Internal Medicine Housestaff Survival Guide & Quick Reference
advertisement

Internal Medicine Housestaff
Survival Guide &
Quick Reference
2010-2011
13th Edition
The University of Tennessee
Health Science Center
Internal Medicine Residency Program
Index I
3
Medicine Ward Expectations and Survival Tips
5
Night Float Expectations and Survival Tips
The Night Float System
8
Cross-Cover Guide for Common Problems On-Call
Acute Chest Pain
Acute Shortness of Breath
Altered Mental Status
Fever On Call
Falls Out of Bed
20
Death Pronouncement
21
Prescription Numbers
21
Dictation Information
22
Regional Medical Center at Memphis (MED)
Phone Numbers
Computer
Dictation
Discharge
25
Baptist Memorial Hospital
Phone Numbers
Computer
Dictation
~1~
Index II
General Program Information, Policies, and Requirements
29
29
30
30
32
33
34
34
35
36
36
36
37
38
38
39
40
40
41
41
41
42
44
44
45
46
46
47
47
49
Campus Training Lessons
Clinical Evaluation Exercise
Conference Attendance
Core Competencies
Curriculum and Syllabi
Duty Hours
Email Policy
Evaluations Policy
Fatigue Policy
Housestaff Manual
Internal Medicine In-training Examination
Internal Medicine Website
Leave Policy
Mail
Medical Records
Moonlighting Policy and Requirement
Non-teaching Patients
Pagers
Paychecks
Portfolio
Procedures
Professional Conduct
Research Rotation
Stipend
Supervision Policy
SVMIC Conference
TB Testing
Teaching Responsibilities
Travel to Meetings
Mini-CEX forms
* This is not a complete list of policies. You should review all program policies on the
program website.
~2~
Medicine Ward Expectations and Survival Tips
All patients should have notes written by an intern daily.
All notes have to be written and on the chart by 9-10am.
The hour between 9 and 10am will be used for pre rounds with
the resident and for discharging.
All new patients are to be seen immediately after intake
rounds.
All new patients should have an order to change the team and
provide pager numbers once assigned to you.
Each note should keep track of antibiotic days (if applicable).
Check each patient’s MAR daily to make sure appropriate
meds are still given and inappropriate meds are not.
Each note should address the current active issues and plans
for discharge.
The orange “Anticipate DC tomorrow” note should be placed
on the charts with pertinent information addressing the things
that we will need to have done in order for the DC to happen.
On days off, the interns are to check out their patients to the
other intern the day before so that ALL patients are covered
the next day.
All interns and medical students are to go to Morning Report.
Once noon conference starts, all team members are to attend.
Once your clinic starts, all patients have to be seen and notes
written prior to your clinic if time permits. If not, check on any
critical pts and check the rest out to the resident and/or other
team members (intern or JI) prior to leaving for clinic. This will
obviously be easier for those who have Methodist clinics, but
we must work together to get all pts seen.
All tests (Cxs, special labs, images, etc) ordered need to be
personally followed up. If time permits, go to the CT room or
Echo lab, etc and review images with the STAFF or Fellow! Do
not wait for results to show up in the computer; that may take
days!
~3~
The patient list is to be updated daily. That means all new
pertinent information (meds, test results, room numbers, etc.)
needs to be on the list by check out.
When discharging a patient, make sure to know who/where
they are following up and have the unit secretary make the
appointment prior to DC. Also, make sure the patient
understands all DC meds, especially if there are changes in
doses, amounts, new medications, etc., so that duplicate meds
(classes or the same med) aren’t taken, and explain that in
your dictation.
All dictations are to be done the same day. Sign your
dictations!
Each intern/JI should check out his/her own patients face-toface at the end of each day.
~4~
Night Float Expectations and Survival Tips
The goal is to work effectively together to get the pts seen and
orders written in a timely fashion and not compromise pt care.
Show up on time so that the day team can check out before we start
getting admissions.
If you switch with another Intern, please inform the operators so the
floors know who to call for each team.
Once you get an admission, if you are not taking care of a critically
ill patient, proceed immediately to the ER because it’s easy to get
behind once you’re down there.
Try to write some basic orders soon after you see the pt. If there is
time, you can finish up with the complete orders and then write your
note. If a bed hasn’t been ordered or you want to switch bed
assignments, please let the charge nurse know ASAP.
Orders should be written clearly and concisely. An example would
be as such:
“ADC VAAN DIMLS”
A – Admit to “team”, attending, resident, intern (pager #), to
floor (tele, medicine, PCU, etc.)
D – Dx. First list what the pt is being admitted for (primary),
then list secondaries (e.g. HTN, DM2, obesity, etc.)
C – Condition. No one’s condition is “stable”. It’s either good,
fair, guarded, or critical.
V – Vitals. Please don’t write routine unless they’re going to
the ICU. Write what you want, Q4 or Q6, etc. Here, also write
telemetry orders, neurochecks, etc.
A – Allergies
A – Activity. Remember that if you want I/Os, they cannot have
BRP.
N – Nursing orders. Parameters if you chose, precautions,
Accuchecks, etc.
D – Diet. Specify what type and how many calories
(sometimes not needed).
~5~
I – IVFs. Please write duration of fluids or amount to be given.
You don’t want the pts to mistakenly get IVFs when they don’t
need them. You can always restart if you fall short.
M – Meds. List them in numerical order so that it is VERY
CLEAR what you want and when! Don’t forget prophylactic
meds if applicable.
L – Labs. I usually write one line for Stat/Now Labs, then
another line for AM labs. Please date and time the labs so they
know when to draw them (e.g. 8/23 0600).
S – Special Orders (you don’t have to write Special Orders)
but here you would write orders such as consults (If emergent,
we call our own consults, even in the middle of the night),
imaging studies (x-rays, USG, CTs), EKGs, old charts,
vaccinations, counseling, etc.
Please TIME/DATE and SIGN your orders! You would be amazed
at how you can forget simple things like this when you’re 3 pts
behind.
Night Float System
MED
Sunday-Thursday
Long Call - 7:30am-4:30pm- The long call team admits.
Day Float - 4:30pm-7:30pm- The dayfloat resident admits.
Night Float*-7:30pm-7:30am- The night float team admits the
patients. These patients are distributed to the ward teams the
following morning.
*For Friday-Saturday, residents & interns on electives take call as the night float team.
MUH
7 Days A Week
Short Call-7:30am-2:00pm (5 pt cap)-The short call team will admit
until 2:00 pm or until 5 patients are admitted, whichever occurs first.
~6~
Long Call-2:00pm-7:30pm-The long call team will start admitting
patients at 2:00 pm or once the short team reaches its cap of 5.
Call will end at 7:30 pm when the night float team arrives. The long
call interns will provide cross-cover until 7:30 pm and will receive
check-out from the other teams.
Night Float**-7:30pm-7:30am-The night float team will admit
patients between 7:30 pm and 7:30 am. These patients will be
distributed to the ward teams upon admission; the team with the
fewest patients will be the first team to receive new admissions.
The night float interns will provide cross-cover overnight and will
receive check-out from the long call interns.
**For Friday-Saturday, The long call resident will act as the night float resident on the
weekends. Interns on electives will provide night float coverage at this time.
VAMC
7 Days A Week
Short Call-7:30am-3:00pm (4 pt cap)-The short call team will admit
until 3:00 pm or until 4 patients are admitted, whichever occurs first.
Long Call-3:00pm-7:30pm-The long call team will start admitting
patients at 3:00 pm or once the short team reaches its cap of 4.
The long call interns will provide cross-cover until 7:30 pm and will
receive check-out from the other teams. One Intern from the day
team stays overnight. The second Intern from the on call team
covers from 4 pm – 7:30 pm and is relieved by the Night Float
Intern. Call will end at 7:30 pm when the night float team (1
Resident and 1 Intern) arrives.
Night Float***-7:30pm-7:30am-The night float team will admit
patients between 7:30 pm and 7:30 am. The night float intern will
provide cross-cover overnight and will receive check-out from the
long call intern who left at 7:30 pm.
***For Friday-Saturday, residents & interns on electives take call as the night float team.
Medicine consults during the evenings are taken by the night float
resident and passed to consult team in the morning.
~7~
“In the Midnight Hour”
Cross–Cover Guide for Common Problems
Encountered On-Call
This guide serves to assist you in taking care of some very common
cross-cover calls you may receive while on call. It is very important
for a physician to learn and master the skill of clinical problem
solving while on call. This is not a comprehensive guide and thus
you may need additional sources to assist you in your management
of a particular patient.
General Keys to Managing a Patient on call:
When the nurse calls you regarding a patient, always use a
pleasant tone when speaking with them, regardless of the time or
situation.
You will get the majority of the history from the patient and the
chart, so do not spend a great deal of time trying to obtain the
complete history from the nurse.
Go and see the patient before making a decision regarding his
care.
If at any time during your cross-cover call you do not know what
to do, call your resident to assist you. Remember we as physicians
are to first DO NO HARM!
Always document what you did on the chart, include the reason you
were called to see the patient, your physical exam, and your
assessment/plan.
Communicate with your resident if you plan to order further testing
or procedures. All intern procedures need to be supervised by a
resident until you have completed the requirements. Also discuss
~8~
with your resident and/or attending your management plans for the
first few months of internship, ESPECIALLY IF THE PATIENT
NEEDS TO BE TRANSFERRED.
If this is a private patient (The patient IS NOT on a medicine/ICU
team, rather his admitting physician is a private physician-at
METHODIST for example), notify the admitting physician of the
patient’s complaint and your physical evaluation. You will need to
discuss your plan with that physician prior to ordering tests,
procedures or transfers.
All patients who are to be transferred will need transfer orders.
These orders are to be written out; do not write “Continue all
previous orders and meds.”
Acute Chest Pain
The nurse calls and states that Mr. Ihurt is complaining of chest
pain
Questions to ask the nurse:
The patient’s age and reason for admission
Time, duration, and description of pain
Vital signs (include O2 sat)
Is the patient on a monitor?
Has the patient been given any medicine for the pain?
Orders for the nurse:
Place patient on a monitor (Note: The Emery House/Code
Blue carts have monitors on them if there are no floor monitors
available)
Get EKG Stat
Get PCXR (portable) stat
O2 sat if not done
~9~
O2 by nasal cannula or face mask
Cardiac enzymes (CK, Troponin)
Sublingual NTG 0.4 mg x 1 (if chest pain is persistent), make
sure BP is stable. Repeat in 2-5 minutes if needed.
ASA 325 mg if no contraindication (Bleeding, Allergy)
Inform nurse:
I will arrive in ____ minutes (Do not delay in going to see the
patient!)
Important differentials to think about on the way
Acute MI
Pulmonary Embolus
Aortic Dissection
Pleuritis/Pneumonia
Pneumothorax
Unstable/Stable Angina
Pericarditis
Gastroesophageal Reflux-GERD
Chest Wall Pain/Musculoskeletal
Herpes Zoster
Rib Fracture
Esophageal Spasm
LIFE THREATENING CAUSES OF CHEST PAIN (DON’T MISS
THESE!!)
Acute MI
Aortic Dissection
Pneumothorax
Pulmonary Embolus
~ 10 ~
Upon Arrival to floor:
Quickly that day, review the chart (PMH, medicine list, recent
procedures/tests, vitals and physical exam earlier that day, labs
earlier that day)
Evaluate the patient (location of chest pain, breathing pattern)
Review EKG, CXR , and labs( may take ½ to 1 hour, so do followup on labs)
Call and discuss your plans with your resident (especially in the
beginning of the internship year)
Decide if patient needs to be transferred to a monitored bed or ICU;
if so begin to write transfer orders and have the nurse call for a bed.
If pain not relieved by 2 nitroglycerines then review precipitating
factors. Think of adding IV Beta-blockers, IV NTG, Morphine
(especially for pulmonary edema)and/or IV Heparin.
If considering thrombolytics, you will need a cardiology consult.
Make sure you discuss with resident first.
NOTE: Call your resident +/- attending for any EKG changes,
unrelieved chest pain, and malignant arrhythmias.
Acute Shortness of Breath
The nurse calls you and states that Ms. Wheezie is complaining of
shortness of breath
Questions to ask the nurse:
The patient’s age and reason for admission
How long has the patient been short of breath
Sudden onset or gradual
Vitals sign (include O2 sat)
Is there any accompanying chest pain
What has been done so far?
~ 11 ~
Orders for the nurse:
O2 sat if not already done
Stat ABG
Stat EKG
Stat PCXR (portable)
Stat CK /Troponin I
O2 by BNC or face mask
If patient is wheezing, order stat breathing treatment (Albuterol unit
dose breathing treatment; if patient has already has already had an
albuterol treatment, consider ordering a combined
Albuterol/Atrovent 1 hour long unit dose breathing treatment)
Inform nurse:
I will arrive in ____ minutes (Do not delay in going to see the
patient!)
Important Differentials to think about on the way
Congestive Heart Failure (CHF)
Pulmonary Embolus (PE)
Pneumothorax
Asthma/ COPD Bronchospasm
Acute MI
Massive Pleural Effusion
Cardiac Tamponade
Pneumonia
Post-Op Atelectasis
Upper Airway Obstruction
Anxiety
Massive Ascites (Liver patients)
~ 12 ~
Upon Arrival to floor:
Quickly review the chart (PMH, medicine list, recent
procedures/tests {Ex. central line placement}, vitals, O2 sat, and
physical exam earlier that day, labs earlier that day, etc)
Evaluate the patient
Review EKG, CXR, ABG and labs( may take ½ to 1 hour, so followup on labs). Go and see the CXR yourself, don’t just go by the
preliminary report
Decide if patient needs airway protection/crashing, if so, call an
EMERY HOUSE/CODE BLUE.
Other options include IV Lasix if pt is CHF/volume overoloaded,
scheduled breathing treatments, 100% face mask ventilation.
Re-evaluate patient after above intervention. If patient is not
improved, decide if patient needs to be transferred to the ICU for
either Non-invasive ventilation (NIPPV) or conventional mechanical
ventilation (CMV). Remember to call your resident for any concerns
or questions. Please discuss any plans of transfer with your resident
and/or the attending
CT chest per PE protocol (make sure pt has a normal creatinine
before ordering.) If pt has renal failure, get V/Q scan instead of CT
chest. Of note, if the patient has an abnormal CXR, the V/Q scan
may not be helpful. Consider giving IVF’s with bicarbonate prior to
the CT if pt has a borderline creatinine or is a diabetic.
Note: If PE is a moderate to high probability and there are no
contraindications, consider start either Heparin or Lovenox prior to
the CT chest or V/Q scan. Decide as to whether to continue
treatment based on clinical suspicion and results of imaging studies.
Discuss your plans with the resident and/or attending prior to
ordering the above studies.
~ 13 ~
Altered Mental Status
The nurse calls and states that Mr. Bonkers is confused
Questions to ask the nurse:
The patient’s age and reason for admission
Vital signs
Is the patient a diabetic or an alcoholic?
Has the patient been recently started on new medicines
(especially in the elderly)
Any recent trauma
Orders for the nurse:
Vitals, fingerstick blood glucose, O2 sat
Inform nurse:
I will arrive in ____ minutes (Do not delay seeing the patient!)
Important differentials to think about on the way
CNS infections
Hypoglycemia/Hyperglycemia
Increased intracranial pressure
Hypoxia
Seizures
Arrhythmias
Toxins/Delirium Tremens
Metabolic (Hypercalcemia, Hyponatremia, Hypernatremia,
Metabolic Acidosis, Uremia/Renal failure)
Drugs (Think about morphine, benzodiazepines, steroids,
tricyclic antidepressants. In the elderly, do not forget aspirin,
beta-blockers, H2 Blockers, Antihistamines, Anticholinergics)
Depression/Schizophrenia
Endocrine: Hypothyroidism, hyperthyroidism, adrenal crisis
Constipation (especially in the elderly)
~ 14 ~
Upon Arrival to floor:
Quickly review the chart (PMH, medicine list, labs earlier that day,
vitals and physical exam earlier that day)
Evaluate the patient (include the neuro exam)
Consider ordering the following:
BMP, CBC, ammonia, CK, Troponin, EKG, ABG
O2 by BNC (Start with 2Liters)
EKG
Thiamine (especially if pt is alcoholic, also order before giving
glucose (D5 IVF’s, or amp of D50 )
Narcan if pt is receiving opioids
Lactulose if pt has hepatic encephalopathy or is elderly with
constipation
Amp of D50
Insulin if pt is hyperglycemic
Haldol or Ativan if pt is extremely agitated or having
hallucinations
IVF’s for metabolic & infectious causes
IV antibiotics for infection (Refer to Sanford guide)
Non-contrasted CT Head to evaluate for intracranial bleed
LP tray to bedside - especially in immunocompromised
patients (HIV, cancer)
Call your resident if LP is needed
Evaluate pt for improvement after above intervention
Decide of patient needs to remain on the floor versus being
transferred to the ICU
~ 15 ~
Fever On Call
The nurse calls and states that Mrs. Hottie is running a fever.
Questions to ask the nurse:
The patient’s age and reason for admission
How high is the temperature and which route was used to
measure the temp (Oral, Axillary, Rectal- Remember that 37°C
oral = 37.5°C rectal =36.5°C axillary)
Vital signs, include O2 sat
Is this fever new?
Is this a postoperative patient? If so, what type of surgery was
done
Orders for the nurse:
IVF’s (especially if the patient is febrile and hypotensive)
Blood cultures X 2 from 2 separate sites, 5 minutes apart. If
patient has a central line, PICC line, or Port-a-Cath, get one
set of blood cultures from the line
Urinalysis with urine culture & sensitivity (UA w/ C&S)
Inform nurse:
I will arrive in ____ minutes (Do not delay in going to see the
patient!)
Important Differentials to think about on the way
Infection (especially in HIV patients)
Pulmonary Embolism
Drug Induced Fever
Delirium Tremens (alcoholic patients)
Post-op Atelectasis
Connective Tissue Disease
Neoplasm
~ 16 ~
LIFE THREATENING CAUSES OF FEVER
(DON’T MISS THESE!!)
Septic shock
Meningitis
Upon Arrival to floor:
Quickly review the chart (PMH, medicine list, recent
procedures/tests, vitals (fever curve), O2 sat, physical exam earlier
that day, and labs that day, etc)
Evaluate the patient –complete physical exam including surgical
wounds, joints, sacral region and rectal exam. Inspect ALL IV
SITES for signs of infection. Inspect Foley catheter bag urine as
well.
Consider ordering CBC with differential, BMP, portable CXR (if pt
with pulmonary complaints-wheezing, decreased breath sounds),
sputum cultures, and LP tray to bedside if patient has signs of
meningitis. Call resident if LP is needed.
Once source of fever is identified, treat accordingly
Infection/Septic Shock- Broad spectrum antibiotics (refer to
Sanford guide and hospital biograms-a list the hospital’s antibiotic
resistance patterns). Aggressive IVF hydration. Call surgery if there
are signs of post-op wound infection.
Drug Induced Fever- Stop the offending agent
Delirium Tremens-Benzodiazepines
Tylenol (PO or Rectal)
Decide if the patient needs to be transferred to a monitored bed or
an ICU bed. IF PATIENT HAS SIGNS OF SEPTIC SHOCK,
TRANSFER THE PATIENT TO THE ICU.
~ 17 ~
Falls Out of Bed
The nurse calls and states that Mr. Ive Fallen was found on the floor
beside the bed and now needs you to evaluate him
Questions to ask the nurse:
The patient’s age and reason for admission
Did anyone witness the fall?
Is the patient injured?
What are the vitals signs, include O2 sat
Is the patient on any anticoagulants or anti-epileptics?
Orders for the nurse:
Please page me back immediately if there is a change in
consciousness before I arrive to the bedside
Inform nurse:
I will arrive in ____ minutes (Do not delay in going to see the
patient!)
Important Differentials to think about on the way
Cardiac causes: MI, Arrhythmias, Orthostatic hypotension
Vasovagal Syncope
Confusion (Could be 2° to drugs, metabolic disorders,
dementia, TIA/stroke or seizure)
Environmental hazards: wet floor, call button out of reach, lack
of assistance when transferring from bed to chair or viceversa, or a dark room
Upon Arrival to floor:
Quickly review the chart (PMH-any history of falls, medicine list,
vitals, labs, etc).
~ 18 ~
Evaluate the patient (check mental status and tilt vitals). Look for
tongue lacerations, evidence of a fracture, bruises, or hematomas.
Do a complete physical examination.
If patient is a diabetic, check fingerstick blood glucose.
If patient is on anticoagulants, check INR and PTT. If patient is on
anti-epileptics, get a drug level.
Decide on reason for fall. If possible treat the underlying cause
(holding sedatives, volume repletion for the hypovolemia, holding
oral hypoglycemics for hypoglycemia, giving additional anti-epileptic
medicine for a seizure, or turning on the light for a dim room).
Decide if any imaging is necessary (CT head for head trauma or
mental status change or X-ray for localized pain)
If patient has head/neck injury or is on anticoagulants, consider
placing these patients on frequent neuro checks (Every 1-2 hours)
If patient needs more intensive monitoring, discuss the option of
transferring the patient with your resident and/or attending.
~ 19 ~
Death Pronouncement
Identify the patient
Examine the patient
Check for verbal stimuli
Auscultate for heart sounds
Inspect for spontaneous breath sounds
Check for pulse
Check pupils for dilation
If family at bedside, express sympathy/empathy
Write the death pronouncement on the chart as follows:
Called to pronounce patient. No response to verbal or tactile
stimuli, pupils fixed and dilated, no spontaneous respirations,
no heart sounds auscultated, and no pulse. Pt pronounced
dead at _____hrs. Cause of death: Cardiopulmonary failure
secondary to underlying disease.
Consider discussing with the family and attending whether an
autopsy is needed. If autopsy is ordered, notify the nursing staff.
Write orders as follows:
Notify attending
Notify family
If no autopsy:
D/C lines/tubes/meds
D/C to morgue
After you write the orders, the nursing staff will take care of getting
the paperwork to the family, calling the tissue bank, calling the
organ donor services, etc.
~ 20 ~
Prescription Numbers:
DEA Number Your Suffix
NPI ___________________________________
Baptist Hospital AB8546004
______________
VAMC AV4580014
______________
MED AC5611000
______________
LeBonheur AL0397643
______________
Methodist AM0395168
______________
Dictation Information:
Hospital Specific Phone Number Dictation ID#
Baptist Hospital 226-5092
_______________
VAMC 523-8990 x3600
_______________
MED 205-9673
_______________
Methodist 516-7054
_______________
Regional Medical Center at Memphis (MED)
OPERATOR : 545-8400
PHONE PREFIX: 545-_______
Inpatient medicine:
5B Lo-side
57173
5C Lo-side
58150
4D MICU
58334
4D NICU
58390
Rout OB ICU 56996
5B Hi-side
5C Hi-side
4C PCU
Adams Prison
57560
58100
57060
57470
Chem
Echo
Heme
Micro
Trauma Lab
X-Ray (Trauma)
57744
448-4767
57767/56344
52178
87192
57771
Miscellaneous:
Admissions
57688
Computer Help 57480
ER MD area
57859
Interventional 57476
MMHI
524-1200
Mphs Path
405-8200
Pathology
448-6300
Psych Holding 57944
Surg B
790-9858
Bed Control
ER front desk
Health Dept:
TB
STD
Newborn Ctr
Pharmacy IP
Surg A
Trauma
57133
57826
544-7600
544-7616
544-7552
87366
57937
790-9849
57857
MedPlex Phone Numbers:
GI Lab
58311
Mammogram 5636
Lab
Pharmacy
57964
57970
Labs:
Cath Lab
CT Scan
EEG
Immunology
MRI
U/S
448-6122
58345/57294
57881
56528
58499
57281
~ 22 ~
Promark (800) 762-2299
X-Ray:U/S
57281
MED Clinics:
Adult Special Care 57446
Derm
57486
Med B
57285
Optho
57257
Ortho
57259
Sickle Cell Clinic
58535
Wound care
58999
TLC
725-7100 #3300
Allergy
Med A
Neurology
Oral Surgery
Neurosurgery
Surg/Urology/Vas
57185
57130
57285
57273
57486
57486
MED Computer:
Meditech
USERNAME: ____________________________________
PASSWORD: ____________________________________
MED Dictation:
Step 1: Dial: 205-9673
Step 2: Your Physician ID# is ________________. Enter your
5-digit ID number. (If less than 5 digits, enter your ID number
followed by the # sign).
Step 3: Enter the Service Number followed by the # sign:
1 – Surgery
9- Neurosurgery
2 – Medicine
10-Thoracic Surgery
3 – Plastic Surgery
11-Neurology
4 – ENT
12-Orthopedics
5 – Urology
13-Trauma
6 – Oral Surgery
14-Rehabilitation
~ 23 ~
7- Ophthalmology
8- Ob-Gyn
15-Newborn-Pediatric
0 – History & Physical
1 – Operative Report
2 – Discharge Summary
3 – Consult
4 – Letter
5 – Progress Note
6 – Out-Patient Note
7 – Physician Action Line
Step 5: Enter the patient’s 8-digit account number (or press # for
PAL)
Step 6: Press 2 to begin dictating. When finished, press 5 to
begin a new dictation or press 9 to obtain a job confirmation
number and disconnect. Begin dictation by stating:
Your Name
Service
Patient’s Name and Spelling
Medical Record Number
Admission and Discharge Dates
Copy Distribution
To indicate STAT dictation, press the * key any time during
dictation
Follow Touch Tone control function on last page of manual.
~ 24 ~
MED Discharge Summaries:
1) Physician’s Name
2) Patient’s Name, Age, Sex, Race
3) Unit Number, Service
4) Hospital Area
5) Date of Admission
6) Date of Discharge
7) Pertinent History
8) Pertinent Physical Findings
9) Pertinent Lab Findings
10) Hospital Course (TX, Complications)
11) Final Diagnosis (Primary, Secondary)
12) Operative Procedures
13) Instructions to Pt for future care
14) Name and Address or Fax # for copy distribution
BAPTIST MEMORIAL HOSPITAL
PHONE: 226-5000
Internal dialing use 6 as the prefix then the extension, red phones
starting with suffix 2 can only be dialed while in the hospital
Phone Numbers: (226- _ _ _ _)
Cath Lab 65196
Medical Records
CT
65159
Pathology
ER
63010
Pharmacy
GME
61350
Radiology
Hem
65647
Recovery Room
MRI
62808
X-Ray Reports: 226-3800
(push 5 for prev report)
2
~ 25 ~
65088
65600
65750
64000
65710
#
BMH Computer System:
Codes will be assigned by Gina Rogers in the Baptist GME office.
226-1350.
USERNAME: _____________________________________
PASSWORD: _____________________________________
BMH Dictation:
East: 226-5092
Step 1: Enter Doctor I.D. #
Step 2: Enter Hospital Admission Number
Step 3: Enter worktype I.D. #
0= H&P
1= OP
2= DS/Transfer
3= Consult
4= Letter
5= Cardiac Cath
6= Monroe Clinic STAT DS
7= Misc
Follow Touch Tone control function on the next page.
~ 26 ~
Generic Touch Tone Phone Functions
~ 27 ~
Campus Training Lessons
You are responsible for completing the following on-line training
modules. Modules should be completed before you start your
training or within the first month.
HIPAA Security Training
Medicare Compliance Training Lesson 1
Medicare Compliance Training Lesson 2
HIPAA Privacy Training Lesson 1
HIPAA Privacy Training Lesson 2
Sexual Harassment Avoidance Training
FERPA Training
General Store Internet Training
HIPAA Privacy Training Update 2007
Billing Compliance Update 2007
Resident Fatigue Training Module
To complete the lessons go to the University website.
http://www.uthsc.edu Click on the iLogin link on the top menu bar of
the website. Enter your User Name and Password. (UT Net ID and
Password) Open the Administration folder and then open the
Campus Training Lesson folder.
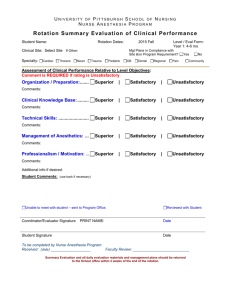
Clinical Evaluation Exercise
All PGY-1 housestaff (except preliminary) are required to perform a
minimum of five (5) Mini-Clinical Evaluation Exercises during their first
year of training. Forms are provided at the back of the guide.
~ 29 ~
An attending physician, chief resident, or senior resident can
complete the form. You may request an evaluation on any rotation
but you must include one evaluation from a general medicine ward,
medicine clinic, and the ICU or ER.
Note: It is your responsibility to ask your attending or senior resident
to complete this evaluation.
Conference Attendance
All residents are required to attend a minimum of 60% of the
housestaff noon conferences and grand rounds. The only excused
months are Night Float and MICU. Missed conferences can be made
up online. All PGY-1 categorical housestaff are required to attend a
minimum of 75% of the MedStudy conferences. A link and required
information is located on the program website.
http://www.uthsc.edu/Internal/conferences.html
Core Competencies – Competency Based Education
The following ACGME core competencies will be used to evaluate
you as a resident physician.
1.
2.
3.
4.
5.
6.
Patient Care
Medical Knowledge
Practice Based Learning and Improvement
Interpersonal and Communications Skills
Professionalism
System Based Practice
~ 30 ~
You should be able to list and define these six competencies. A very
simple breakdown is listed below. Please visit the ACGME website
at: http://www.ACGME.org for detailed information on the
competencies and various teaching methods.
Patient Care
Medical Knowledge
Practice Based Learning
Interpersonal and
Communications Skills
Professionalism
Systems Based Practice
What you do
What you know
How you get better
How you interact with other
How you act
How you work within the
system
Patient Care – demonstrate patient care that is compassionate,
appropriate, and effective for the treatment of health problems and the
promotion of health. It is the basis of our profession so all the other
competencies will improve patient care.
Medical Knowledge – demonstrate an investigatory and analyticthinking approach to clinical situations, and know and apply basic and
clinically supportive science of their discipline. The basis of physician
training which consist of specific knowledge needed to treat patients.
Practice Based Learning and Improvement – requires residents to
investigate, evaluate, and improve their patient care practices, and
appraise and assimilate scientific evidence into their practice. It is a
method to monitor, reflect, and improve performance.
Interpersonal and Communication Skills- skills that result in the
effective exchange of information and collaboration with patients, their
~ 31 ~
families, and other health professionals. One of the most important
skills a physician can master as communication problems may
negatively affect patient management and outcomes.
Professionalism – demonstrate a commitment to carrying out
professional responsibilities, adherence to ethical principles, and
sensitivity to a diverse patient population. Patients are more
compliant to treatment recommendations when they trust their
physician. Trust is large part of professionalism. You must
demonstrate, integrity, honesty, and morality in your work and daily
life.
System Based Practice – demonstrates an awareness and
responsiveness to the larger context and system of healthcare, as
well as the ability to call effectively on other resources in the system
to provide optimal healthcare. The utilization of the health care
system as a whole to provide quality care as the patient’s advocate.
Curriculum and Syllabi
Housestaff and teaching attendings must review the curriculum at the
beginning of each rotation. The review will clarify learning objectives
and competency assessment methods. The curriculum for each
rotation is listed on the website at:
http://www.uthsc.edu/internal/curriculum.html
Program goals, general objective, and progressive learning objectives
are listed at the beginning of the curriculum page.
The following syllabi require a password for access.
~ 32 ~
Ambulatory Care Syllabus – Password: Ambulatory
Consult Medicine Syllabus – Password: Consult
Ward Medicine Syllabus – Password: Ward
*Click Submit after entering the password.
Duty Hours
Duty hours must be entered into New Innovations quarterly (August,
October, January, and April) and must be completed by the 4th of the
following month. The internal medicine residency program adheres
strictly to the RRC guidelines. Duty hour rules are summarized below
and the entire policy can be viewed online at http://www.acgme.org
under resident duty hours.
one 24-hour period away from the hospital averaged over a
four week period for a minimum of four days off per four
weeks
hours are limited to 80 hours per week
10 hours off between shifts
no more than 30 continuous hours
Post-overnight call residents must leave the hospital premises
promptly at 12 pm or earlier if they started the previous day before 6
am. Teamwork is essential in order to comply with the RRC
guidelines. Following an overnight call, housestaff must not care for
any new inpatients.
NOTE:
YOUR AVAILABLE EDUCATION AND/OR TRAVEL FUNDS WILL BE
SUSPENDED/FROZEN UNTIL THE NEXT DUTY HOUR REPORTING PERIOD IF YOU
FAIL TO ENTER YOUR DUTY HOURS. IN ADDITION, YOU WILL RECEIVE A
REDUCTION IN THE AREA OF PROFESSIONALISM ON THE YEARLY AMERICAN
BOARD OF INTERNAL MEDICINE EVALUATION.
~ 33 ~
Email Policy
All residents are required to have a UT email address. You can
contact the Computer Help Desk at 448-2222 to set up your account.
Important information from the Chiefs, Program Coordinators, and
Program Director will be communicated through UT email.
Note: If you have a personal email account you may forward your UT
email to that account. If you need instructions on how to do this
contact the Computer Help Desk at 448-2222. Check you email
frequently!
Evaluation Policy
Residents will be evaluated following each rotation. Residents must
ensure the program office is provided with the correct attending
physician/supervising faculty by the 15th of each month. Upon
completion of a rotation, the program office will send evaluation forms
to the faculty member(s) who has supervised the resident during this
period. Completed evaluations will be returned to the program and will
be reviewed by the program director. The program office will verify
that all evaluation forms have been returned and assemble the
information for each resident. Each resident will also anonymously
evaluate their peers and their faculty on a monthly basis.
Constructive comments for anonymous feedback should be provided.
Each resident has an assigned faculty advisor who reviews all new
evaluations with the resident on a quarterly basis. The Faculty Advisor
Committee meets quarterly to review each resident's progress and
make suggestion for improvement.
~ 34 ~
A resident having problems will be referred to the Clinical
Competence Committee, a small group chaired by an Associate
Program Director. The committee studies the problems, contacts
residents and staff for additional insights, allows the resident to
appear before the group, and passes on its recommendations in
written form to the program director. The program director then meets
with the resident to review findings, make recommendations for
improvement, and/or reformulate goals and objectives as indicated.
The resident will be requested to sign the evaluation summary which
will then be placed in the resident's file. The resident will receive a
copy of the signed summary. Residents may review their files upon
request.
Fatigue Policy
Faculty and residents should be alert for signs of fatigue among
housestaff. These signs include falling asleep, irritability, apathy, and
careless medical errors. When faculty and residents observe these
signs, the houseofficer should be questioned about sleep loss and
fatigue. Brief counseling should be provided if a sleep deficit is
identified. This counseling may include information about naps, use of
caffeine, and good sleep hygiene. If the symptoms continue, referral
to the chief residents or program director should occur.
If the houseofficer's fatigue symptoms at any point are sufficient to
jeopardize patient care, the houseofficer or attending physician
discovering the problem should consult immediately with other
members of the team or with the chief resident or program director so
that the houseofficer may be immediately relieved of duty. Patient
care should then be delivered by other members of the team or by
~ 35 ~
another houseofficer designated by the chief residents. All
housestaff must complete the “Resident Fatigue Training Module”.
Housestaff Manual
The Housestaff Manual is located on the website at:
http://www.uthsc.edu/Internal/hmanual.pdf It is your responsibility as
a resident to read this manual.
Internal Medicine In-training Examination
The Internal Medicine In-training Examination is administered yearly
to all categorical and combined medicine/pediatric housestaff in
October for self-assessment. It is a timed national examination
consisting of two books.
Sharing of test information before, during, or after testing is prohibited
and is a violation of professionalism. Irregular or unprofessional
behavior during the exam will be reported to the testing agencies. The
Clinical Competency Committee will be convened to investigate any
irregularities and recommend appropriate disciplinary action up to and
including termination from the training program.
Internal Medicine Website
The program website located at http://www.uthsc.edu/internal is an
excellent source of information. Conferences, call schedules,
curriculum, housestaff manual, program documents and polices are
listed on the site.
~ 36 ~
Leave Policy
Paid annual leave of three (3) weeks, consisting of twenty-one (21)
days with a maximum of fifteen (15) “working days” (Monday-Friday)
plus six (6) “weekend days” (Saturday-Sunday), may be given per
twelve month period. Annual leave is granted at the discretion of the
Program Director and must be approved, in writing, by the Program
Director (or his/her designee) in advance.
**All vacation and sick days must be entered into the New Innovations
system under Duty Hours.**
You may take an extended (more than one week) vacation during
back to back electives with prior approval. However, for those
two week vacations housestaff must ensure that they are back to
work on time. For those that arrive late one extra night call will
be assigned for each day late plus one week of back-up call. A
minimum of two extra calls will be assigned.
Educational leave is granted at the discretion of the Program
Director, but may not exceed ten (10) days per twelve month
period.
Sick leave - Twenty-one (21) working days of per twelve month
period.
Maternity leave - All available sick and annual leave days up to
the maximum of six (6) paid weeks duration may be used by
female housestaff members for the birth of a child. With prior
approval, additional unpaid maternity leave may be granted by
the Program Director. Extended leave due to complications may
be covered under the resident’s disability policy after the 90 day
waiting period.
~ 37 ~
Paternity leave - 7 days with a possible extension using vacation
days. With prior approval, additional unpaid parental leave may
be granted by the Program Director.
***Due to APDIM rules, taking additional time off will delay completion
of the residency.***
Mail
Any mail received for you at the program office will be placed in a mail
slot near the program office. Journals should be mailed to your home
address not the program office. Please check for mail on a regular
basis.
Medical Records
One of the major components of “quality assurance” is timely
completion of the medical record; specifically, an appropriately
detailed discharge summary dictated on the day of the patient’s
discharge. At the time of discharge the house officer should make a
quick review of the chart and co-sign any verbal orders, consults, or
student notes. The summary should be dictated on the day of the
patient’s discharge. If this is impossible, the dictation must be done
within two weeks of discharge. If the summary has not been
completed within two weeks, it is deemed delinquent and disciplinary
action may be taken against the assigned resident. Extra guest call
may be assigned during selective/elective months and documentation
of poor professional behavior may be filed in the house officer’s
permanent GME record. Additionally, the resident may be suspended
from clinical duties until all charts are completed, which may result in
an extension of training time. Failure to complete medical records
~ 38 ~
within the allotted time has an adverse impact not only on
reimbursement for physician services but also on patient care.
Moonlighting Policy and Requirement
All moonlighting requests must be submitted and approved by the
program director. A link for requests is location at the bottom of the
training program website. Residents are not required to moonlight.
The performance of residents' moonlighting will be monitored and any
adverse effects will lead to withdrawal of permission.
PGY-1 residents may not moonlight/sunlight.
No moonlighting/sunlighting during medicine wards or any ICU
months.
No moonlighting/sunlighting pre-call, post-call or when on backup call.
During ER months, any moonlighting/sunlighting must be
separated by at least 10 hours from any ER shift.
Moonlighting/sunlighting shall not occur more frequently than
twice per week and for a maximum duration of 24 hours per
week.
Moonlighting/sunlighting cannot interfere with scheduled
afternoon or weekend rounds.
No moonlighting/sunlighting during sick leave or maternity leave.
No sunlighting during leaves of absence.
Residents who plan to moonlight outside of the system must
notify the program director of this intention in writing. They will
then need to notify the program director of the location, type and
schedule of moonlighting by the first of each month.
~ 39 ~
Any resident who wishes to moonlight on this campus (i.e. Med
ER) must obtain a signed moonlighting approval form from the
Program Director.
All moonlighting/sunlighting by residents is ultimately subject to
the program director's approval.
Moonlighting hours combined with residency work hours must
not exceed 80 hours per week when averaged over a 4 week
period.
Each resident is responsible for maintaining the appropriate state
medical license where moonlighting occurs (see GME Policy
#245 – Licensure Exemption) and separate malpractice
insurance. The Tennessee Claims Commission Act does not
cover residents who are moonlighting.
Non-teaching Patients
Housestaff are occasionally asked to render care to patients not on
the teaching service. This care must be limited to emergent situations
only with the primary physician expected to assume care
expeditiously after the housestaff are called.
Pagers
We are using Comserv Alpha Numeric Pagers. Text messages can
be sent from http://www.pagememphis.com. If your pager
malfunctions contact the program office at 448-5814 for a
replacement. There is a $75.00 charge for lost pagers and a $50
charge for pagers with damage.
~ 40 ~
Paychecks
Paychecks are received the last working day of each month. All
paychecks must be set up for direct deposit (University Policy). Direct
deposit verifications are emailed each month.
Portfolio
The Portfolio in New Innovations is to assist you with keeping a record
of scholarly activity. All residents must enter any presentations,
posters, journal club materials, abstracts, research projects, or
publications you produce.
Procedures
All residents must maintain a procedure log to comply with
specifications of the American Board of Internal Medicine (ABIM) and
the Residency Review Committee and to assist residents with
obtaining hospital privileges in the future. All procedures must be
logged into the New Innovations computerized system and confirmed
by supervising faculty.
The following is a list of required procedures:
Breast Exam (5), Rectal Exam (5), Pelvic Exam (5)
Paracentesis (3), Arthrocentesis (3), Thoracentesis (3), Lumbar
Puncture (5), Central Line (5), Arterial Blood Gas (5), and Nasogastric
Intubation (3)
~ 41 ~
Professional Conduct
House officers are expected to maintain a high level of professional
conduct. Professionalism is one of the six clinical competencies in
which residents must demonstrate proficiency in order to successfully
complete residency. Professionalism includes maintaining a
professional appearance as well as demonstrating a high standard of
moral and ethical behavior. Some examples of expected behavior that
should be maintained throughout a physician’s career are listed
below. Other examples are given in the Academic Appeals Process
section.
Communication:
• Discuss treatment plans or changes in status with patients and
families daily
• Personally call all consultants at the time the consult order is
written
• Call the patient's primary care provider upon admission and
discharge and send a copy of the discharge summary to the
physician’s office
• Discuss issues concerning patient management with fellow
colleagues personally and in a professional manner. Do not write
inflammatory or disparaging remarks about colleagues in the
chart.
• Notify the appropriate personnel including hospital paging
operators immediately about any call schedule changes
~ 42 ~
Confidentiality:
• All residents and staff must comply with federal HIPPA
guidelines. GME requires all housestaff to complete an online
course documenting knowledge of the policy.
• Respect patient privacy at all times. Avoid using patients’
names and personal information in public places. Shred all
documents with personal information, including patient census
lists.
Honesty:
• All information written in the chart must be accurate and true.
Any medical errors or adverse patient outcomes must be
documented honestly and disclosed to the patient and/or family.
• Honesty must be use when taking any program related
examination or course.
Appearance:
• Project a professional, confident, and caring image.
• Be well-groomed, professionally attired, and practice good
hygiene.
Dedication:
• Possess a sound work ethic
• Judiciously use the back-up call system
• Follow a diligent reading regimen
• Ensure proper follow-up of inpatient and outpatients
• Develop a good working relationship with colleagues and
consultants
• Teach fellow residents and medical students
• Comply with the 80 hour work week and 30 hour continuous
duty rule
~ 43 ~
Respect:
• For all hospital and UT employees regardless of position
• For all patients and their families
• Respond sensitively to patients' and co-workers culture, age,
gender, and disabilities
Research Rotation
At the end of any research rotation all residents must submit to the
program office a minimum three-page paper summarizing work
performed during that rotation. This paper must be put into resident’s
file and entered into New Innovations under the Portfolio option.
Stipend (Educational)
MedStudy books for PG1 categorical and medicine/pediatric
housestaff
UpToDate access for all residents
Pocket PC (if needed) from Graduate Medical Education office.
You will be notified when additional funds are available.
Additional funds can be used toward purchase of the following:
Medical textbooks, medical instruments, computer software, journal
subscriptions, board review books, membership dues, and exams.
All receipts must be given to the Program Coordinator, Susan
Andrews, by May 31 for reimbursement each year. Please contact her
at 448-5704 or sandrew8@uthsc.edu if you have any questions.
MedStudy DVDs, Multimedia Primary Care Procedures, and MKSAP
questions are available for checkout in the program office.
~ 44 ~
Supervision Policy
Implementation of the Resident Supervision Policy (RSP) and
Guidelines occurred October 1, 2006. They have been incorporated
into the housestaff manual and placed on the program website under
Documents and Syllabi.
1. The RSP states supervisory expectations in inpatient and
outpatient settings, for consultations, and for bedside and other
procedures. Please review the RSP carefully since resident and
attending documentation are significantly affected. Both residents and
attendings need to document their interactions on the chart. Attending
physician and resident interaction should be encouraged in all
situations.
2. For inpatient, non-critical care admissions, the admitting resident is
expected to notify the attending physician promptly (within minutes
after full patient assessment) in the following situations: a. any
questions about patient care; b. clinical instability; c. need to move to
a higher level of care; d. any major change in patient status; and e.
need to make DNR.
3. For critical care admissions, the critical care fellow (either
pulmonary or cardiology) is expected to see these patients promptly
after admission. The fellow is expected to notify his attending
physician if there are any questions about patient care.
~ 45 ~
4. For inpatient consults, the resident is expected to notify his
attending promptly in the following situations: a. any questions about
patient care; b. any patient going soon to the operating room; c.
clinical instability; d. need to move to a higher level of care; e. a
recent major change in patient status; and f. patient to be discharged
prior to attending seeing patient.
5. While attending physicians and housestaff are required to adhere
carefully to the RSP and guidelines, attending physicians may wish to
provide even closer supervision (i.e., prompt notification after every
admission and consultation). This is left to the discretion of the
attending physician.
See web page for specific information:
http://www.uthsc.edu/GME/policies/supervision_pla2008.pdf
SVMIC Conference
This is a mandatory conference that covers malpractice issues. The
State Volunteer Mutual Insurance Conference must be attended each
year. Specific dates for 2010 are September 2 & 3.
TB Testing
Residents are required to have a TB test every year. PGY-1s must
have the test done before they start training. PGY-2 and 3s can have
testing completed at University Health (448-5630), 910 Madison
Avenue, 9th Floor. TB results must be faxed to the Graduate Medical
Education Office at 448-6182.
~ 46 ~
Teaching Responsibilities
An integral part of the learning experience is the ability to teach
others. Residents in charge of a ward service are expected to
present at least one oral presentation weekly to the interns and
students on the service. Additional bedside teaching is expected as
part of the daily ward activity.
Travel to Meetings
Approval for travel to meetings is contingent upon the requirements
listed below.
An Internal Medicine Travel Request Form MUST be
completed for travel to meetings and submitted to the Program
Coordinator four (4) weeks before the meeting.
No more than eight (8) residents will be allowed to attend the
same meeting. Permission to attend will be given on a first
come-first served basis.
The abstract(s) must be submitted to the Program Director for
approval before submission to the meeting.
You must be the 1st author or presenting because the 1st
author cannot attend the meeting.
All requirements must be met to receive approval. No exception will
be made.
Publications and presentations must be entered into the New
Innovations Portfolio.
~ 47 ~
Internal Medicine Travel Request Form (program website)
If travel funds are available, the training program will provide support
for one (1) Regional, State, or National meeting.
If support funds are provided, the program will pay for one
(1) poster.
The poster MUST be made at the UT Print Shop.
A GME Travel Form must be reviewed and signed by the Program
Coordinator then submitted with a meeting brochure and original
receipts to Lisa Shinall in the Graduate Medical Education Office
when you return from your meeting for travel reimbursement to be
processed.
To ensure you have the required documentation necessary for
reimbursement, review (and perhaps take with you) the GME Travel
Reimbursement form before leaving on your trip.
GME Travel Reimbursement Form
(http://www.uthsc.edu/GME/policies/travel.pdf)
~ 48 ~
Mini-Clinical Evaluation Exercise (CEX)
Evaluator: __________________________ Date: ______________
Resident: ___________________________
Setting:
Ambulatory
In-patient
R1
ED
R2
R3
Other
Medical Interviewing Skill
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Physical Examination
1
2
3
|
Unsatisfactory
|
7
8
9
Superior
Humanistic Qualities/Professionalism
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Clinical Judgment
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
Counseling Skills
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
4
5
6
Satisfactory
|
7
8
9
Superior
Organization/Efficiency
1
2
3
|
Unsatisfactory
4
5
6
Satisfactory
Overall Clinical Competence
1
2
3
|
4
5
6
|
7
8
9
Unsatisfactory
Satisfactory
Superior
___________________________________________________________
___________________________________________________________
___________________________________________________________
Resident Signature
Evaluator Signature
Mini-Clinical Evaluation Exercise (CEX)
Evaluator: __________________________ Date: ______________
Resident: ___________________________
Setting:
Ambulatory
In-patient
R1
ED
R2
R3
Other
Medical Interviewing Skill
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Physical Examination
1
2
3
|
Unsatisfactory
|
7
8
9
Superior
Humanistic Qualities/Professionalism
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Clinical Judgment
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
Counseling Skills
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
4
5
6
Satisfactory
|
7
8
9
Superior
Organization/Efficiency
1
2
3
|
Unsatisfactory
4
5
6
Satisfactory
Overall Clinical Competence
1
2
3
|
4
5
6
|
7
8
9
Unsatisfactory
Satisfactory
Superior
___________________________________________________________
___________________________________________________________
___________________________________________________________
Resident Signature
Evaluator Signature
~ 50 ~
Mini-Clinical Evaluation Exercise (CEX)
Evaluator: __________________________ Date: ______________
Resident: ___________________________
Setting:
Ambulatory
In-patient
R1
ED
R2
R3
Other
Medical Interviewing Skill
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Physical Examination
1
2
3
|
Unsatisfactory
|
7
8
9
Superior
Humanistic Qualities/Professionalism
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Clinical Judgment
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
Counseling Skills
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
4
5
6
Satisfactory
|
7
8
9
Superior
Organization/Efficiency
1
2
3
|
Unsatisfactory
4
5
6
Satisfactory
Overall Clinical Competence
1
2
3
|
4
5
6
|
7
8
9
Unsatisfactory
Satisfactory
Superior
___________________________________________________________
___________________________________________________________
___________________________________________________________
Resident Signature
Evaluator Signature
~ 51 ~
Mini-Clinical Evaluation Exercise (CEX)
Evaluator: __________________________ Date: ______________
Resident: ___________________________
Setting:
Ambulatory
In-patient
R1
ED
R2
R3
Other
Medical Interviewing Skill
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Physical Examination
1
2
3
|
Unsatisfactory
|
7
8
9
Superior
Humanistic Qualities/Professionalism
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Clinical Judgment
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
Counseling Skills
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
4
5
6
Satisfactory
|
7
8
9
Superior
Organization/Efficiency
1
2
3
|
Unsatisfactory
4
5
6
Satisfactory
Overall Clinical Competence
1
2
3
|
4
5
6
|
7
8
9
Unsatisfactory
Satisfactory
Superior
___________________________________________________________
___________________________________________________________
___________________________________________________________
Resident Signature
Evaluator Signature
~ 52 ~
Mini-Clinical Evaluation Exercise (CEX)
Evaluator: __________________________ Date: ______________
Resident: ___________________________
Setting:
Ambulatory
In-patient
R1
ED
R2
R3
Other
Medical Interviewing Skill
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Physical Examination
1
2
3
|
Unsatisfactory
|
7
8
9
Superior
Humanistic Qualities/Professionalism
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Clinical Judgment
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
Counseling Skills
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
4
5
6
Satisfactory
|
7
8
9
Superior
Organization/Efficiency
1
2
3
|
Unsatisfactory
4
5
6
Satisfactory
Overall Clinical Competence
1
2
3
|
4
5
6
|
7
8
9
Unsatisfactory
Satisfactory
Superior
___________________________________________________________
___________________________________________________________
___________________________________________________________
Resident Signature
Evaluator Signature
~ 53 ~
Mini-Clinical Evaluation Exercise (CEX)
Evaluator: __________________________ Date: ______________
Resident: ___________________________
Setting:
Ambulatory
In-patient
R1
ED
R2
R3
Other
Medical Interviewing Skill
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Physical Examination
1
2
3
|
Unsatisfactory
|
7
8
9
Superior
Humanistic Qualities/Professionalism
1
2
3
|
4
5
6
Unsatisfactory
Satisfactory
|
7
8
9
Superior
Clinical Judgment
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
Counseling Skills
1
2
3
Unsatisfactory
|
4
5
6
Satisfactory
|
7
8
9
Superior
4
5
6
Satisfactory
|
7
8
9
Superior
Organization/Efficiency
1
2
3
|
Unsatisfactory
4
5
6
Satisfactory
Overall Clinical Competence
1
2
3
|
4
5
6
|
7
8
9
Unsatisfactory
Satisfactory
Superior
___________________________________________________________
___________________________________________________________
___________________________________________________________
Resident Signature
Evaluator Signature
~ 54 ~
~ 57 ~