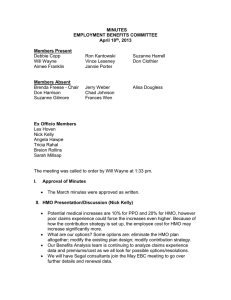
Managed Care: Present and Future
advertisement

Managed Care: Present and Future Robert (James) Walling, MRH&T James B. Connor, Pricewaterhouse Coopers James W Macdonald, Reliance Reinsurance Corp. Managed Care: A Brief Look at the Past Robert J. Walling, Consulting Actuary Miller, Rapp, Herbers, & Terry, Inc. Why look at “Ancient History” Those who cannot remember the past are condemned to repeat it. —George Santayana That men do not learn very much from the lessons of history is the most important of all the lessons of history. —Aldous Huxley Ancient History 1 1910 – First prepaid group practice (50¢ /member/mo) – First group health policy issued to Montgomery Ward 1917 – Early medical society opposition to managed care begins as Pierce County Service Bureau is formed to limit competition from prepaid plans. 1929: Depression & Managed Care Decreased philanthropic support of hospitals Substantial medical inflation Decreased hospital occupancy First prepaid hospital (Dallas Schools & Baylor University Hospital) The Ross-Loos service clinic establishes prepaid clinic in L.A. for Power and Water Departments Backlash 1931 - Ross & Loos expelled from L.A. County Medical Society 1932 - AMA Publishes a strong statement opposing prepaid medical. 1932 - Blue Cross developed (medical community responded more favorably to health insurance than prepaid medical) Development Despite Opposition 1937 - First Urban HMO established (Group Health Associates in D.C.) 1937 - Henry Kaiser begins Permanente Plans as prepaid medical plan for workers on Grand Coulee Dam construction site. Judicial Developments 1941 - U.S. Supreme Court finds D.C. Medical Society guilty of Restraint of Trade against Group Health Associates Several court successes for HMOs follow. (Shadid v. Oklahoma Medical Society) Over the next 10 years, 100 rural group health plans, 20 HMOs, and prepaid group health plans for several local unions (Teamsters, UAW, UMW) develop. Social/Political Changes 1965 - Social Security expanded to include medical insurance for the elderly (Medicare) and poor (Medicaid) 1970 - Nixon responds to $85B in US Health expenditures by endorsing HMOs as new national health strategy 1973 - HMO Act signed by Nixon. Provides for “assistance and encouragement for the establishment and expansion of HMOs” Economic Changes 1975-84 - Hospital charges inflated at average of 9.3% 1970-90 US Health expenditures rise from $85B to $647B 1990 - Health Expenditures 12% of GDP. Economic Changes (cont.) Dramatic increase in medical malpractice costs Dramatic advances in medical technology (CAT scans, MRI, Organ transplants, etc.) revolutionize medical care but at a substantial cost A number of social factors (aging population, more doctors, new techniques, relatively low employee costs) increase utilization. Number of HMOs 1950 - 20 1970 - 37 in 14 states 1975 - 183 in 32 states (297 more in planning) 1980 - 236 HMOs serving 9.1 million members 1985 - 393 HMOs 1987 - 662 HMOs Early Cost Containment Efforts Controlling Utilization – Utilization Review – Weekend Admissions – Maternity Length of Stay – Preadmission review – Second Surgical Opinion – Case Management – Appropriate Level of Care – Pre-admission Review Early Cost Containment Efforts Employee Contributions Reducing Plan Benefits – Deductibles – Copayments – Maximums (Mental Health, Private Rooms, Chemical Dependency, DME, Physical Therapy) – Outpatient Incentives Provider Network Discounts Backlash Revisited 1996 - Over 1,100 bills considered in 46 states to regulate managed care. 1997 - President Clinton appoints advisory panel to draft bill of rights for health care consumers. 1997 - In the first 4 months, 800 proposals to regulate managed care are introduced in 49 states. Managed Care: Present & Future Jim Conner Pricewaterhouse Coopers Managed Care - Overview Current Environment – Trend Issues – Overview Growth Prices Medical Care Costs Margins Mergers Quality of Care Member Satisfaction Government Programs Computer Systems Regulatory National Employee Health Care Enrollment 1993 1997 1998 Change 1993 to 1998 Indemnity 48% 15% 13% -35 PPO 27% 35% 40% +13 POS 7% HMO 19% 53% 20% 30% 85% 20% 27% 87% +13 +8 Overview - HMO Results 1990 1994 1996 1997 # Members 36.5 mil 51.1 mil 64 Mil 64 mil Growth Rate 5% 13% 19% 0% Penetration 15% 20% 24% 24% Margin 4.6% 4.7% 2.0% -0.5% HMO RATE INCREASE 9 8.3 8 7 6 4.6 5 4 Projected Actual 3.3 2.6 3 2.1 2 1 0.8 0.5 0 1996 1997 1998 Sources: Sherlock Co. (Projected); KPMG Peat Marwick (Actural) 1999 Managed Care - Growth Penetration/Growth Rate Control Risk Underwriting Risk Provider Contracting Leverage Managed Care - Prices Price Changes Market Share Driven Employer Leveraged Expectations of Managed Care Purchasing Coalitions Underwriting Cycle Managed Care - Medical Care Costs Utilization vs. Inflation Aging Population Disease Management Capitation/Risk Sharing Pharmacy Costs Complementary & Alternative Medicine (CAM) Managed Care - Margins Digesting Acquisitions Computer Capacity Rising Medical Costs Building Market Share Managed Care - Quality of Care Clinical vs. Administrative Accreditation (NCQA) HEDIS Reporting Quality vs. Cost Managed Care - Member Satisfaction Choice of Provider Point of Service/Open Access Products Availability of Provider Managed Care Government Programs Medicare Risk Medicare + Choice Medicaid Managed Care - Computer Systems Information Driven Business Capacity Medical Management Integrated Healthcare Systems Dynamic Industry Managed Care Pricing Components Pricing Grid Medical Service Categories 20 - 30 Diagnostic Related Groups (DRG) 495 Procedure Codes (CPT) 1,000+ Diagnostic Codes (ICD9) 1,000+ Managed Care -Regulatory Consumer Protection Legislation – – – – – Emergency Care External Appeals Access to Specialists Continuity of Care Right to Sue Health Plan Medicare Reform – Medicare & Choice – Outpatient Drugs Medical Record Privacy – Consent Issue – Genetic Data Uninsured (45 Million) MANAGED CARE MANAGED HEALTH Future of Managed Care: The Only Certainty is (Much) More Change James W Macdonald, Senior Vice President Reliance Reinsurance Corp. Important recent developments most likely to define the future of Managed Care Consumer Choice is returning rapidly Number of Operating HMOs Dramatic Growth Since 1993 800 750 700 650 600 550 1997 1996 1995 1994 1993 1992 1991 1990 1989 1988 500 Source: Hoechst Marion Roussel Managed Care Digest 1998; SMG Marketing Group Total Enrollment Approached 84 Million In 1997 85 75 65 55 45 35 1997 1996 1995 1994 1993 1992 1991 1990 1989 1988 25 Decentralized Models are #1: Over 70% of 1997 HMO Enrollees were in Network or IPA model plans 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% Staff Group Network IPA 1995 1996 1997 4.3 16.2 8.9 38 4.2 19.5 8.4 45.2 3 19.8 14.2 46.7 IPA Model HMOs Not Penalizing Physicians for Certain Practices Increased From 49% in 1996 to 74.1% in 1997 75.00% 65.00% 55.00% 45.00% 35.00% IPA HMOs 1996 49.00% 1997 73.90% HMO Capitated contracts with Specialists Declined in 1997 44.0% 43.0% 42.0% 41.0% 40.0% 39.0% 38.0% Specialists with Captiated Contracts 1996 1997 43.2% 40.3% Primary Care Physicians also saw a reduction in Capitated Contracts in 1997 77.0% 75.0% 73.0% 71.0% 69.0% 67.0% 65.0% PCP's with HMO Captiated Contracts 1996 1997 75.0% 70.7% Triple-Option HMO plans Jump to over 41% of all HMO plans 42.0% 40.0% 38.0% 36.0% 34.0% 32.0% 30.0% HMO Plans Offering Triple Options 1996 1997 33.9% 41.4% Note: Triple Option plans give enrollees choice of HMO, PPO or indemnity. Important recent developments most likely to define the future of Managed Care Consumer Choice is returning rapidly The Cost of Health Care will Re-Accelerate Health Care Expenditures as a Percent of GDP - New Growth Expected (Selected Years to 2007) 19 17 15 13 11 9 7 5 1970 1980 1990 1993 1996 1998e 2001e Sources: HCFA, Office of the Actuary; US Department of Commerce, Bureau of Economic Analysis 2007e Private Sector Expected to assume Burden of Increased Expenditures ($B)... 1200 1100 1000 900 800 700 600 500 400 300 200 1990 1993 1996 1998e 2001e 2007e Pub lic Sector 284.4 389 483.1 540.4 637.4 987.4 Private Sector 415.1 505.9 552 606.4 746.6 1145.9 …with the average annual Private Funds growth rate more than doubling from 1996 to 2001 12 11 10 9 8 7 6 5 4 3 2 1990 1993 1996 1998e 2001e 2007e Pub lic Sector 10.5 11 7.5 5.8 5.7 7.6 Private Sector 11.3 6.8 2.9 4.8 7.2 7.4 …But widespread double-digit growth rates are not expected to return (Average Annual Growth Rate From Prior Year Shown)... 30 25 20 15 10 5 0 1970-1980 1993-1996 2001-2007 National Health Expend. 12.9 5 7.5 Hospital care 13.9 4.9 6.6 Physician services 12.8 3.5 7.8 Other professional 16.3 7.8 8.1 Home health care 26.9 9.7 8 Prescription Drugs 8.2 7.6 9.8 Two assumptions critical to these projections ... Cost savings produced by Managed Care are “primarily one-time” and are not sustainable. Only a small long term growth rate reduction will result from the impact of managed care on the use of higher cost medical technology. Important recent developments most likely to define the future of Managed Care Consumer Choice is returning rapidly The Cost of Health Care will ReAccelerate Vertical Integration will become as much a change driver as Horizontal Integration Horizontal Consolidation: The nation’s 25 largest HMO’s enrolled 25.4 million members, or 30.3% of the total versus 23.7 million in 1996. Top 25 HMOs 30% All Other 70% Vertical Consolidation: Hospitals are forming and taking increased equity stakes in HMOs 65 60 55 50 45 40 Hospital-Owned HMOs 1995 1996 1997 46 58 61 Source: SMG Marketing Group Vertical Consolidation: Hospital-Owned Enrollment Growth Possible Key Indicator to Future of Managed Care 4200 3700 3200 2700 2200 Hospital-Owned HMO Emrollment (000s) 1995 1996 1997 2,448 2959.8 4082.1 Source: SMG Marketing Group Vertical Consolidation: Hospitals with an HMO equity stake averaged 72% occupancy versus 46% for hospitals with no HMO equity 70% 60% 50% 40% 30% 1997 Hospitals with HMO equity 72% Hospitals Without HMO equity 46% Vertical Consolidation: Pharmaceutical Segment Top Down: Merck / Medco Bottom Up: Rite Aid / PCS Mixed Segments: McKesson / HBOC Important recent developments most likely to define the future of Managed Care Consumer Choice is returning rapidly The Cost of Health Care will ReAccelerate Vertical Integration will become as much a change driver as Horizontal Integration Future of Managed Care / Health Care Free Market Ideal: Three Phases to Market Evolution Phase 1: Phase 2: National expansion & share consolidation Market Segmentation HMO Customers Segment1 Segment 2 Segment 3 Source: Andersen Consulting Three Phases to Market Evolution: Phase: 3 Outcomes Based Product & Service Differentiation “...universally accepted quality standards and measurement capabilities…” Source: Andersen Consulting Conclusion: Past Key Health Care Issues Remain Unresolved ... Aging Baby Boomers (should drive medicare Managed Care Growth) Uninsured & Underinsured Americans Solvency of Medicare / Medicaid Highest Health Care % of GDP High Cost of New Technology Need for highly informed patient / consumer (“Demand Management”) … while several tough issues have emerged today... Demonization of Managed Care Probable loss of ERISA protection Patient Distrust of For-Profit Providers Failure of PPMC model: Physicians in disarray New and tougher regulatory environment … and new important challenges appear to be on the horizon. End of low cost malpractice and E&O Insurance? Payer Dis-intermediation: Large Employer Direct Contracting (e.g. John Deere)? Impact of BBA of 1997 prospective payment system Conclusion: Follow the Money Two Possible Long Term Scenarios Decentralized, regional payer and provider system – Can consumer bear increased cost? – Can investors achieve adequate ROI? If not, probable alternative: centralized, single or limited payer system – Strictly tiered, government controlled – Similar to British or Canadian systems Conclusion: Most Likely Scenario “Tiers - R - Us” Elite Elite Secure Middle Market Vulnerable Middle Market Safety Net Safety Net 1980 1990 Elite Upscale Managed Care Low-End Managed Care Safety Net 2000+ Q&A