Bringing I-PASS to the Bedside and the Unit Faculty Development
advertisement

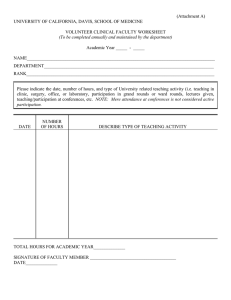
Bringing I-PASS to the Bedside and the Unit Faculty Development Learning Objectives • Activate and engage families and all members of the inter-professional team to create a shared mental model • Apply health literacy principles to improve communication • Incorporate I-PASS structured communication as an organizing framework for Family Centered Rounds • Demonstrate effective use of written information to facilitate communication with families and the interprofessional team • Describe the new paradigm for faculty/attending level workflow • List appropriate educational activities for Family Centered Rounds • Articulate how team communication occurs throughout the day Patient and Family Centered I-PASS Study We aim to: • Reduce serious medical errors • Improve FCR and daily communication • Improve the shared understanding of care plans between providers and patients and families • Improve the patient and provider experience Guiding principles: • Change FCR to enhance shared understanding • Optimize workflow • Maintain education time by reassigning “displaced” teaching Patient and Family Centered I-PASS Study Organizational Chart PRIS Executive Council Raj, Srivastava, Chair Christopher P.Landrigan Jay Berry Patrick Conway Ron Keren Sanjay Mahant Karen Wilson Theo Zaoutis Dissemination Committee I-PASS Executive Council Theodore C. Sectish, Chair Christopher P. Landrigan, P.I. Nancy D. Spector, Chair Christopher P. Landrigan. P.I. Theodore C. Sectish Amy J. Starmer Rajendu Srivastava Daniel C. West Scientific Oversight Committee Patient and Family Centered I-PASS Coordinating Council Alisa Khan, Co-Chair Daniel C. West, Co-Chair Christopher P. Landrigan. P.I. Dorene Balmer Maitreya Coffey Sarah Collins Katie Litterer Rita Pickler Nancy D. Spector Amy J. Starmer Christopher P. Landrigan. P.I., Chair Alisa Khan, Project Leader Michele Ashland Benard Dreyer Kate Langrish Theodore C. Sectish Nancy D. Spector Amy J. Starmer Rajendu Srivastava Daniel C. West Education Executive Committee Rounds Subcommittee Lauren Destino, Co-Chair Jennifer Everhart, Co-Chair Anupama Subramony, Co-Chair Brenda Allair Claire Alminde Marisa Atsatt Sharon Cray Liz Kruvand Nicholas Kuzma Glenn Rosenbluth Doug Thompson Becky Blankenburg Roben Harris Jennifer Baird Amy Guiot Leigh Anne Bakel PRIS Advisory Board Donald Berwick, IHI Brent C. James, IH Charles Homer, NICHQ QI and Implementation Subcommittee Data Coordinating Center Anuj K. Dalal, P.I. Stuart R. Lipsitz Kathy Zigmont Doernbecher Children’s Hospital OHSU Pilot Site Megan Aylor* Sarah Green Windy Stevenson Anne Bateman Mary Pozsgai St. Louis Children’s Hospital Mentor Site F. Sessions Cole* Kevin T. Barton Roben Harris Elizabeth Kruvand Michele Lane Kimberly Sauder Michael P. Turmelle Andrew J. White Amy J. Starmer, Chair Jennifer O’Toole Glenn Rosenbluth Daniel West Nancy Spector Ted Sectish Maria Obermeyer Jenni Baird Alisa Khan Ckaire Alminde Sharon Cray Shilpa Patel Advisory Board Alisa Khan, Co-Chair Theodore C. Sectish, Co-Chair Nancy D. Spector, Co-Chair Brenda Allair Jenni Baird Claire Alminde Becky Blankenburg Sharon Calaman Lauren Destino Benard Dreyer Jennifer Everhart Jennifer Hepps Christopher P. Landrigan, P.I. Christy Ledford Amanda Mangan Jennifer O’Toole Shilpa Patel Glenn Rosenbluth Raj Srivastava Amy Starmer Anupama Subramony Daniel West Clifton Yu Maria Obermeyer Health Literacy Subcommittee Benard Dreyer. Chair Wilma Alvarado-Little Cindy Brach Fernando Mendoza Vineeta Mittal Lee Sanders Michael Wolf Shonna Yin Faculty Development Subcommittee Shilpa Patel, Chair Jennifer K. O’Toole Nancy D. Spector Clifton E. Yu Ted Sectish Dan West Anu Subramony Sharon Calaman Arabella Simpkin Jennifer Hepps Education Committee Subcommittees and Advisory Groups Simulation and Educational Strategies Support Team Written Communication Tool Subcommittee Glenn Rosenbluth, Chair Benard Dreyer Brian Good Christy Ledford Dale Micalizzi Aarti Patel Jennifer Baird Doug Thompson Sally Coghlan McDonald Boston Children’s Hospital Pilot Site Christopher P. Landrigan* Brenda Allair Kelly Dunn Alisa Khan Katie Litterer Jayne Rogers Theodore C. Sectish Amy J. Starmer Laura Wood Jenni Baird Sharon Calaman, Co-Chair Jennifer Hepps, Co-Chair Jenni Baird Zia Bismilla Roben Harris Kheyandra Lewis Joe Lopreiato Clifton E. Yu Team Communication Subcommittee Clifton Yu, Chair Michelle Ashland Christy Ledford Nursing Rep Family Rep Campaign Subcommittee Glenn Rosenbluth, Chair Roben Harris Kheyandra Lewis Jennifer K. O’Toole Shilpa J. Patel Theodore C. Sectish Nancy D. Spector Clifton E. Yu James Bale Dorene Balmer F. Sessions Cole Kelly Dunn Benard Dreyer Helen Haskell Katherine Litterer Joseph Lopreiato Sanjay Mahant Christopher Maloney Dale Ann Micalizzi Vineeta Mittal Terrence O’Malley Mary Ottolini Jayne Rogers Samir Shah E. Douglas Thompson Clifton Yu Family Advisory Council Dale Ann Micalizzi, Co-Chair Helen Haskell, Co-Chair Brenda Allair Michele Ashland Marisa Atsatt Eileen Christensen Amanda Choudhary Sharon Cray Roben Harris Elizabeth Kruvand Katie Litterer Sally Coughlin McDonald Laquanna Williams Chelsea Welch Pat Katsis Peggy Markle Cindy Warnick Mary Pozsgai Nursing Advisory Council Jayne Rogers, Chair Claire Alminde Anne Bateman Kelly Dunn Michele Lane Kate Langrish Amanda Mangan Kimberly Sauder Stephanie Wintch Laura Wood Jenni Baird Annie Guerrero Maria Obermeyer Laura Trueman Debbie Chandler LeAnn Gubler Resident Focus Group Ad hoc members St. Christopher’s Hospital for Children Cincinnati Children’s Hospital Lucile Packard Children’s Hospital UCSF Benioff Children’s Hospital Hospital for Sick Children (Toronto) Walter Reed Military Medical Center Primary Children’s Hospital (Utah) Sharon Calaman* Sharon Cray Doug Thompson Nick Kuzma Kheyandra Lewis Nancy D. Spector Claire Alminde Laquanna Williams Jennifer K. O’Toole* Aarti Patel Maria Obermeyer Laura Trueman Debbie Chandler Lauren Destino* Michele Ashland Marisa Atsatt Becky Blankenburg Jennifer Everhart Joseph Kim Stephanie Wintch Glenn Rosenbluth* Daniel C. West Amanda Mangan Sally McDonald Zia Bismilla* Carolyn Beck Maitreya Coffey* Kate Langrish Pat Katsis Jennifer Hepps* Joseph O. Lopreiato* Clifton E. Yu* Peggy Markle James F. Bale* Brian Good* Amanda Choudhary Rajendu Srivastava Cindy Warnick Eileen Christensen Chelsea Welch LeAnn Gubler Annie Guerrero Communication on Family Centered Rounds Pilot Data • Pilot data from Boston Children’s Hospital – 45% discordance rate for understanding the plan of care between families and the medical team This is a patient safety issue! Khan A. Physician-Parent miscommunication in the hospital at night. PAS Meeting Vancouver, Canada; May 3, 2014. Patient and Family Centered I-PASS Educational Intervention Bundle Everyone has a role during FCR Team Member Role Patient & family Equal partners, speak first, give “illness severity” and “synthesis by receiver” Coach, advocate, provide information Orient, invite, introductions, I-PASS presentation/discussion Orient, invite, introductions, I-PASS presentation/discussion Oversee medical decision making, teaching, feedback Oversee medical decision making, teaching, feedback Interpret Ad hoc Nurses Medical students Interns Senior residents Attending Interpreters Other (SW, pharm, CM, RD, PT/ OT) Preparation For And Oversight Of Rounds What Am I Responsible For as the Attending? Oversight Of Team Activation • The attending is responsible for ensuring the patient, family and all team members are activated during rounds • Encourage team to let patient/families speak first • Ensure that nurses and other members of the care team get a chance to speak • Utilize TeamSTEPPS communication techniques Standardized Communication Techniques Support Situational Awareness and Shared Mental Model Technique Function Example Brief Plan team activities Day one discussion for team orientation Debrief Analyze an interim event Recap of events at the end of a shift Huddle Problem solve Planning for a procedure Cross monitoring / Feedback Improve performance Commenting about a decision (selected test) Assertive statement Advocate for safe, high quality care Recognizing a potential error Check back Ensure accurate information transfer Reading back a verbal order Handoff Transfer care and responsibility Transitions of care The Brief • Review situation awareness prior to rounds – Census and workflow – Admissions and discharges – Social considerations – Priorities • Sickest patients • Time sensitive decisions – Wean Albuterol – Schedule imaging procedures Huddles Before Going Into a Room • Occasional events • Provide opportunities to – Prioritize family’s questions and issues – Clarify care plans – Discuss sensitive issues – Prime learners to educational opportunities • Should not be a formal rounds presentation Debriefs Between Patients • Occasional events • Opportunities to – Clarify issues – Revisit teaching objectives – Give brief feedback • Be sensitive – Not within earshot – Not within sight Mid-Shift Huddle • Inter-professional team meeting typically late afternoon and on overnight rounds • Update on watchers • Concerns or problems • Changes in clinical status • Family concerns • Impediments to key action items • High level discussion of admissions and discharges Oversight Of Communication During Rounds • To keep the focus on the patient/family it is crucial that attendings • Ensure learners are using the principles of effective patient/family centered communication • Re-direct learners if presentations if they stray from the patient/family friendly format • Model effective use of interpreters and the rounds report printed tool Oversight of Team Positioning Senior Intern Attending Physicians and Medical Students Nurse Patient and Family Interpreter Other Team Members Attendings should facilitate proper positioning of team, computers The I-PASS Mnemonic I Illness Severity • Getting better, getting worse, about the same P Patient Summary • Problem oriented • Ongoing assessment and plan A Action List • To-do list S Situation Awareness & Contingency Planning • Knowing what’s going on • Planning for what might happen S Synthesis by Receiver • Check back: receiver summarizes what was heard, asks questions, restates key action/to do items Introductions First Presenter • Invites parents and patients to join FCR • Determines location • Reviews concepts and goals of FCR • Reviews time allotment and future check-ins • Introduces team members • Reinforces patient and parent roles as team members • Inquires about concerns Family Concerns • Provide the family with an opportunity to raise questions and concerns • Discuss concerns in the beginning to promote the development of a shared mental model Concerns Illness Severity • Articulate Illness Severity to assist in the development of a shared mental model • Provide the family an opportunity for their assessment of illness severity • May reveal a discordant understanding and offer an opportunity for clarification Illness Severity Patient Summary: Rethinking Oral Presentations on FCR • Problem-based discussion with the family – Move away from the formal presentation – Provide a brief summary statement/one-liner – Discuss problems in order of priority – Use evidence/data to support your A&P • • • • Overnight events Vital signs as applicable Physical findings Labs, test results – Use plain language = Pertinent Positives & Negatives Action List • Medical student or intern • Summary of main action items from the plan – Orders, consults, studies, procedures – Timeline: today, this week, before discharge • Order entry in real time • Ownership • Follow-up Situation Awareness & Contingency Planning • Problem solving before things go wrong • If this happens, then… from patient/ family/RN perspective Synthesis by Receiver • Brief synthesis of essential information • Opportunity for receiver to clarify information and have an active role on rounds • Demonstrates information is received and understood • Promotes a shared mental model Synthesis by Receiver • How do you ask a parent to synthesize? – Use open-ended questions • Not testing questions – Create a safe and welcoming environment – Be attuned to non-verbal cues that you observe in family members Oversight Of Communication During Rounds • Addressing discordant understanding – When illness severity is elicited – With check back for every patient • Learners will likely struggle with this skill; attendings will have to model how to execute effectively • Check back must occur in a way to not make patients/families feel like they are being tested – Encourage learners to: • Use close-ended probing questions • Articulate individual components of the A/P • Consider one-on-one discussion after rounds, written communication Preparing For Rounds As An Attending A Paradigm Shift • Rounds is now about the patient/family, and not for sharing information with the attending • Prior to rounds attendings must – Read admission note • Formal presentation from learners not necessary – Review notes and recommendations – Assist early learners • Set expectations for oral presentations – Not the traditional long H+P • Focus on clinical reasoning, gaps in knowledge, and rationale Rounds Report • Information intake is influenced by: – Stress, fatigue – Literacy level, learning styles, language – Access to technology • Benefits of Rounds Report: – Provides a document for families to refer to • Don’t have to remember everything • Can write down notes and questions – Can update as things change – May include pictures and diagrams Rounds Report Key Data Elements • • • • Name Date Parental concerns or questions Illness severity – Overall, how is your child doing compared to yesterday? • Patient summary – Updates • What is new or changed • What needs to happen before the child is ready to leave the hospital • Action list – What should be done today • Situational Awareness and Contingency Plan – Things that might happen and what to do about them Teaching on FCR • Benefits – Enhancement of clinical education through exposure to multiple patients by all team members – Ability to teach, model, observe, and evaluate clinical skills more effectively than “sitting” rounds • Challenges – Not all teaching topics amenable to discussion in presence of patient/family – Perceptions about rounding inefficiency if not done correctly General Rules on Teaching Topics • At the bedside – Physical examination – Clinical reasoning (assessment, prioritized DDx, work-up/treatment options) – Provider-patient communication – Anticipatory guidance – Professionalism – Other things that benefit the family and learners • Outside patient room; pre-round/educational huddles – – – – – – Psychosocial issues Pathophysiology Sensitive differential diagnosis discussions Issues unrelated to patient care Longer/foundational teaching sessions Formal presentations Educational Huddle Venue for Teaching Residents and Students • Brief teaching – On FCR between patients – After FCR at other times of the day • Teaching topics – Pathophysiology – Communication skills (priming, debriefing) – Review of overnight events – Systems-based practice – Sensitive social issues – Practice sessions for performing formal presentations Sample Bedside Teaching Techniques • 1 minute preceptor • Rounding like a Ninja and Karate Kid Physical Exam Skills • Focus on a single physical exam skill • Involve the child and child’s family – Respiratory distress in an infant: Let’s go look at the belly together to have a shared understanding of what respiratory distress looks like and what is normal breathing • Allow parent to be close to the child • Preserve modesty http://www.med-ed.virginia.edu/courses/pom1/PhysicalExamLinkPage.cfm http://www.easyauscultation.com/ http://www.med.ucla.edu/wilkes/ http://www.blaufuss.org/ www.learnpediatrics.com Communication Skills • Role modeling • When possible – Prime • “We are about to see a patient with an ambiguous diagnosis, pay attention to how the intern introduces…” – Debrief • “The family is understandably upset by the delays in care. What did you notice the senior doing to address their concerns? What else could our team have done to let them know we were listening?” How to Make Teaching Family Centered Do • Explain that teaching is an important part of rounds • Highlight when teaching is happening • Acknowledge family's input into teaching • Consider the impact of discussions outside the room when visible to parents – Alleviate family anxiety by explaining the need to have some deeper discussions about the medicine • Reframe a learner’s incorrect answers as thought processes • Model critical thinking and medical decisionmaking How to Make Teaching Family Centered Don’t • Assume families cannot understand clinical terms – Families may be more knowledgeable and can be quick studies • Engage in teaching behaviors that remove the child and family from the experience – Relate to the patient during the physical exam • Recite medical information about the patient as if they were not present • Tell families things are not relevant to their child – Save that for an educational huddle How to Respond to Wrong Answers • “That is an interesting thought…however, in Johnny’s case, symptoms A and B make me think that diagnosis X might be more likely.” • “Tell me more about that.” • “It is good we are having this discussion and considering all of the possibilities.” • Don’t say: “We’ll talk more about that later.” Large Group Discussion • Do you incorporate any of these practices into your rounding workflow already? – Benefits? – Challenges? • How do you think this will impact your workflow? • How do you think this will impact learner education? • How do you think this will impact the experience of patients/families?