the students did not see, but on the other hand, we can be aspirational. We need to be thoughtful about the procedures. The epidemiology of experience of procedures has changed dramatically as Interventional Radiologists have begun to get involved. Many residents don’t get enough exposure at this stage much less students. We need to have a focused attention as to what we want them to have and then seek that out. Should we begin to think about following up with students systematically after 12-24 weeks into 3rd? This might require calendar changes. The assumption is that this will be used also in the mid-clerkship assessment and remediation taken care of. The next draft of the tracking document will emphasize changes in evaluations and clinical log, as discussed, as well as filling out specific sources of data. Key decisions regarding the log: o Technically user friendly o Both diseases/conditions and symptoms o Over all four years o The list of core diseases will be dealt with repetitively over that period of time but it’s expected that other noncore diseases will be brought up as necessary. o Rule for diseases and NC prevalence, morbidity & mortality, cost of care for both conditions as well as preventive conditions o Consensus that students must drive the process and advisors work with the students on that. We need to build that in. The next step will be to come up with a list of core diseases for input by the Curriculum Committee. Newton will follow-up and get input from the subcommittee. Document1