Global TB Research – as part of the new End... Strategy Dr Dick Menzies Research Methods course
advertisement

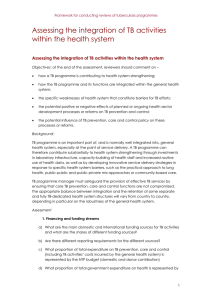
Global TB Research – as part of the new End TB Strategy Dr Dick Menzies Research Methods course McGill University – 6-10 July 2015 The Global Burden of TB - 2013 Estimated number of cases All forms of TB 9 million 126 per 100,000 • 550,000 in children • 3.3 m in women Estimated number of deaths 1.5 million* • 80.000 in children • 510.000 in women HIV-associated TB 1.1 million (13%) 360,000 Multidrug-resistant TB 480,000 210,000 Source: WHO Global TB Report 2014 * Including deaths attributed to HIV/TB TB cases and deaths in slow decline, 1990-2013 All TB deaths Incidence peaked at 9.5 million in 2004 9 million in 2013 Total mortality peaked in 2002 at 1.7 million 1.5 million in 2013 Full implementation of Global Plan: 2015 MDG target reached but TB will not be eliminated by 2050 Current rate of decline -1.5%/yr China, Cambodia -4%/yr W Europe 1950-60s -10%/yr Elimination target:<1 / million/yr -20%/yr The End TB Strategy: Vision, goal, targets 2035 Vision: A world free of TB Zero TB deaths, Zero TB disease, and Zero TB suffering Goal: End the Global TB epidemic (<10 cases per 100,000) Target 1 95% reduction in deaths due to TB (compared with 2015) Target 2 90% reduction in TB incidence rate (compared with 2015) Target 3 No affected families face catastrophic costs due to TB The End TB Strategy - Components 1. INTEGRATED, PATIENT-CENTRED CARE AND PREVENTION A. Early diagnosis of tuberculosis including universal drug-susceptibility testing, and systematic screening of contacts and high-risk groups B. Treatment of all people with tuberculosis including drug-resistant tuberculosis, and patient support C. Collaborative tuberculosis/HIV activities, and management of co-morbidities D. Preventive treatment of persons at high risk, and vaccination against tuberculosis 2. BOLD POLICIES AND SUPPORTIVE SYSTEMS A. Political commitment with adequate resources for tuberculosis care and prevention B. Engagement of communities, civil society organizations, and public and private care providers C. Universal health coverage policy, and regulatory frameworks for case notification, vital registration, quality and rational use of medicines, and infection control D. Social protection, poverty alleviation and actions on other determinants of tuberculosis 3. INTENSIFIED RESEARCH AND INNOVATION A. Discovery, development and rapid uptake of new tools, interventions and strategies B. Research to optimize implementation and impact, and promote innovations Projected acceleration of TB incidence decline to target levels Current global trend: -1.5%/year Optimize use of current & new tools emerging from pipeline, pursue UHC and social protection Average -10%/year by 2025 Introduce new tools: a vaccine, a new easier prophylaxis & Average treatment regimen, a PoC test -17%/year -5%/year Global TB diagnostics Pipeline - 2013 GLOBAL TB PROGRAMME Global TB Drug Pipeline 2013 Discovery1 Preclinical Development Lead Optimization Diarylquinoline DprE Inhibitors GyrB inhibitors InhA Inhibitors LeuRS Inhibitors MGyrX1 inhibitors Mycobacterial Gyrase Inhibitors Pyrazinamide Analogs Riminophenazines Ruthenium (II) complexes Spectinamides Translocase-1 Inhibitors Preclinical Development CPZEN-45 DC-159a Q201 SQ609 SQ641 Clinical Development GLP Tox. Phase I BTZ043 TBA-354 4 Repurposed Drugs 6 New Drugs 3 New Classes Phase II Phase III AZD5847 Bedaquiline (TMC-207) Linezolid Novel Regimens2 PA-824 Rifapentine SQ-109 Sutezolid (PNU-100480) Delamanid (OPC-67683) Gatifloxacin Moxifloxacin Rifapentine Drugs currently in the regulatory review process Chemical classes: fluoroquinolone, rifamycin, oxazolidinone, nitroimidazole, diarylquinoline, benzothiazinone 1 Ongoing projects without a lead compound series can be viewed at http://www.newtbdrugs.org/pipeline-discovery.php. 2 Combination regimens: first clinical trial (NC001) of a novel TB drug regimen testing the three drug combination of PA-824, moxifloxacin, and pyrazinamide was initiated November 2010 and completed in 2011 with promising results. The second clinical trial (NC002) of this regimen was launched in March 2012 and will test the efficacy of the regimen in drug-sensitive and multidrug-resistant patients. The third clinical trial (NC003) will evaluate PA-824, TMC-207, pyrazinamide and clofazimine in combinations and is scheduled to begin September 2012. www.newtbdrugs.org Updated: June 18, 2013 Global TB Vaccine Pipeline 2013: Phase II Ad5 Ag85A McMaster CanSino ID93 + GLA-SE IDRI, Aeras Hyvac 4/ AERAS-404 + IC31 SSI, sanofi-pasteur, Aeras, Intercell H56 + IC31 SSI, Aeras, Intercell MTBVAC TBVI, Zaragoza, Biofabri Hybrid-I + CAF01 SSI, TBVI VPM 1002 Max Planck, VPM, TBVI Hybrid-I + IC31 SSI, TBVI, EDCTP, Intercell RUTI Archivel Farma, S.L Phase IIb Phase III MVA85A/AERAS485 OETC, Aeras AERAS-402/ Crucell Ad35 Crucell, Aeras M72 + AS01 GSK, Aeras M. Vaccae Anhui Longcom, China Viral vector rBCG Protein/adjuvant Attenuated M.tb Immunotherapeutic: Mycobacterial – whole cell or extract 10 Implementation, and research - need financing IMPLEMENTATION $2 billion Funding gap RESEARCH $ 6 billion available $1.32 billion Funding gap $8 billion funding required for TB prevention, diagnosis and treatment $677 M $2 billion funding required for research and development TAG TB R&D report 2013 Total TB R&D Funding, 2005-2013: flat line $675,328,887 $700,000,000 $643,360,390 $636,979,349 $676,656,323 $638,783,272 $494,576,235 $525,000,000 $478,343,421 $418,928,300 $358,476,537 $350,000,000 $175,000,000 $0 2005 2006 2007 2008 2009 2010 2011 2012 2013 but receives TB has killed more people… less funding $43 BILLION HIV/AIDS GLOBAL FUNDING Malaria 1813-2013 30,000,000 $7 Billion TB HIV/AIDS deathGlobal Funding Source: Nature Vol 502, No. 7470 Suppl, S2 (2013) Tuberculosis 1990-2010 Source: Financing Global Health 2012, IHME; Aeras Global Consultation on Research for TB Elimination Stockholm, Nov 2014 Meeting objectives: •To review the existing mechanisms, funding and capacity for TB research, identify gaps and propose new mechanisms of collaboration, capacity building and resource mobilization, •To outline a global framework to operationalize pillar 3 that addresses TB research planning, capacity-strengthening and research funding in all countries GLOBAL TB PROGRAMME 14 Global Consultation on Research for TB Elimination Stockholm, Nov 2014 Main Output: Development of a Global Action Framework for TB Research aimed at the operationalization of research for TB elimination, with: → a 10 year vision (2025) towards reaching the 2035 targets of the End TB Strategy → a 5-year strategic plan to implement Pillar 3 of the End TB Strategy → a 1-year operational plan with specifics at global and national levels: - enhance use of current resources, - strengthen country specific research programs, - strengthen research capacity, - identify mechanisms for innovative financing of research. GLOBAL TB PROGRAMME 15 The Global Action Framework for TB Research The Global Action Framework for TB Research sets the principles for action on TB research and recommends the roles, responsibilities and deliverables of major stakeholders at global and national levels. Four main parts: - Part I: Strengthening TB research in low and middle-income countries most affected by TB. - Part II: Supporting and facilitating research at global level. - Part III: Supportive role of WHO - Part IV: Next steps. Supporting and facilitating research at global level Aim: to support and reinforce the efforts invested at national level through the development of strong research partnerships and networks, accompanied by reinvigorated funding for TB research and development. 1. Mobilizing increased resources for TB research: - Expand international funding sources to support research in low and middle income countries - Hold regular TB research donors’ forum - Stimulate the development of innovative funding mechanisms - enhance advocacy globally and nationally Supporting and facilitating research at global level 2. Enhance international collaboration on TB research. - Pursue an international mapping of TB research - Compile an international compendium of funding opportunities - Stimulate the creation of international networks and thematic hubs - Encourage large scale, cross-cutting multi-disciplinary multi-site collaborative research projects Role of WHO 1. Provide Technical Assistance to countries. 2. Develops guidance tools and documents (e.g. “How to form a TB research network”, “How to develop a National TB Research Agenda”, etc.). 3. Work with international and bilateral agencies that are providing support to countries for various forms of research 4. Foster support for dissemination of research outputs and uptake by countries (eg Xpert, new TB drugs, etc) 5. Enhance data sharing 6. Convene meetings and facilitate communication 7. Establish a Global TB Research Task Force that will assist in implementation of the Global Action Framework Strengthening TB research in low and middleincome countries most affected by TB – Key steps 1. Development/reinforcement of a national TB research network, 2. Development of a country-specific TB research strategy and priorities based on the characteristics of the TB epidemic and the mapping of resources and activities at country level, 3. Plan for relevant training and capacity building on (TB) research from an early stage, 4. Ensure sustained national TB research funding mechanism for training, infrastructure and research operations, 5. Establish mechanisms for on-going monitoring and evaluation of the implementation of the TB research action framework, 6. Advocate for public support and funding of TB research. Strengthening TB research in low and middle-income countries most affected by TB – Key steps 1. Establish/Strengthen an integrated national TB research network 1. Members: - NTP/MoH and other Ministries. A “Focal point in research” within NTP is often a successful linkage - University based researchers (a focal point for NTP can be appointed) - NGO’s / international organizations - Civil society 2. Funding – modest funding for meetings/secretariat needed – long term 3. Leadership – ideally rotates between members 4. Functions: Regular meetings - Scientific meetings - Set national research agenda - Help coordinate projects Strengthening TB research in low and middle-income countries most affected by TB – Key steps 2. Establish/update National strategic plan for TB research 1. This should be developed by all stakeholders Could be a responsibility of the TB Research Network 2. Based on the needs and capacity of the country - Assessment of the TB epidemic – incidence, HIV-TB, DR-TB, etc. - Inventory of current TB research and research capacity (Research teams/institutes/universities) 3. Development of country-specific TB research priorities. 4. Needs to be part of a National TB Strategic plan Strengthening TB research in low and middle-income countries most affected by TB – Key steps 3. Publicly Funded Plan to build and maintain capacity for TB Research 1. Training in Research at several levels - Under-grad – medical schools and others - Post-grad – Master’s and PhD levels - Methodologies – include the spectrum of research (basic to operational) 2. Salaries – for researchers - Through competitive mechanisms - Through universities or research institutes 3. Infrastructure - Labs – for basic research, or to support clinical research (RCTs) - Personnel – research coordinators, data analysts, etc Strengthening TB research in low and middle-income countries most affected by TB – Key steps 4. National funding for TB Research. 1. This should be part of general plan for health research funding 2. Funding should come from national Government - Ministries of Health, or Science & Technology … 3. Other sources could include - Industry (Pharmaceuticals, Diagnostics) - Donors/NGOs (eg. Global Fund, USAID) 4. Commitment should be long-term - smaller funds that are stable more likely to affect career choices 5. Mechanism – suggested based on best model in high income countries: - open and transparent process - peer reviewed Model countries – roles and expected outcomes • Objective: develop models for implementation of “Pillar 3” within low/middle income countries that have high TB burden. • Selection criteria: ad hoc process - self-identified. • Role: Partner with WHO to produce examples of successful implementation that other LMIC may follow in next 10 years • Outcomes: – Achieve within one year (by June 2016) the milestones outlined above for low-middle countries – Evaluate and document major roadblocks as well as key factors in success Potential 'path-finder' or Model countries • • • • • • Brazil* India Indonesia* Peru South Africa Vietnam Brazil • • • Status at end 2014: – Functioning TB research network (REDE-TB since 10 years) – Very well funded research training (Science without Borders) – Well funded peer-reviewed research funding – Substantial international collaborations (NIH, Gates) Progress in 2015: – Survey (investigator, health system managers, industry and NGO) to identify Gaps and Research Priorities – Joint meetings of REDE-TB, Government, NTP, Fiocruz – Updated the Brazil national TB research strategy/Research Agenda – Formulated plans for immediate action in new tools Plans up to June 2016: – Fiocruz – develop a new Tuberculin. NTP & Universities – will test – Industry/REDE TB – impact of new Diagnostic for MDR-TB (replace liquid culture). – Industry /REDE TB – impact of TB eXiST for XDR-TB diagnosis. – International – collaboration with China in Translational research – International – Promote cost sharing model of NIH-MoH-Brazil (Report Brazil) Indonesia • Status at end 2014: – Functioning TB research network - TORG (Tuberculosis operational research group) since 10 years – Several university based research groups with well trained researchers (largely through Netherlands) – Challenge TB country • Progress in 2015: – Expansion of TORG – involve NTP manager, WHO country rep, others – Involvement of TORG in Global Fund concept note • Plans up to June 2016: – Recent meeting of TORG – consensus to push forward as ‘model country’ – Meeting of all stake-holders re National TB research strategy – September 2015 Model countries: Milestones and deliverables – 1 year Specific One-year Objectives for Model countries 1. Establish/Strengthen an integrated national TB research network, linked with regional and international collaborations 2. Establish/update a National strategic plan for TB research, as part of National Strategic plan for TB. 3. Plan to build and maintain capacity for TB Research – part of a national plan to build/maintain capacity for all health research. 4. Establish mechanisms for public funding for TB Research - part of a national plan for all-health research funding Model countries: Milestones and deliverables – 5 year Specific Five-year Objectives for Model countries 1. Will have established mechanisms for national funding for TB research with regular (e.g. annual) national competitions for research operating funds. 2. Will have established mechanisms to review and finance the research and development components of the Stop TB Partnership’s Global Plan 2016-2020. All other LMIC: Milestones and deliverables – 5 year All other low and middle income countries with substantial TB burden will have (at minimum): 1. established a National TB Research Network that includes at least researchers, academia, the National TB Programme and other relevant stakeholders. 2. developed and started implementing a national TB Research Strategic Plan with clear TB research priorities. 3. initiated in-country research training with national faculty (minimum – have the capacity within the country to deliver operational research training). All LMIC: Milestones and deliverables – 10 years 1) Implemented a national TB research strategic plan with a TB specific prioritized research agenda within a larger health research agenda; 2) Established sustained national TB research funding mechanism(s): - based on the national research priorities; - Funds a broad spectrum of research efforts on TB (from basic to operational as appropriate to country settings and resources). 3) Created/strengthened TB research capacity: - including training, mentoring and career support. - well-defined roles for governmental agencies and national TB programmes (NTP), universities/medical schools/research institutions, private sector, and NGOs. 4) Empowered a strong and self-sustaining TB research community (i.e., a critical mass within the country), which is productive, addressing national priorities, and linked with regional hubs and international networks of research. The 10 year vision - by 2025 1. Greatly increased capacity and leadership for TB Research in high TB-burden countries. This means a strong and self-sustaining TB research community in these countries, 2. Major increase of government and industry financing for TB Research – especially in middle-income high TB-burden countries, including the BRICS, 3. Further increased commitment and financing for global TB R&D in high-income countries, 4. Enhance international collaboration within the larger context of health research. Next steps 1. Post STAG Workshop: - Training WHO country/regional staff on Pillar 3 - Global Action Framework - Up-date operationalization documents – “how-to” initiate/strengthen TB research in LMIC. 2. Global TB Research Task force: - Initial meeting - Q4 of 2015 - Evaluate progress, refine indicators, suggest actions 3. International Union Conference, Cape-town: - Symposium on “End TB Strategy - Pillar 3”. Speakers from “model countries” (researchers and NTP) – describe process, obstacles and lessons learnt 4. Continue work with Model countries: - Update Framework – with various new models that have worked "The struggle [against tuberculosis] has caught hold along the whole line and enthusiasm for the lofty aim runs so high that a slackening is no longer to be feared. If the work goes on in this powerful way, then the victory must be won". Robert Koch, Nobel Lecture December 12, 1905. Acknowledgements – ideas, input, (and ppt slides) Christian Lienhardt (slides) Knut Lonnroth Mario Raviglione (slides) Mukund Uplekar Diana Weil … All Stockholm meeting attendees …. And all those who are taking research forward in Model countries GLOBAL TB PROGRAMME 36