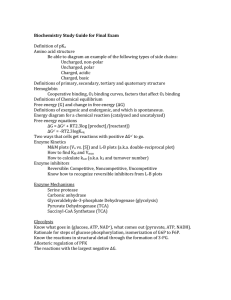
Document 17852375
advertisement

Chapter 18 Glycogen Metabolism I. Purpose: Glycogen is a branched polymer of glucose; it is the stored form of G. The many branches each have a C#4 end at which GP and GS can act for rapid response. Glycogen is stored after a meal for release: From liver when blood [G] is low to supply brain; OR In muscle for rapid activity. A. Main Enzymes 1. Glycogen Phosphorylase (GP): releases G as G1P: Gn + Pi G(n-1) + G1P (no ATP cost) GP removes G only from C#4 ends of chains that are at least five G’s from a branch (G1P equilibrates with G6P; this is not regulated) G1P<----> G6P 2. Glycogen Synthase (GS): adds G (as UDP–G) only to C#4 ends of chains. a) Preliminary: G G6P G1P ; then: G1P + UTP PPi + UDP–G b) GS rxn: Gn + UDP – G UDP + G(n +1) B. Other Enzymes of Glycogen synthesis/breakdown: 1. Debranching enzyme: after GP has removed all but the last 4 G residues from a branch, this enzyme: 1) catalyses transfer of 3 G residues to the C#4 end of a nearby branch and 2) catalyses hydrolysis of the 1 6 linkage, producing G 2. Branching Enzyme: transfers C#1 of a 7G residue segment (from a branch at least 11 G long) to the C#6 of a residue at least 4 G away. II. Regulation of GP, GS 1. GP is designated by 2 systems a/b and m/o, which we will not use. Instead, we will refer to the enzyme as: phosporylated (P) or dephosphorylated (DP) (GS is also P, DP). 2. GP and GS are phosphorylated in response to glucagon (in the liver) (low blood [G]) and adrenalin (muscle) (fight/flight), activating GP for release of G and inactivating GS. 3. GP kinase (GPK): GP + ATP ADP + GP–P. 4. They are dephosphorylated in response to insulin inactivating GP, activating GS to store G. 5. Regulatory effects a. GP-DP is: 1) activated by AMP. MR: GP provides GlP G6P for ATP production in glycolysis, and in OP via PDH, TCA, ET, OP. ML: [AMP] is high when ATP use is rapid and ATP production is needed. 2) inhibited by ATP. MR in 1). ML: when [ATP] is high, GP doesn’t need to release G to produce more 3) inhibited by G6P. MR: G6P is an indirect product of GP. ML: when [G6P] is high, GP doesn’t need to make more. b. GP-P is inhibited by glucose. MR: G is indirect product: GlP G6P G. ML: no need for more fuel when plenty is available c. GPK is activated by Ca2+. MR: GPK activates GP, which provides fuel for ATP production. ML: Ca2+ triggers muscle contraction, ATP production is needed. d. GS-DP is activated by G6P: MR: G6P is indirect substrate: G6P GlP UPD-G (feed forward) ML: when G6P is plentiful, it’s time to store G. III. Hormonal Regulation of Glycogen Metabolism. A. Enzyme Phosphorylation 1. The “hunger hormone”, glucagon is a signal to release G to blood from the liver via glycogenolysis and gluconeogenesis. Liver GP is activated, GS inhibited. 2. Adrenalin (epinephrine) is a signal to “break down” muscle glycogen to produce G6P for ATP production for fight-or-flight. Muscle GP is activated, GS inhibited. 3. Mechanism: When either of these binds its cell-membrane receptor, a. the hormone-receptor complex binds to adenylate cyclase and activates it to catalyse ATP PPi + cAMP b. cAMP is the internal or “2nd” messenger. It binds to protein kinase (PrK) regulatory (r) subunits, dissociating them from the catalytic (c) subunits, which are then active. c. PrK catalyses the phosphorylation of a variety of proteins, including: Glycogen synthase, inactivating it Glycogen phophorylase kinase (GPK), activating it. the tandem E (G’lysis) pyruvate kinase (G’lysis) AcoAcarboxylase (FA synthesis) d. GPK-P catalyses phosphorylation of glycogen phosphorylase (GP), activating it. e. Net hormonal effect: GP activated: Gn G; and GS inactive, preventing opposition to GP. B. Enzyme Dephosphorylation 1.Dephosphorylation of these enzymes (GPK, GP, GS) is catalyzed by phosphoprotein phosphatase 1 (PP1). 2. a. Phosphorylation of a regulatory glycogen binding protein, GM in response to insulin (which causes dephosphorylation of other Es) at site 1 activates it resulting in the opposite activities to the above (GS active to store the plentiful G, GP not, to prevent opposing GS). b. Phosphorylation of GM at site 2 (alone or in addition to site 1) by PrK inactivates it, preventing it from opposing PrK. 3. PrK also phosphorylates phosphoprotein phosphatase inhibitor 1 (PPI-1) causing it to bind to and inactivate PP1. 4. In Liver, the switch from the phospho- to the dephospho- state of the above cannot occur without the accumulation of glucose: “GP is the glucose sensor”: a. In the phospho (active) form, the P’s on GP are “buried” where PP1 can’t get at them. b. When G binds to active GP-P, its conformation changes, “exposing” the P’s so PP1 can “clip them” off. c. While PP1 is bound to GP-P in the R form the phosphatase (PP1) is not active toward other phosphoproteins. Only after GP-P binds G and PP1 dephosphorylates GP is PP1 released and active. d. PP1 has a much higher affinity for GP than for GS, GPK, etc, so it must first “work its way through” ~ all the GP-P, dephosphorylating it, before it has much effect on GS. C. Amplification cascade GP and GS are allosterically regulated by intracellular metabolites like AMP, ATP, G, and G6P. So why has a complex hormonal regulation scheme evolved? The big advantage is speed and magnitude of response: each enzymatic step amplifies the signal, and subsequent ones multiply previous ones: 1. each hormone-receptor complex activates one adenylate cyclase, which can produce, say 1000 cAMP/sec. 2. 4 cAMP can --> 2 active PrK which can produce, say, 100 GPK-P/sec. 3. Each GPK-P can phosphorylate, say, 100 GP/s. 4. So, the one H-R complex results in: 1000 cAMP x 2PrK/4 cAMP x 100 GPK-P/PrK x 100GP-P/GPK-P = 5,000,000 activated GP/sec, rather than 1 Enzyme/1 effector. That's why it’s called the" amplification cascade". IV. Glucokinase (GK) 1. GK catalyzes G + ATP G6P + ADP, same as HXK. 2. GK is a liver enzyme; muscle doesn’t have it (has HXK). 3. The properties of GK are more suited to maximum glycogen synthesis when [G] is high. HXK can also support rapid glycogen synthesis, but not as well as GK. 4. HXK is “designed” to keep up with extremely rapid glycolysis (if that’s the pace PFK sets): when PFK consumes F6P rapidly, G6P is also consumed rapidly, (G6P F6P) so that HXK is not inhibited by G6P. 5. But GK is not inhibited by G6P, so when [G] is high it can produce a much higher [G6P] which kinetically pushes glycogen synthase: via G6P GlP UDPG 6. GK has a much higher Km (lower affinity) for G so its rate is nearly proportional to [G] across the physiological [G] range. Chapter 25 FAs (fatty acids) I. Introduction 1. FAs are a much more efficient form of stored fuel: 9kcal/g (9 Cal/g) vs. (4 Cal/gG); also glycogen binds two times its weight of H2O. A typical man would have to store ~ 90 kg of glycogen (~200lbs) if he was to have the same energy as in the ~15 kg fat he stores. 2. Although glycolysis is a major fuel consuming pathway, FAs are the main fuel (except in brain, RBCs, rapid muscle activity). 3. Because of the above, glycogen storage is limited and “xs G” is converted to fat via glycolysis, PDH, CS and FA synthesis. II. FA use as fuel: A. 1. FAs are released (from storage as triacylglycerol) by the hydrolytic action of hormonesensitive lipase, which is activated by phosphorylation by PrK in response to adrenalin or glucagon, deactivated by dephosphorylation by PP1 in response to insulin. 2. FA’s then travel from adipose cells (“cytosol” is mainly a fat globule) in blood to cells that use them. 3. FA’s are prepared in the cytosol (cytoplasm) for transport to the mitochondrial matrix in FA activation: a. FA + ATP PPi + FA–AMP; b. FA–AMP + CoASH AMP + FA – SCoA (costs 2 ATP) 4. CoA from cytosol doesn’t enter matrix (or vice-versa). a. Instead, on outer surface of inner membrane, FA is transferred to carnitine (releasing CoASH to cytosol) in a rxn. catalyzed by carnitine acyltransferase I (CATI) (aka Carnitine PalmitoylTransferaseI, or CPTI). b. A transport protein in the inner membrane brings fatty-acyl carnitine into the matrix (in exchange for carnitine delivered outside). c. CATII (CPTII) on inner surface transfers FAcyl group from carnitine to CoASH. (Palmitate is the 16C saturated FA) B. 1. -oxidation converts the fatty acyl group to ACoA. Net reaction for palmitate: C15H31COSCoA + 7FAD + 7CoASH + 7NAD+ 8ACoA + 7FADH2 + 7NADH CH3(CH2)14CO2SH + 7CoASH +7NAD+ + 7FAD 8ACoA + 7NADH + 7FADH2 2. ATP production from -oxidation of palmitate (+ TCA, ET, and OP): a. 8XTCA: +8GTP + 24NADH + 8FADH2 b. ET: -31NADH – 15FADH2 c. OP: [+3(31) + 2(15)] ATP = + 123 ATP d. 123ATP + 8GTP – 2 “ATP” (ATP AMP in FA acivation ) = 129ATP C. Ketone body production 1. The moderate rate of production of acetoacetate, hydroxybutyrate and acetone that occurs normally in liver mito. matrix delivers “water soluble FA fragments” to cells via blood for use as fuel. 2. Since this process involves unregulated enzymes, the buildup of ACoA in diabetes overproduces these compounds to toxic levels. III. FA Synthesis (a liver pathway) The net effect is to build up the CH2 chain by joining ACoAs’ acetyl groups and reducing (and hydrogenating) the C=O. A. The ACoAs for FA synthesis don’t come from oxidation. Rather it’s the “xs G” that enters liver cells after a meal and goes through insulin stimulated glycolysis and PDH. But PDH is in matrix, FA sythase is in cytosol: 1. high ACoA from PDH stimulates PC high oxac. 2. (ACoA + oxac citrate) in matrix; then transport citrate to cyosol. 3. citrate cyto (ACoA + oxac) cyto (catalyzed by citrate lyas e) 4. oxac + NADH malate + NAD+ then, mal can enter matrix, OR 5. in cyto: mal + NADP+ NADPH + pyr + CO2 ; (pyr goes to matrix). this rxn is catalysed by the malic enzyme 6. The NADPH is needed for FA synthesis (below) 7. The cyto ACoA is activated for joining by conversion to malonyl CoA (carboxylation): ACoA + CO2 +ATP ---> ADP + Pi + mal CoA B. FA synthase: in E Coli, this consists of a number of separate enzymes, but in animals 2 identical subunits each contain the enzyme activities for all the rxns ( oxidation has a different enzyme for each step). 1. The substrate remains bound to the long phosphopantethein prosthetic group (Fig. 25-29, p931), which “carries” it to each of the various active sites. This is on ACP (acyl-carrier protein) 2. Phases of reaction “cycle”: a. Loading: the acetyl group of ACoA is transferred to a cys-S (viaACP) and the malonyl group of mal-CoA to ACP-S. b. Condensation, Reduction: C2 chains are linked, releasing CO2, then reduced to (CH2)2. c. Reloading: existing chain transferred to cys-S; next malonyl group to ACP-S (each mal of mal CoA goes onto ACP, only acetyl group of ACoA (and existing chain) go onto cys-S 3. Release: FA hydrolyzed from ACP IV. Regulation of FA Metabolism ACoAC A. ACoA Carboxylase (ACoA mal CoA) 1. Inhibited by palmitoyl CoA. MR: indirect product (mal CoA palmitate pal CoA) ML: If [pal CoA] is high, it is being produced faster than it can be used, production can slow) 2. Activated by citrate. MR: indirect substrate; citrate oxac + AcoA, the substrate ML: when[citrate] cyto is high, [citrate] mito is very high, fuel is plentiful, time to store it 3. Inhibited by phosphorylation in response to glucagon or adrenalin. These hormones promote fuel mobilization to make fuel available, so they inhibit storage. 4. Activated by dephosphorylation in response to insulin. Insulin “signals fed state”, when [G] is high it’s time to store C as glycogen and FAs. 5. Phosphorylation shifts ACoAC from active polymer form to inactive monomer form. B. Carnitine Acyl Transferase I (CATI) (transport of FAs into matrix for oxid’n). Inhibited by mal CoA. MR: mal CoA is the product of the committed step in the opposing pathway, FA synthesis. ML: When [mal CoA] is high, FA synthesis is rapid (in liver), with the purpose of export of these FA’s for storage. Inhib of CATI prevents consumption from working against synth. Chapter 26 Amino Acid (AA) oxidation A. Introduction 1. Part of the C’s of some of the AAs are convertible to ACoA, either directly or via acetoacetate or pyr. (and less directly, so are the others via TCA int oxac PEP pyr ACoA.) (These are the “ketgenic AAs.) So, these C’s of xs AA intake (in relation to need for protein synth) are used as fuel, just like dietary CH2O’s, fats. 2. Part (or all) of the C’s of 18 of the AAs can be converted to TCA intermediates, which can PEPCK be converted to G (TCA int oxac PEP G). These are referred to as the “glucogenic” AAs. AAs from digestion of muscle protein are the main source of C for gluconeogenesis in CH2O starvation B. Transaminations (trnsams) and Oxidative Deamination 1. Each AA can be converted to the corresponding keto acid by at least one transaminase. This AA is oxidized in this rxn, but kg is reduced to glu at the same time so not a net AA oxidation 2. Net oxidation occurs by coupling of trnsam with glutamate dehydrogenase (GDH). 3. GDH: glu + NAD+ kg + NADH + NH3 (this rxn running in reverse when [NH3] is very high depletes TCA ints, interferes with TCA +ET + OP in brain cells and causes the delirium/dementia in liver damaged patients) 4. The amino group transferred to kg (---> glu) is toxic when released as NH3 in GDH. This ammonia is detoxified by conversion to urea in the urea cycle (NH3 can be excreted). C. Regulation of AA Oxidation 1. GDH is inhibited by ATP and GTP and activated by ADP and GDP. MR: GDH + trnsam TCA ints TCA ET OP: ATP production ML: If [ATP] or [GTP] is high, more is not needed; if [ADP] or [GDP] is high, ATP synthesis is needed; TCA ATP 2. Carbamoyl Phosphate Synthetase I (CPSI) is activated by N-acetylglutamate (NAG). MR: is produced from ACoA and glutamate: ACoA + glu NAG. A high [ACoA] and/or a high [glu] increases the rate of NAG production and the [NAG], so the [NAG] indicates the levels of AcoA and glu. MR, ML for ACoA: when [ACoA] is high there is a need for oxac to react with ACoA in the CS reaction. GDH + trnsam can produce TCA ints from AAs at a high rate only if CPSI consumes the ammonia product of GDH. MR, ML for glu: when [glu] is high it has been produced by a high rate of trnsam and there is a need to convert it to kg in GDH to maintain [ kg] for TCA and trnsam. CPSI must consume the ammonia product of GDH in order for GDH to go. Diabetes Mellitus and Review of Hormonal Regulation of Metabolism Enzymes (Pathways) Glucagon Adrenaline (* = Phosphorylation) Liver Muscle Insulin (Dephospho) Liver Muscle Glycogen synthase* glycog phosphorylase* (synthesis/olysis) inh act olysis inh act olysis act inh synth tandem*: PFK2 FBPase2 [F2,6BP] PFK (Not*) FBPase (Not*) Pyruvate Kinase* (glycolysis/gluconeo) inh act low inh act inh neo act (hrt) inh (hrt) high (hrt) act (hrt) act inh high act inh act lysis ‘lysis (hrt) PDH (* but not in resp to glucag/adren) ACoA carboxylase* [malonyl CoA] lipase* FA (synth/oxid’n) act inh synth act inh low act (adipose) oxid oxid act high inh (adipose) synth 1. In type I diabetes, insulin is underproduced, glucagon is overproduced. So, even after a meal when blood [G] is high, the liver is responding to glucagon by producing G (for export to blood?) via gluconeogenesis and glycogenolysis and is also doing rapid FA and AA oxidation. (It should be responding to insulin and doing glycogen synthesis, and glycolysis/PDH/FA synthesis.) 2. G’neo consumes TCA intermediates (ox ac PEP). This depletes TCA because PC lacks pyr for pyr ox ac. Meanwhile, active FA oxidation produces high [ACoA], rapid ketone body synthesis. If this goes too far it results in ketoacidosis, even coma, death. 3. Other insulin effects: increases uptake of G into muscle and adipose tissue; also increases uptake of some AA’s and protein synthesis. Lack of these effects results in: a) AA’s being used for gluconeo rather than protein synth, muscle wasting, b) low glycolysis in adipose low glycerol phosphate (from DHAP) low FA storage as triacylglycerol. 4. Very high blood [G] exceeds capacity for reabsorption in distal tubule in kidney, G “spills” into urine. 5. Non-insulin-dependent diabetes in obesity is very common, results from overutilization of insulin response to eating. This causes decreases in insulin receptors by downregulating receptor synthesis. Cells can’t respond. May have normal insulin production or decreased. (“Adult onset”) 6. Type I is an autoimmune disease. A protein on the surface of the insulin secreting cells of the pancreas is very similar in structure and sequence to a surface protein of the coxsackie virus, which causes flu like symptoms. After infection, some of the person’s killer T cells have become activated against this protein, kill pancreatic cells.