SAN DIEGO STATE UNIVERSITY ENVIRONMENTAL HEALTH & SAFETY BLOODBORNE PATHOGEN EXPOSURE
advertisement

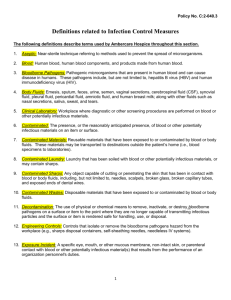
SAN DIEGO STATE UNIVERSITY ENVIRONMENTAL HEALTH & SAFETY BLOODBORNE PATHOGEN EXPOSURE CONTROL PLAN FOR RESEARCH AND HEALTHCARE A. INTRODUCTION AND OVERVIEW The U.S. Department of Labor Occupational Safety and Health Administration (OSHA) Bloodborne Pathogen Standard effective 6 March 1992, applies to all employees who could "reasonably anticipate," as the result of performing their job tasks, contact with blood and other potentially infectious materials (OPIM). ). OSHA'S bloodborne pathogens standard (8 CFR 5193) protects employees who work in occupations where they are at risk of exposure to blood or other potentially infectious materials. San Diego State University’s Bloodborne Pathogen Exposure Control Plan can be found at the Environmental Health & Safety website http://bfa.sdsu.edu/ehs/. "Blood" means human blood, human blood components and products made from human blood. "Other Potentially Infectious Materials" means the following human body fluids: semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures, and any body fluid visibly contaminated with blood and all undifferentiated body fluids in emergency response situations. OPIM also include: Any unfixed tissue or organ other than intact skin from a human (living or dead). Cell, tissue or organ cultures from human or experimental animals infected with HIV, HBV or HCV. Blood, organs or other tissues from experimental animals infected with HIV, HBV or HCV. Culture medium or other solutions containing HIV, HBV or HCV. The purpose of the Standard is to limit occupational exposure to blood and other potentially infectious materials since any exposure could result in transmission of bloodborne pathogens that could lead to disease or death. These pathogens include hepatitis B virus (HBV) and human immunodeficiency virus (HIV), syphilis, malaria and many others. The primary feature of this standard is a written Exposure Control Plan; at SDSU it is called the Bloodborne Pathogen Exposure Control Plan. Individual Research Laboratories and Healthcare Settings shall develop and implement a Department Specific Exposure Control Plan. The Department ECP Template can be found at http://bfa.sdsu.edu/ehs/ . B. POLICY At SDSU, the California OSHA Bloodborne Pathogen Standard (8 CCR 5193), http://www.dir.ca.gov/title8/5193.html, takes precedence over the Federal OSHA Bloodborne Pathogen Standard (29CFR 1910.1030), http://www.oshaslc.gov/OshStd_data/1910_1030.html. San Diego State University is committed to providing a safe and healthful work environment for our entire staff. In pursuit of this goal, the following exposure control plan (ECP) is provided to eliminate or minimize occupational exposure to bloodborne pathogens in accordance with CalOSHA standard 8 CFR 5193, "Occupational Exposure to Bloodborne Pathogens." The ECP is a key document to assist our organization in implementing and ensuring compliance with the standard, thereby protecting our employees. This ECP includes: Determination of employee exposure Implementation of various methods of exposure control, including: Universal precautions Engineering and work practice controls Personal protective equipment Housekeeping Hepatitis B vaccination Post-exposure evaluation and follow-up Communication of hazards to employees and training Recordkeeping Procedures for evaluating circumstances surrounding exposure incidents Sharps Injury Log Implementation methods for these elements of the standard are discussed in the subsequent pages of this ECP. C. RESPONSIBILITIES 1. EHS is responsible for: 1. Developing and implementing the elements of the SDSU Exposure Control Plan (ECP). 2. Maintain, review and update the SDSU ECP at least annually and whenever necessary to include regulatory updates and to reflect new or revised employee categories with occupation exposure to bloodborne pathogens. 3. Determining the level of potential exposure to bloodborne pathogens for specific categories of employees. 4. Providing guidance to supervisors regarding universal precautions related to bloodborne pathogen control. 5. Ensuring that all medical actions required by the standard are performed and that appropriate employee health and OSHA records are maintained. 6. Providing training, documenting training and making the written SDSU ECP available to employees and OSHA representatives. 2. Individual supervisors/principal investigators are responsible for: 1. Adopting applicable elements of the campus Exposure Control Plan to develop site-specific Exposure Control Plan 2. Implement elements of the site-specific Exposure Control Plan. 3. Providing and maintaining all necessary PPE, engineering controls, labels, and red bags as required by the standard. 4. Ensuring that adequate supplies of the aforementioned PPE are available in the appropriate sizes. 3. Individual employees are responsible for: 1. Reading and being familiar with applicable elements of the Exposure Control Plan. 2. Complying to the procedures and work practices outlined in the Exposure Control Plan. 3. Reporting any injury or incident to their supervisor or EHS. 4. Attending the Bloodborne Pathogen Training Sessions. D. EXPOSURE CONTROL PLAN COMPONENTS The Exposure Control Plan shall contain at least the following elements: Exposure Determination Method of Compliance o Universal precautions o Engineering and work practice controls o Personal protective equipment o Housekeeping HIV, HBV and HCV Research Laboratories Hepatitis B Vaccination and Post-Exposure Evaluation and Follow-Up Hazard Communication Recordkeeping Evaluation of Exposure Incidents Sharps Injury Log Employees covered by the bloodborne pathogens standard receive an explanation of this ECP during their initial training session. It will also be reviewed in their annual refresher training. All employees can review this plan at any time during their work shifts by contacting EH&S (619) 594-6778 or the employee’s Supervisor. If requested, we will provide an employee with a copy of the ECP free of charge and within 15 days of the request. Use the CalOSHA Exposure Control Plan for Bloodborne Pathogens booklet as a workbook to aid in the development of the Departmental Exposure Control Plan. This plan includes all elements required by the CalOSHA bloodborne pathogens standard (8 CFR 5193). The intent of this booklet is to provide departments with an easy-to-use format that may be used as a template to develop a written exposure control plan tailored to the individual requirements of their department in conjunction with the exposure control plan for San Diego State University. Please allow all employees access via written or electronic copies to the department and university exposure control plan. E. EXPOSURE DETERMINATION Each employee must have an exposure evaluation based upon the job description and assigned tasks. The evaluation shall be reviewed with the employee at time of hire or within 90 days of the establishment of this program. Exposure evaluation shall be based upon a reasonably anticipated contact (skin, eye, mucous membrane, parenteral contact, etc.) with blood or other potentially infectious materials that may result from the performance of an employee's duties. As required by OSHA, exposure evaluations will be performed in accordance with a categorization scheme based on the potential of job-related tasks leading to exposure. The three categories used are: Category 1 Tasks that involve occupational exposure to blood, body fluids or tissues. Category 2 Tasks that involve no occupational exposure to blood, body fluids or tissues, but employment may require performing unplanned Category 1 procedures. Category 3 Tasks that involve no occupational exposure to blood, body fluids or tissues and Category 1 tasks are not a condition for employment. Table 1 presents a listing of job classifications identified to date that may be assigned to Categories 1 or 2. This list can be used as a guideline for categorization. Actual determinations for specific employees must be performed by EHS and the applicable supervisor. Table 1. List of Employee Assignments that Qualify as Category 1 or 2 for Purposes of Bloodborne Pathogen Control College, School, or Department College of Sciences Exercise and Nutritional Sciences Family Studies and Consumer Science Graduate School of Public Health Mechanical Engineering (Bioengineering) Psychology School of Nursing Student Health Services Employee Assignment Principal Investigators and researchers Technicians (including Student-techs) Phlebotomists Faculty, technicians, student workers Principal Investigator and researchers Technicians (including Student-techs) Principal Investigators and researchers Technicians (including Student-techs) Principal Investigators and researchers Technicians (including Student-techs) Principal Investigators and researchers Technicians (including Student-techs) Faculty, technicians, student workers Physicians, nurses, phlebotomists Guideline Category 2-3 2-3 1 1-2 2-3 2-3 2-3 2-3 2-3 2-3 2-3 2-3 1 1 Technicians, laboratory workers Student workers 1 1 F. METHODS OF COMPLIANCE The following methods shall be instituted as means of infection control. 1. Universal Precautions shall be utilized to prevent contact with blood and other potentially infectious materials. Universal precautions require that under circumstances in which differentiation between body fluid types is difficult or impossible, all body fluids shall be considered potentially infectious materials. 2. Engineering and Work Practice Controls shall be used to eliminate or minimize employee occupational exposure and examined and revised on an annual basis to ensure their effectiveness. All procedures involving blood or OPIM shall be performed in a manner as to minimize splashing, spraying and aerosolization. These controls shall include: a. Needleless systems shall be used. If needleless systems are not used, needles with engineered sharps injury protection shall be used. If sharps other than needle devices are used, these items shall include engineered sharp injury protection. This is for work with human or non-human primate work only, and not for all animal work. b. Needles and other sharps shall not be recapped, sheared, bent, broken or resheathed by hand. Used needles shall not be removed from disposable syringes. Disposable sharps shall not be reused. The entire unit shall be placed in a rigid, puncture-proof, leak resistant and properly labeled container such as a sharps container. c. Broken glassware that may be contaminated shall not be picked up directly with the hands. It shall be cleaned up using a brush, dustpan, tongs or forceps. d. Sharps containers shall not be opened, emptied or cleaned manually which would expose employees to the risk of sharps injury. e. Mouth pipetting/suctioning is prohibited. f. Eating, drinking, applying cosmetics or lip balm and handling contact lenses are prohibited in areas where there is a potential for occupational exposure. g. Food or drink shall not be stored in refrigerators, freezers or cabinets where blood or other potentially infectious materials are stored or other areas of possible contamination. h. Sharps container shall be closed immediately prior to removal or replacement to prevent spillage or protrusion of contents during handling, storage, transport or shipping and placed in a secondary container if leakage is possible. The secondary container shall be closable, leakproof and properly labeled. Regulated waste not consisting of sharps shall be disposed of in red bags, which are closable, leakproof and properly labeled. i. Specimens of blood or other potentially infectious materials shall be placed in a closable, leakproof container labeled or color-coded such as a red bag prior to storage, transportation or collection by disposal contractor. If outside contamination of the primary container is possible, a secondary container, also properly marked, shall be used. If a puncture of the primary container is likely, then it shall be placed within a leakproof, puncture resistant container. Reusable items contaminated with blood or OPIM shall be decontaminated prior to washing and/or reprocessing. j. Good Housekeeping shall be applied so that the work area is maintained in a clean and sanitary condition. A written schedule shall be implemented for cleaning and the proper method of disinfection or decontamination based upon location within the facility, type of surface, type of soil present and tasks or procedures being performed. All equipment and environmental working surfaces shall be properly cleaned and disinfected after contact with blood or other potentially infectious materials. Surfaces shall be cleaned after completion of procedures, when surfaces are overtly contaminated, immediately after any spill of blood or other infectious materials and at the conclusion of the work shift. Equipment that becomes contaminated with blood or other potentially infectious materials shall be decontaminated prior to servicing. k. All bins, pails, cans and similar receptacles intended for reuse which have a potential for becoming contaminated with blood or other potentially infectious materials shall be inspected, cleaned and disinfected on a regularly scheduled basis and cleaned and disinfected immediately or as soon as possible after visible contamination. l. Protective coverings such as imperviously backed absorbent paper, plastic wrap or aluminum foil may be used to cover equipment and surfaces. These coverings shall be changed at the conclusion of the work shift or when they become contaminated. m. Employees shall wash their hands immediately or as soon as possible after the removal of gloves or other PPE and after hand contact with blood or other potentially infectious materials. n. Contaminated laundry shall be handled as little as possible with a minimum of agitation and placed in properly labeled bags. Employees who have contact with contaminated laundry wear protective gloves and other protective clothing. This facility identifies the need for changes in engineering controls and work practices through review of OSHA records, employee interviews, committee activities, etc. We evaluate new procedures and new products regularly by literature review, supplier information and product consideration. Both front-line workers and management officials are involved in this process in the following manner: Safety Meetings, Tailgate Trainings, Environmental Health & Safety is responsible for ensuring that these recommendations are implemented. 3. Personal Protective Equipment (PPE) shall be provided by the university whenever there is potential for occupational exposure. supervisors/principal investigators/professors shall assure that employees under their direction use appropriate PPE including, but not limited to: gloves, gowns (or laboratory coats), fluid-proof aprons, head and foot coverings, face shields or masks and eye protection. PPE shall be easily accessible and issued at not cost to the employee in the appropriate sizes. Hypoallergenic gloves, glove liners and powderless gloves shall be accessible to employees who are allergic to the gloves normally provided. PPE shall be removed immediately upon leaving the work area or as soon as possible if overtly contaminated and placed in the properly labeled receptacle for storage, washing, decontamination or disposal. Training in the use of appropriate PPE for specific tasks or procedures in provided by the Environmental Health & Safety Department. Procedures for handling used PPE are provided at the training. PPE shall be removed immediately upon leaving the work area or as soon as possible if overtly contaminated and placed in the properly labeled receptacle for storage, washing, decontamination or disposal. a. Gloves shall be worn when the employee has the potential for the hands to have direct contact with blood or other potentially infectious materials, and when handling items or surfaces soiled with blood or other potentially infectious materials. Disposable (single use) gloves shall be replaced as soon as possible when visibly soiled, torn or punctured or whenever their ability to function as a barrier is compromised. They shall not be washed or disinfected for re-use or worn outside the containment area. b. Face shields, eye protection, respirators and masks shall be worn whenever splashes, spray, spatter, droplets or aerosols of blood or other potentially infectious materials may be generated and there is potential for eye, nose or mouth contamination. c. Gowns, aprons or laboratory coats or other forms of appropriate protective clothing shall be worn when there is the potential for occupational exposure. The clothing shall form an effective barrier against blood or other potentially infectious materials. Selection shall be based upon the task and potential for exposure. Additional PPE such as head and foot protection and fluid-proof clothing shall be worn as needed. 4. Housekeeping. Regulated waste is placed in containers which are closable, constructed to contain all contents and prevent leakage, appropriately labeled or color-coded (see the following section "Labels"), and closed prior to removal to prevent spillage or protrusion of contents during handling. Contaminated sharps are discarded immediately or as soon as possible in containers that are closable, puncture-resistant, leak proof on sides and bottoms, and appropriately labeled or color-coded. Bins and pails (e.g., wash or emesis basins) are cleaned and decontaminated as soon as feasible after visible contamination. Broken glassware that may be contaminated is only picked up using mechanical means, such as a brush and dustpan. 5. Laundry The following laundering requirements must be met: handle contaminated laundry as little as possible, with minimal agitation place wet contaminated laundry in leak-proof, labeled or color-coded containers before transport. Use red bags for this purpose. wear the following PPE when handling and/or sorting contaminated laundry: gloves, N95 mask. G. SPECIAL HANDLING - HIV, HBV AND HCV RESEARCH LABORATORIES All work that involves the manipulation, handling, culture, production and concentration of HIV, HBV or HCV by research laboratories and production facilities shall be performed in accordance with guidelines established by CDC/NIH in the publication Biosafety in Microbiological and Biomedical Laboratories (4th Ed., 1999) and the California OSHA Bloodborne Pathogen Standard (8 CCR 5193)l. Unless otherwise permitted by the IBC, laboratories working specifically with HIV, HBV or HCV must follow standard BSL 2 for handling clinical materials, and BSL 3 practices and procedures for growing and concentrating virus particles. The following are of particular importance with regard to control of bloodborne pathogens: 1. Standard Microbiological Practices Standard microbiological practices shall be followed by research laboratories and production facilities. 2. Special Practices All personnel engaged in work utilizing HIV, HBV or HCV shall adhere to the following special practices. a. Laboratory doors shall always be kept closed. b. Contaminated materials that are to be decontaminated away from the work area shall be placed in a durable, leakproof container that is closed before being removed from the work area. c. Access to the work area shall be limited to authorized personnel only. An access control procedure should be established whereby only persons who have been advised of the nature of the potential biohazard, and who comply with entry and exit procedures, shall be allowed to enter the work areas and animal rooms. d. Hazard warning signs incorporating the universal biohazard symbol shall be posted on all access doors. The sign shall identify the name of the infectious agent, special requirements for entering the area and the name and telephone number of the PI, laboratory manager or responsible person. e. ALL activities involving potentially infectious materials shall be conducted in BSCs or other physical-containment devices within the containment area. NO WORK SHALL BE CONDUCTED IN OPEN VESSELS ON THE OPEN BENCH. f. Laboratory coats, gowns, smocks or other protective clothing shall be used in the work area and animal rooms. Protective clothing shall not be worn outside of the area. Single use or disposable protective clothing shall be removed and disposed prior to leaving the work area. g. Avoid skin contact with infectious materials or infected animals. Gloves shall be worn. h. ALL potentially infected waste from work areas, including animal rooms, shall be placed in red bags and transported to designated collection sites for disposal contractor incineration. i. Vacuum lines shall be protected with HEPA (High Efficiency Particulate Air) filters and liquid disinfectant traps. j. Only needle locking syringes or disposable syringe-needle units shall be used for parenteral injection and aspiration of fluids or infectious materials from laboratory animals and diaphragm bottles. Needles or other sharps are prohibited for use in BSL 3 containment areas. Extreme caution should be used when handling needles and syringes to avoid autoinoculation or the generation of aerosols during use and disposal. k. Spills and accidents that result in exposures of employees to potentially infectious materials shall be immediately reported to the laboratory manager and EHS. l. Supervisors shall ensure that laboratory personnel are advised of the potential hazards and procedures to control those hazards. An Exposure Control Plan should be prepared for each laboratory involved in HIV, HBV or HCV handling. The Exposure Control Plan shall be required reading for all laboratory personnel. In addition, laboratory personnel shall read and comply with the practices and procedures described in the "SDSU Biohazard Control Program Manual" and other pertinent procedures. 3. Containment and Decontamination a. Certified BSCs - Class II or III or other appropriate combinations of personal protection or physical containment devices shall be used for all activities with potentially infectious materials that pose a threat of exposure to droplets, splashes, spills or aerosols. BSCs must be certified (according to NSF 49 Standards) upon installation, whenever they are moved and at least annually or more often as determined. b. Each laboratory must contain a sink for handwashing. c. An autoclave for decontamination of infectious laboratory wastes shall be available. H. HEPATITS B VACCINATIONS AND POST-EXPOSURE FOLLOWUPS 1. Overview Hepatitis B vaccinations shall be made available to any employee who has a potential for becoming exposed to blood or other potentially infectious materials. If an occupational exposure (HIV, HBV or HCV) occurs, a postexposure follow-up shall be provided. Post-exposure management including medical evaluations and procedures shall be performed by or under the supervision of a licensed physician and laboratory tests shall be conducted by an accredited laboratory. The evaluations and procedures shall be provided to the employee at a reasonable time and place and according to standard recommendations for medical practice. 2. HBV Vaccination Criteria HBV vaccinations shall be offered to all employees occupationally exposed on an average of one or more times per month (i.e., Category 1 or 2) to blood or other potentially infectious materials, unless the employee has had a previous HBV vaccination or unless antibody titer testing has revealed that the employee is immune. If the worker initially declines the HBV vaccination but at a later date decides to accept the HBV vaccine, SDSU will provide the vaccine. HBV antibody testing is available to employees whether or not they decide to receive the vaccine. (If the employee is found to be immune to HBV by virtue of an adequate antibody titer, SDSU is not required to offer the HBV vaccine to that worker). The vaccination shall be made available to the employee after training has been provided and within ten (10) working days of the initial assignment. 3. Notification Procedure The procedure whereby employees are notified and offered the HBV vaccination is as follows: a. EHS works with individual supervisors to identify Category 1 and Category 2 employees. b. EHS prepares a written notification package which is mailed to each employees identified as Category 1 or 2. c. EHS maintains a list of those individuals who accept the vaccination offer and works with individual departments and Student Health Services to coordinate the scheduling of vaccinations. Records of individuals accepting and rejecting the offer are maintained by EHS. 4. Post-Exposure Evaluation and Follow-Up Following an occupational exposure incident, a confidential medical evaluation and follow-up shall be made available to the individual(s) involved. The following elements shall be included: a. Documentation of the route(s) of exposure, HIV, HBV and HCV antibody status of the source material (or patient) - if known, and the circumstances in which the exposure occurred. b. Collection of blood from the employee as soon as possible after the exposure for determination of HIV, HBV and/or HCV status. (Actual antibody or antigen testing of the blood or serum sample shall be done at this time.) c. Follow-up of the exposed employee includes: antibody or antigen testing, counseling, illness reporting, and safe and effective post-exposure prophylaxis according to current medical practices. d. The university shall provide the attending physician evaluating an employee after an exposure incident the following information: (1) A copy of this regulation. (2) A description of the exposed employee's duties as they relate to the exposure incident. e. The physician shall provide the University with a copy of the medical evaluation and physician's written opinion (within fifteen days of the completion of the evaluation). SDSU shall provide the employee a copy of the medical evaluation and written opinion which would indicate: (1) The ability of the employee to receive the HBV vaccine. (2) A statement that the employee has been informed of the results of the medical evaluation and has been informed of any medical conditions resulting from exposure to blood or other potentially infectious materials which require further evaluation and treatment. (3) Documentation of the route(s) of exposure and circumstances under which exposure occurred. (4) Result of source material or individual, if available. f. Prophylaxis will be provided to occupationally exposed individuals with a high risk for sero-conversion. Treatment will begin within 2-4 hours after an exposure (HIV and HBV) has been reported. I. HAZARD COMMUNICATION 1. Signs and Labels a. Signs shall be posted at the entrance to the work areas which shall bear: (1) Name of the infectious agent(s). (2) International symbol for biohazard (Figure 1) in fluorescent orange-red. (3) Special requirements for entering the area. (4) Name and telephone number of the laboratory director or other responsible person. b. Warning labels shall be affixed to containers of infectious waste; refrigerators and freezers containing blood and other potentially infectious materials; and other containers used to store or transport blood or other potentially infectious materials. Labels shall have the international biohazard symbol. The labels shall be fluorescent orange or orange-red with lettering or symbols in a contrasting color. The labels shall either be an integral part of the container or shall be tightly affixed to the container by adhesive to prevent their loss or removal. EH&S is responsible for ensuring that warning labels are affixed or red bags are used as required if regulated waste or contaminated equipment is brought into the facility. Employees are to notify EH&S if they discover regulated waste containers, refrigerators containing blood or OPIM, contaminated equipment, etc., without proper labels. Labels can be obtained through San Diego State University, Environmental Health and Safety Department at Chemical Sciences Laboratory 106. Figure 1 Biohazard Symbol 1. Training Individual supervisors/principal investigators/professors, in consultation with EHS, shall ensure that all employees with potential for occupational exposure (Category 1 or 2) are trained in this standard and proper technique. The training program should include, but is not necessary limited to: o An explanation of the California OSHA Bloodborne Pathogen Standard. o An explanation of the epidemiology and symptoms of bloodborne diseases. o o o o o o o o An explanation of the modes of transmission of bloodborne pathogens. An explanation of SDSU's Bloodborne Pathogen Control Plan. An explanation of the appropriate methods for recognizing tasks and other activities that may involve exposure to blood and other potentially infectious materials. An explanation of the use and limitations of prudent practices that will prevent or reduce exposure. Information on PPE, including selection, use, cleaning, disposal and maintenance. Information on the Hepatitis B vaccine including efficacy, safety, method of administration, benefits of being vaccinated and free of charge. Information on emergency procedures, including reporting of incidents and medical follow-up. An explanation of the signs and labels. PIs shall ensure that employees are trained in and demonstrate proficiency in standard microbiological practices and in operations specific to the laboratory in question before being allowed to work with HIV, HBV or HCV. A progression of work assignments should be made as techniques are learned and proficiency is developed. J. RECORDKEEPING A system shall be established whereby medical records shall be prepared and maintained for each employee who may be occupationally exposed to blood or other infectious materials. Employee exposure and medical records will be maintained in accordance with Section G.6 of the SDSU Injury and Illness Prevention Program. 1. Medical Records Medical records shall remain confidential and will not be disclosed or reported to any person, except as required by regulation. The records shall be maintained for at least thirty (30) years and will include: Employees name and social security number. · A copy of the HBV vaccine records. · A copy of the results of all medical evaluations and follow-up. · The University's copy of the physicians' written opinion. · Copies of all information initially provided to the physician. 2. Training Records Training records shall be prepared and maintained by the College of Science and/or EHS and shall include the following information: · Dates of all training sessions. · Contents, outline or summary of the training. · Name of trainer. · Names and job titles of all attendees. 3. Sharps Injury Log The University shall establish and maintain a Sharps Injury Log, which is a record of each exposure incident involving a sharp. The Sharps Injury Log shall be maintained for 5 years from the date the exposure occurred. The information recorded shall include the following: · Date and time of the exposure incident. · Type and brand of sharp involved in the exposure incident. · Description of the exposure incident including: a. Job classification of the exposed employee. b. Work area where exposure occurred. c. Work procedure at the time of incident. d. How the incident occurred. e. Body part involved in the incident. f. If sharp had engineered sharps injury protection, whether protective mechanism was activated and whether the injury occurred before, during or after the protective mechanism was activated. Each exposure incident shall be recorded on the Sharps Injury Log within 14 working days of the date the incident is reported. The information in the Sharps Injury Log shall be recorded and maintained to protect the confidentiality of the injured employee. 4. Availability SDSU shall assure that all records required to be maintained by this Standard are available upon request to the regulatory agencies (Cal/OSHA, Cal/EPA, OSHA), the employee or their designated representative or any other person in accordance with 29 CFR 1910.1030 and 8 CCR 5193.