Minutes from the Curriculum Committee Meeting Topic Discussion Action Items
advertisement

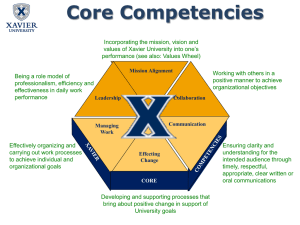
Minutes from the Curriculum Committee Meeting 5/4/11 Topic Attending: Minutes Information Items Discussion Bacon, Byerley, Chuang, Darrow, Dent, Dreesen, Enarson, Farrell, Felix, Heck, Hines, Hobbs, Jordan, Perry, Rao, Serra, Shaheen, Slatt, Steiner, Stone, Woods Approved unanimously. New Whitehead Co-Presidents were introduced (Rachel Hines and Meg Jordan) Cedric Bright, MD will start as Director of the Office of Special Programs and Assistant Dean of Admissions 7/1/11. He came to the SNMA graduation celebration and the students are excited to have him. He is the incoming president of the National Medical Association. Strategic planning at the School of Medicine is underway. Some of you may have received the survey. This is important because it will determine the broad scope of our education mission over the next number of years. Importantly, the research done for the review has identified that benchmark institutions have done competencies a while ago and are proceeding towards team based learning and often longitudinal curriculum. Budget & tuition increase news – in process. The House budget has 17.5% cut, which is an improvement over the first budget. The House budget will be finalized in the next week or so and then it moves to the Senate and the Governor. Liz Dreesen has agreed to become co-director of CC1. Jonathan Oberlander has agreed to become course director of the Humanities and Social Sciences seminars. Anthony Charles will be the director of the Surgery clerkship. Tim Farrell will serve as co-director of that clerkship and retain his leadership role in CC3/4. Jim Barrick has agreed to be the course director for Introduction to Acute Care. Campus visits will focus on LCME issues – what the campus leadership and faculty need to know. We have started a significant intervention with Pharmacology and then perhaps also Cardiovascular. Timeliness of Grades – We’ve had significant improvement in the timeliness of grades but inpatient medicine and electives are still a problem. ? Berryhill vs. Taylor Hall – We are now in the process of negotiating with campus for which one we should Action Items Document1 Consent Agenda support. The possibility has risen of renovating Taylor Hall in the way that we did Burnett-Womack. We decided that the new medical education building will not have another lecture hall and that we will likely not use Brinkhous-Bullitt for Anatomy. We will embed Anatomy facilities in the new facility. Comments on Course Reviews: Please note that integration selective will be changing its name to “The Science of Medicine” starting with the new year. Gastroenterology has demonstrated a best practice. Their exam quality has improved substantially as a result of efforts of the course director, Ryan Madanick, to implement what he learned from AOE workshops, faculty presentations, and support from Mari-Wells Hedgpeth. Host Defense and Microbial Pathogens (MS1) has piloted mid-course feedback across competencies. Comments Regarding Midcourse Review: Professionalism How should clerkships include in clinical settingsformative vs. summative? Discussion included importance of being explicit about what would happen. Clinical settings are often formative with the exception of exams if previously labeled such. What’s innovative about what Kurt described is feedback across the competencies. There needs to be some faculty development in giving feedback across competencies regarding pilot of midcourse review. The rest of the consent agenda items were accepted. The Professionalism Task Force included representatives from ICM, students, advisors and Social Medicine. Draft minutes are available in the agenda. The group reviewed the Cruess visits and the learnings from their visit and then put together the components of what we might want to do with respect to teaching professionalism – the chart is a draft . The focus of the discussion was on priorities for next year. The recommendations were: 1. Orientation should include an explicit mention of social contract as well as introduce the language/concepts by Advisor. Priorities for 2011-2012: Orientation to include social contract and introduction to core concepts in Advisory Colleges. Track where taught explicitly. Pilot peer evaluation. Capstone Faculty development OME will work with faculty leaders to develop Document1 2. A next step should be defining where topics are taught, specifically what’s done within Medicine & Society vs. other settings. 3. Pilot and spread peer evaluations in the next year. 4. Embed professionalism in the student clerkship evaluations. 5. Include professionalism in Capstone. 6. Faculty development around professionalism. explicit plan and bring it back to SOM Curriculum Committee. Comments: We need to include guidance on appropriate use of Facebook and other social media. Dr. Pamela Rowland of Surgery has done a lot of work on communication and professionalism; it might be appropriate to incorporate her in the group. How to do faculty development is critical – the next phase of the discussion should include that. One approach would be to work with the institutional leadership to establish definitions of professionalism and other common terms. Perhaps the Academy of Educators can invite another guest speaker on professionalism. Population Health The Curriculum Committee endorsed these principles for next steps. A task force with slightly different composition will meet to flesh out where professionalism is addressed in the curriculum - a definition and strategy for faculty development in the next year. Please see draft minutes from the Population Health Task Force. The major focus of the group was to explore what we’re currently doing and to see whether we should add focused material in the first year. Members of the task force included course directors from Medicine & Society and Clinical Epidemiology with previous input from CSD/CSI and the MD-MPH leaders. The task force began by describing what is currently taught. Medicine & Society includes a lot of theoretical framework for looking at populations as well as some of the organization of care. Clin. Epi. takes the tools of population science and focuses on those things relevant to the care of individual patients – diagnostic assessments as well as critically appraising the literature. Indeed, explicitly, clinical epidemiology took out some of the population management issues several years ago. Also of note, for the last three years the students OME will work with faculty leaders to track what and where population health is delivered through the curriculum and define options for how it might be integrated in the first year. Document1 have said that they want to put Clin Epi into the first year. The consensus of the task force was that there was indeed new material and that it should probably go in the first year whether it be part of Medicine & Society or a new course itself, provided that the details could be worked out. In addition, the committee considered the question of whether there should be a block or a distributed longitudinal base. The sense of the group was that there should be both going forward. Finally, they commented that there was much less population health involvement in clerkships than there might be. The students commented that it was hit and miss. The task force will address. Comments: The overall goal of improving the population health curriculum is to give a perspective not just of patients one by one but of managing a population. This will need a gradual approach to place through the curriculum. It includes, but is not limited to, burden of suffering in the second year. It needs some actual exercises. Basic metrics such as quality and costs need to be presented in the first two years so they can be followed up in the third and fourth years. Putting more critical appraisal in the first year may be helpful for summer research projects. A key issue is where Host Defense goes. There are also many things in Host Defense that could help with the content of population management. The task force envisioned what the key elements are in learning how to manage a population. They believe that it naturally occurs as an extension from managing individual patients. So, they start with individual patients, take collections of patients (from a group practice), then extend to those who don’t come in, with explicit attention to both subspecialty and primary care examples. The community weeks play an important role, and exercises can be added to them to underscore management of populations. As with professionalism, we are evolving a framework in which each of the competencies is tracked and managed through the curriculum. Document1 Integrated Fridays Simulations might be possible, but we need to think more deeply about assessment. Context – The Curriculum Committee decided that ultimately they want to combine normal and abnormal science throughout the curriculum. Several have had the idea of trying to integrate them in a particular day – for example, starting with a case presentation and a symptom, then the normal anatomy and physiology and then pathophysiology and diagnosis all grounded in the clinical assessment. GI, Musculoskeletal and ICM are interested in doing this. The discussion here was whether and when we should pilot. Discussion: The Framework for the Next Two Months There was concern that we needed a more developed vision of where the curriculum is going, particularly in view of the calendaring. We need the overall vision and need to fit this into it. Otherwise, it’s just piecemeal. The counterpoint is that we have milestones and established strategies, and we need to learn how to implement them, since it is not trivial. We need to proceed to start to do that – such integrated days would allow us the opportunity to begin to learn . SHAC and foreign experiences can be helpful – they reveal a lot about management of populations in addition to systems based practice. Can students be given a Chinese menu style approach? Role modeling is critical, so we need to have a way of explicitly identifying faculty who are managing populations. We need to have a strategy for dealing with variation of knowledge among faculty about management of populations. Again, this is something that the Academy of Educators might address. We’ve reached the stage where work along a number of different lines is going to be integrated. 15 months ago we started to define competencies then milestones and now integrate them into each of the courses. This is the major task of the next 2-3 months. At the same time, we’ve got a number of cross cutting initiatives that we as the leadership group have Document1 defined – curricula on professionalism, population health, high salience LCME issues that will need to be acknowledged and built into the curriculum. Our review has also determined that we need a broader set of assessment tools. We need to identify what we are doing already, and we need to have a strategy for moving forward with assessment. Alice Chuang and her task force are leading this process. In June, the end of year reviews in each of the year curriculum committees will give us a chance for each the years as a group to decide where they are and where they need to go. I don’t anticipate that all of the work with integrating the new components of assessment will be done by that time but we should have the objectives mostly in place by then. The SOM Curriculum Committee retreat will take place at the end of June and will again address how the whole Curriculum Committee will begin to ensure that the various threads are woven together. As I think we all recognize, pulling everything together is a challenging task. As Nick Shaheen noted, it is important to give our course directors and clerkships prioritization – things that they need to be working on and help them as much as we can. The first task is to evaluate the competencies and milestones in the courses/clerkships. Curriculum Committee Meetings (monthly) in 238 MacNider: 6/6 – 5:30-7pm (NOTE: CHANGED TO 5-6:30PM) 7/11 – 5-6:30pm 8/18 – 5-6:30pm 9/19 – 5-6:30pm 10/17 – 5-6:30pm 11/14 – 5-6:30pm 12/15 – 5-6:30pm Document1