OECD Health Committee Survey on Health Systems Characteristics P
advertisement
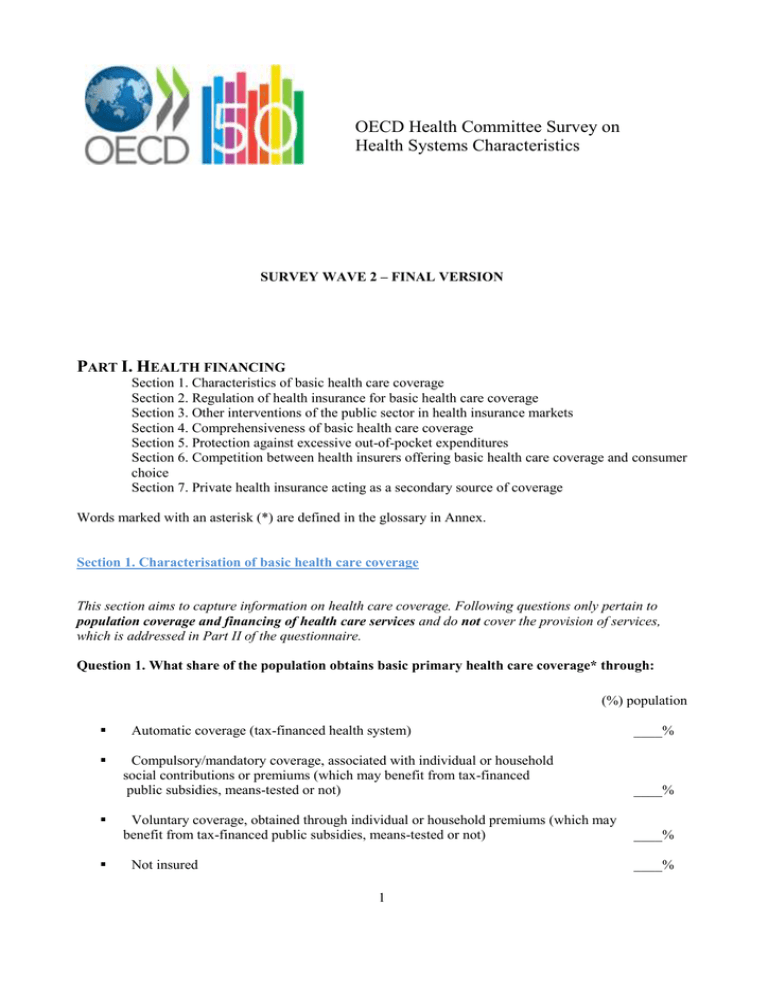
OECD Health Committee Survey on Health Systems Characteristics SURVEY WAVE 2 – FINAL VERSION PART I. HEALTH FINANCING Section 1. Characteristics of basic health care coverage Section 2. Regulation of health insurance for basic health care coverage Section 3. Other interventions of the public sector in health insurance markets Section 4. Comprehensiveness of basic health care coverage Section 5. Protection against excessive out-of-pocket expenditures Section 6. Competition between health insurers offering basic health care coverage and consumer choice Section 7. Private health insurance acting as a secondary source of coverage Words marked with an asterisk (*) are defined in the glossary in Annex. Section 1. Characterisation of basic health care coverage This section aims to capture information on health care coverage. Following questions only pertain to population coverage and financing of health care services and do not cover the provision of services, which is addressed in Part II of the questionnaire. Question 1. What share of the population obtains basic primary health care coverage* through: (%) population Automatic coverage (tax-financed health system) ____% Compulsory/mandatory coverage, associated with individual or household social contributions or premiums (which may benefit from tax-financed public subsidies, means-tested or not) ____% Voluntary coverage, obtained through individual or household premiums (which may benefit from tax-financed public subsidies, means-tested or not) ____% Not insured ____% 1 Comments/clarifications (if any): Question 2. What is the main source of basic health care coverage in your country? (i.e. which covers the largest share of the population) A national health system covering the country as a whole Local health systems that serve distinct geographic regions A common health insurance scheme (single-payer model) Multiple insurance funds (if multiple) Question b. (continued). For multiple insurance funds, how is affiliation with a particular insurer determined? Affiliation to a specific insurance/fund is not a matter of choice; it is linked to professional status, geographic situation, or employer. Affiliation is a matter of choice; people can choose among several insurers/funds. Comments/clarifications (if any): Countries with national health services will be directed to section 4, Question 12. Section 2. Regulation of health insurance markets for basic health care coverage The following questions apply only to those countries featuring multiple insurers/funds. For questions 39 below: if a system has multiple coverage schemes (e.g., both social insurance and voluntary insurance providing basic health care coverage), the response should refer to the scheme under which the greatest number of people are covered. Question 3. Are insurers/funds required to offer the same coverage/products? They are required to offer the same benefit package with the same level of coverage / copayment. They are required to offer the same benefit package but can differentiate the level of coverage (level and/or type of cost sharing). They are allowed to differentiate the benefit package but a “minimum benefit” is defined. They define freely the benefits they cover and the level of coverage. Comments/clarifications (if any): Question 4. Are premiums/contributions regulated by the government or the parliament? Contributions/ premiums are defined by regulation with no possible variations at the scheme/fund level. Contributions/ premiums are defined by regulation with some (rather marginal) variations permitted at the scheme/fund level. Schemes/funds can define contributions/premiums within regulatory constraints. If so, insurers are allowed to modulate premiums according to (check all that apply): age gender health status benefit design geographic area (e.g. region, canton) income other, explain Schemes/funds can define contributions/premiums without any regulatory constraint. Comments/clarifications (if any): Question 5. Is there any system of risk-equalisation between health insurers/funds? Yes If so, what are the main risk factors used in adjustment? (Check all that apply.) age gender health status (e.g. prevalence of specific diseases generating higher costs in the insured population) prior utilisation of services other (please specify) No Comments/clarifications (if any): The following questions only apply to those systems with multiple insurers/funds and choice of affiliation. Question 6. Restrictions and constraints on enrolment and contract renewal a. Are health insurers/funds required to enrol any applicant? Yes No Comments/clarifications (if any): b. Are health insurers/funds required to accept contract renewal for people they cover? Yes No Comments/clarifications (if needed): c. Are there constraints on premium increases in the case of contract renewal? Yes 3 No Comments/clarifications (if any): Question 7. Are there restrictions on switching? People are allowed to switch insurers at any time. People are allowed to switch at set times/frequencies (annually, quarterly) Comments/clarifications (if any): Question 8.a. What kind of information is available to individuals who are choosing among alternative health insurers/funds (check all that apply)? Information on premiums/ contributions Information on benefits covered Information on performance (e.g. claim processing time, client responsiveness) No Information Comments/clarifications (if any): Question 8.b. Is this information disclosed by (check all that apply): Individual funds Private organizations which publish comparative standardized information on health insurance funds Public authorities which publish comparative standardized information on health insurance funds Comments/clarifications (if any): Question 9. What share of the population (out of the total insured population) have switched insurer in 2011 (or nearest year for which information is available)? ____(%) Comments/clarifications (if any): Question 10. What happens if a health insurer goes bankrupt? Please explain in plain text: _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ _____________________________________________________________________________________ Section 3. Other interventions of the public sector in the health insurance market The following questions do not apply to systems with a national health service model of coverage. Question 11. Does the government intervene to ensure the provision of basic primary health coverage or health care services for low-income or economically disadvantaged groups? No Yes If so, how does the government intervene? (Check all that apply.) There are public subsidies (direct subsidy, tax credit or other tax incentives) for the purchase of basic health insurance. If so, is the level of the subsidy: Flat (the same for all beneficiaries) Means-tested What is the share of the population eligible for such subsidies? ___% What is the share of the population with effective take-up of subsidies? ____% People are entitled to health coverage through dedicated public programmes that subsidise public or private provision. If so, what is the share of the population entitled to such health care coverage through dedicated public health programmes? ____% The public sector directly provides health care services to the poorest part of the population. If so, what share of the population uses publically provided health care services? ____(%) Comments/clarifications (if any): Question 12. Does the government intervene to ensure the provision of basic primary coverage or ensure the provision of health care services to high-risk groups (seniors, disabled, people with chronic disease, etc.) ? No Yes If so, how does the government intervene in the provision of services to high-risk groups? (Check all that apply) The government regulates premiums to promote access to insurance for high-risk groups (e.g., community rating). The government subsidises (via direct subsidy, tax credit or other tax incentive) the purchase of basic health insurance. High-risk people are entitled to public health coverage through dedicated programmes that subsidise public or private provision. 5 The public sector directly provides free health care services to high-risk people. (Please specify.) Comments/clarifications (if any): Section 4. Comprehensiveness of basic health care coverage Section 4 aims to assess the level of basic health care coverage to which “typical” working-age adults are entitled to. Responses should not consider children, seniors and other categories of population which may be entitiled to higher levels of benefits (e.g. people with serious illnesses). In countries with multiple insurers allowed to offer different levels of benefits, responses should refer to the most frequent or most typical situation (see exemples below). Question 13. Is there a general deductible* that must be met before basic health coverage pays a share of the cost or the full cost of covered services? Yes If so, what is the amount of the deductible that must be met before basic primary health coverage pays/reimburses? (national currency units) ______ What is the period in which the deductible applies (e.g. year, lifetime, episode of illness, etc.)? No Comments/clarifications (if any): Question 14. Are patients required to share the costs of health care for the services and goods listed below? Please indicate the type and level of cost-sharing left at the charge of users by basic primary health coverage, in the case of an adult with no specific exemption of user charge. If there is no cost-sharing, please indicate "no cost-sharing". Please refer to the glossary for standard terminology relating to cost-sharing requirements (deductible, co-insurance and copayments). You may wish to refer to the System of Health Accounts Manual to obtain more information about the content of each category (see SHA classification of functions: http://www.oecd.org/document/8/0,3746,en_2649_37407_2742536_1_1_1_37407,00.html Types and level of cost-sharing requirements for an adult not subject to any specific exemption rule Acute inpatient care Examples: - Free at the point of care; - €15/day, capped to €X or Y days; - max (20% cost-sharing; copayment per day) - Free at the point of care for patients treated as public patients in public hospitals but cost-sharing of x% + potential extra-billing for “private patients” in public or private hospitals. - Not reimbursed if private hospital Outpatient primary Examples: care physician* - Free at the point of care; contacts - Copayment of €2 per visit; - Copayment of €10 for the first of each semester; - Co-insurance of 20%; - Not reimbursed if not referred Outpatient contacts Clinical tests Diagnostic specialist Examples: - Free at the point of care; - Co-insurance of: 30% if referred by a primary care doctor, otherwise: 50% + potential extra-billing - Copayment of €10 if not referred by a primary care doctor laboratory Examples: - Free at the point of care; - Co-insurance of 20% capped at €X; imaging Examples: - Free at the point of care; - Co-insurance of 20% capped €X; - Copayment of €18 for any test exceeding €91 + co-insurance of 30% Physiotherapist services Examples: - Free at the point of care; - Co-insurance of 20% capped €X; Pharmaceuticals Examples: - Copayment per prescription item ($5 for generics and $20-25 for brandname drugs); - Cost-sharing: 10% of cost with a min of €5 and a max of 10€ per item; - Cost-sharing of 0%, 35%, 65% or 85% depending on drug category + €0.50 per item - Deductible of SEK 900 beyond which cost-sharing diminishes by step as spending increases (from 50%, 25%, 10% and 0%). - Any difference between actual price and reference price for medicines subject to reference price Eyeglasses and/or Examples: contact lenses - 25% of costs, capped to one pair of glasses every two year. - Not covered Dental care Examples: - Not covered - Cost-sharing: 65% of costs Dental prostheses Examples: - Not covered - Cost-sharing: 65% of costs - Any difference between price and reference price Long term care Examples: 7 - Not covered - Nursing care at home with cost-sharing - Nursing care in institutions outside hospital with cost-sharing Comments/clarifications (if any): Section 5. Protection against excessive out-of-pocket expenditures Question 15. For ambulatory care (doctors visits), do people usually: Please indicate the most frequent situation Receive free services at the point of care Pay only user fees or copayments (where applicable). Pay the full cost of health services and get reimbursed for covered services afterwards. Comments/clarifications (if any): Question 16. Are there partial or total exemptions from copayments for some segments of the population? For those with certain Ye medical conditions or s disabilities No For those whose income are Y under designated thresholds es N o For beneficiaries of social Y benefits es N o For seniors Y es N o LTC Dental prostheses Dental care and/or Eyeglasses contact lenses Pharmaceuticals Physiotherapist services Diagnostic imaging Clinical laboratory tests specialist Outpatient contacts Outpatient primary care physician* contacts Acute inpatient care ARE THERE EXEMPTIONS ? If there are any types of exemptions, please specify by type of services For children Y es N o For pregnant women Y es N o For those who have reached an upper limit (or cap) for es out-of-pocket payments o Others (please specify in comments/clarifications) Y N Comments/clarifications: Question 17. Are there special tax treatments (e.g., credits, deductions) for households’ qualified health or medical expenditures (e.g., insurance premiums, out-of-pocket expenditures)? Yes No Comments/clarifications (if any): Question 18. What was the share of households exposed to catastrophic health expenditures* in 2010 or last available year? _______(%) Comments/clarifications (if any): Question 19. Do exemption mechanisms most often: Prevent people from paying copayments at the point of service? Reimburse or refund copayments afterwards (e.g., through tax credits)? Comments/clarifications (if any): Section 6. Competition between health insurers offering basic health care coverage and consumer choice The following questions apply only to those countries featuring multiple insurers/funds in competition. Question 20. A typical insurance customer has how many choices of health insurance plans? 1-2 9 3-5 more than 5 Comments/clarifications (if any): Question 21. What is the share of the basic health insurance market covered by: % market % population the top insurance company/fund? the top 3 insurance companies/funds? the top 5 insurance companies/funds? the top 10 insurance companies/funds? Comments/clarifications (if any): Question 22. What share of the market (% of covered population) is insured by: % market % pop covered Not-for-profit insurers (public or private) Private for-profit insurers Comments/clarifications (if any): Question 23. Relations between health insurers and insured people. Are health insurers allowed to: (check all that apply) Require prior authorisation for certain services in order for them to be reimbursed Offer insurance plans with a restricted network of providers If so, what percentage of insured persons are enrolled in restricted network plans? ___ % Offer insurance plans requiring patients to follow specific care pathways (gatekeeping, disease management, etc…) If so, what percentage of insured persons are enrolled in managed care plans? _____% Offer several options of cost sharing levels in exchange for higher or lower premium If so, what percentage of insurers offer such options? (%) _____% Offer financial rewards (bonuses) to insured persons who do not claim any reimbursements within a given period of time? Comments/clarifications (if any): Section 7. Private health insurance acting as a secondary source of coverage While SHA and OECD health data already include data on PHI contribution to the financing of health care services (by function of care) and on the percentage of people covered by secondary health insurance, this section aims to collect updated information on the role and scope of private health insurance acting as a secondary source of coverage (complementary, supplementary or duplicative). Question 24a. Does private health insurance provide a secondary source of coverage? Yes No Comments/clarifications: Question 24b. What are the main areas of interventions of secondary private health insurance (PHI) in your country? This represents a significant share of secondary PHI activities This represents a PHI is not more marginal allowed to share of cover this. secondary PHI activities PHI is allowed to cover this but generally does not. It covers health goods and services that are not included in the basic benefit package*, please specify (e.g. dental care, eyeglasses, pharmaceuticals…) It covers cost-sharing for health goods and services covered by basic primary coverage scheme(s). It covers health goods and services included in the basic benefit package* (duplicate cover): i. Only when provided by providers whose services are not eligible for funding by basic primary coverage ii. Including when provided by providers whose services are eligible for funding by basic primary health coverage (e.g. to jump the queue or choose your doctor). Question 25. If you responded that there is any duplicate cover in question 24, what does duplicative coverage most often allow? 11 Coverage for enhanced non-medical accommodation services (e.g. private rooms in hospitals, a television etc) Expands the choice of providers Quicker access to health care Choice of doctor Lower co-payments Financial benefits through the tax system PART II. HEALTH CARE DELIVERY This part of the questionnaire on health care delivery contains eight sections from provision of health care to user choice and coordination and continuity of care. Section 1. Provision of health care and payment of health services Section 2a. Status and payment of health care professionals Section 2b. Special focus on pay-for-performance Section 3. User choice and competition among providers Section 4. Workforce training and regulation Section 5. Regulation of medical equipement Section 6. Regulation of prices/fees Section 7. Regulation/monitoring of health providers activity Section 8. Co-ordination and continuity of care A glossary of terms is available on the introductory web page of the questionnaire http://www.oecd.org/health/HSCsurvey. Words marked with an asterisk (*) are defined in this glossary. Section 1. Provision of health care and payment of health services This section aims to describe the status and types of organisations delivering health care services as well as their mode of payments. Status and remuneration of individual health professionals are addressed in the following section. Since health care services can be financed through several routes and with different payment methods, the questionnaire will focus on payment methods employed by the key “purchasers” for each category of services, as identified in the table below. “Purchasers” refer to financing agents as defined in the System of Health Account, i.e. the “final payers”. Depending on the country and type of service, purchasers either pay directly the provider or reimburse the patient after he/she receives care. Question 26. Who are the key purchasers of health services? For each column (i-iv), check all that apply Types of care i. Acute Ambulatory / outpatient inpatient Care care iii. Primary ii. Specialist/ care services Diagnostics iv. Pharmaceuticals vi. Public health National/ Central Goverment Regional/ State governments Local/ Municipal governments Social health insurance Private health insurance Other, please specifiy: Note: For many countries, SHA data allow identifying the main financing agent by category of services. However, this table is proposed to help respondents identifying the “key purchasers” they will refer to in the following questions. Comments/clarifications: Question 27. Please provide information on provision of primary care services and payment methods used by key purchasers below: a. Are primary care services* provided predominantly in (please check only one answer): Public primary care clinics staffed by physicians only Public primary care clinics staffed by physicians and other health professionals (e.g., nurses) Outpatient departments of public hospital Private solo practices Private group practices staffed by physicians only Private group practices staffed by physicians and other health professionals (e.g., nurses) Outpatient departments of private hospital Other, please specify ______________________________________ b. If the predominant mode of provision of primary care services is group practice or clinics, please specify the average number of physicians in the practice/clinic: _____________ c. What is the share of the predominant service model in primary care services? The share can be expressed (by order of preference) as a % of primary care spending, or as a % of primary care contacts, or as a % of primary care “providers”. Please specify the unit used.______________________ d. How are these providers paid for primary care services by key purchasers? (Check all that apply) Capitation Fee-for-service Pay-for-performance Global budget Other, please specify ___________________ 13 e. If capitation is one component of payment, is it adjusted in any way? Yes If so, what are the main risk factors used for adjustment? (check all that apply) Age Gender Health status (e.g. measured by prevalence of specific conditions) Prior utilization of services Other (please specify): ______________________ No Comments, clarifications f. Is there a second significant form of service provision (providing more than 20% of primary care services, as measured in the unit used in Q27c)? No Yes, If so, please indicate the second main form of service provision (check only one answer): Public primary care clinic staffed by physicians only Public primary care clinic staffed by physicians and auxiliary medical staff (e.g., nurses) Outpatient department of public hospital Private solo practice Private group practice staffed by physicians only Private group practice staffed by physicians and auxiliary medical staff (e.g., nurses) Outpatient department of private hospital Interdisciplinary teams and nurse practitioner setting g. How are these providers paid for primary care services by key purchasers? (check all that apply) Capitation Fee-for-service Pay-for-performance Global budget Other, please specify h. If capitation is one component of the payment, is is it adjusted in any way? Yes If so, what is the main risk factors used for adjustment? (check all that apply) Age Gender Health status (e.g. measured by prevalence of specific conditions) Prior utilization of services Other (please specify) ____________________ No Comments/clarifications (if any): Question 28. Please provide information on the provision of ambulatory/out-patient specialist services and payment methods used by key purchasers below: a. Are ambulatory/outpatient specialists' services provided predominantly in: Public multi-specialty clinic Outpatient department of public hospital Private solo specialists Private group practice Outpatient department of private hospital b. What is the share of the predominant service model in out-patient specialist services? The share can be expressed (by order of preference) as a % of spending, or as a % of contacts, or as a % of “providers”. Please specify the unit used.______________________ c. How are these providers paid by key purchasers? (check all that apply) Fee-for-service Global budget Pay-for-performance Other, please specify _________________ Comments/clarifications: d. Is there a second significant form of service provision (providing more than 20% of ambulatory/outpatient specialist services)? No Yes, e. If so, please indicate the second main form of service provision: Public multi-specialty clinic Outpatient department of public hospital Private solo specialists Private group practice Outpatient department of private hospital f. How are these providers paid by key purchasers: Fee-for-service Global budget Pay-for-performance Other, please specify Comments/clarifications (if any): Question 29. What are the possible statuses of hospitals delivering acute inpatient care? (check all that apply) Publically owned hospitals Not-for-profit privately owned hospitals 15 For-profit privately owned hospitals Question 30. Are public hospitals mainly owned by: (Please only check one answer) Central Government Regional Government Municipal Government Social health insurance funds Others, please specify : ________________ Question 31. What is the main payment method used by key purchasers of care to pay for acute care in each relevant category ? Please refer to definitions in the glossary for the terms marked with a * Please check only one answer per category a. Public hospitals Prospective global budget* Line-item budgets* Payment per case (DRG-like)* Payment based on procedure or service Per diem Retrospective payments of all costs Is capital funding covered in these payments? Yes No Are teaching, training and research funded separately? Yes No If a second method is used and represents a significant share of revenues for the kind of hospital under consideration (e.g., 20% or more), please specify: ____________________________________________________ b. Private not-for-profit hospitals Prospective global budget* Line-item budgets* Payment per case (DRG-like)* Payment based on procedure or service Per diem Retrospective payments of all costs Is capital funding covered in these payments? Yes No Are teaching, training and research funded separately? Yes No If a second method is used and represents a significant share of revenues for the kind of hospital under consideration (e.g., 20% or more), please specify: ____________________________________________________ c. Private for profit hospitals Prospective global budget* Line-item budgets* Payment per case (DRG-like)* Payment based on procedure or service Per diem Retrospective payments of all costs Is capital funding covered in these payments? Yes No Are teaching, training and research funded separately? Yes No If a second method is used and represents a significant share of revenues for the kind of hospital under consideration (e.g., 20% or more), please specify: ____________________________________________________ d. If the main payment method for acute care services is payment per case (DRG-like) for any of the categories, please answer the following questions: When was it implemented? ___________________ What is the classification system in use? _________________ How many groups are used? _____________ How frequently is the classification updated? Are day-care services covered by these payments? Are the costs of very expensive medicines included in DRG-rates? Are the costs of very expensive medical devices included in DRG-rates? If hospital physicians are self-employed, are physician fees included in DRG rates? Comments/clarifications (if any): Question 32. What happens if the expenditure of a public hospital exceeds its revenue? Check all that applies It cannot happen, deficits are not allowed The hospital (or its owners) must finance the deficit (through grants, loans, restructuring of activities) 17 Arrears can accumulate over years and public payers/government generally bail out Arrears can accumulate over years but hospital can default and be closed Other (please provide additional information in the comments/clarifications) Comments/clarifications (if any): Section 2. Employment status and payment of health care professionals This section aims to collect information on the status and payment of health care professionals with the main focus on physicians. In most countries, physicians can choose among several status and payment methods, or even have multiple exercices. Therefore, this section aims to collect information on the predominant status and payment methods for each category of service. Countries are invited to provide information on the relative size of the “predominant” category whenever possible. Question 33. Please provide information on the employment status and payment methods of physicians supplying primary care services: a. Are physicians supplying primary care services predominantly: Self employed Publically employed Privately employed b. What is the share of primary care physicians working in this category (exclusively or not)? ____ c. Are these physicians remunerated by? Salary Fee-for-service Capitation A mix of these – plus other types of payments when relevant. Please indicate the different components of the mix and the average share of each component for an individual doctor where available d. Do at least 20% of physicians providing primary care services belong to another category? No Yes, e. If so, which category: Self employed Publically employed Privately employed f. Are they remunerated by: Salary Fee-for-service Capitation A mix of these. Please indicate the different components of the mix and the average share of each component for an individual doctor where available: _______________ g. Is dual practice allowed for primary care physicians (e.g. as self-employed and publically employed)? No Yes, in some circumstances only (e.g. only in some states in federal countries, or for some categories of physicians) Yes, always If dual practice is allowed, what is the share of primary care physicians with dual practice? _____ Comments/clarifications (if any): Question 34. Please provide information on the employment status and payment methods of physicians supplying out-patient specialist services: a. Are physicians supplying out-patient specialist services predominantly: Self employed Publically employed Privately employed b. What is the share of specialists supplying outpatient services working in this category (exclusively or not)? ____ c. Are these physicians remunerated by : Salary Fee-for-service A mix of fee-for-service and salary. Please indicate the average share of each component for an individual doctor where available _______________________________ d. Do at least 20% of physicians providing out-patient specialist services belong to another category? No Yes, e. If so, which category: Self employed Publically employed Privately employed f. Are these physicians remunerated by: Salary Fee-for-service A mix of fee-for-service and salary. Please indicate the average share of each component for an individual doctor ___________ g. Is dual practice allowed for specialists supplying outpatient services** (e.g. as self-employed and publically employed)? No Yes, in some circumstances only (e.g. only in some states in federal countries, or for some categories of physicians) Yes, always If dual practice is allowed, what is the share of specialists with dual practice? _____ 19 ** In some countries, it may not be possible to distinguish specialists supplying out-patient services from specialists providing inpatient services for this question. In such a situation, please indicate in comments below. Comments/clarifications (if any): Question 35. Please provide information on the employment status and payment method of physicians supplying in-patient specialist services: a. Are physicians supplying in-patient specialist services predominantly: Self employed Publically employed Privately employed b. What is the share of specialists supplying inpatient services working in this category (exclusively or not)? ____ c. Are these physicians remunerated by: Salary Fee-for-service A mix of fee-for-service and salary. Please indicate the average share of each component for an individual doctor ___________ d. Do at least 20% of physicians providing in-patient specialist services belong to another category? No Yes, e.If so, which category: Self employed Publically employed Privately employed f. Are these physicians remunerated by: Salary Fee-for-service A mix of fee-for-service and salary. Please indicate the average share of each component for an individual doctor ___________ g. Is dual practice allowed for specialists supplying inpatient services** (e.g. as self-employed and publically employed)? No Yes, in some circumsntances only (e.g. only in some states in federal countries, only in underserved areas, or for some categories of physicians) Yes, always If dual practice is allowed, what is the share of specialists with dual practice? _____ ** In some countries, it may not be possible to distinguish specialists supplying out-patient services from specialists providing inpatient services for this question. In such a situation, please indicate in comments below. Comments/clarifications (if any): Question 36. Please provide information on the regulation of recruitment and remuneration of medical staff in public hospitals. a) Recruitment of medical staff Hospital managers have complete autonomy Hospitals must negotiate with local authorities Central or sub-national level of government decides Not applicable (physicians are always or most often self-employed and therefore not recruited or appointed) b) Remuneration level of medical staff Hospital managers have complete autonomy A pay scale is set or negotiated at the national level A pay scale is set or negotiated at a sub-national level (e.g. province, region, canton, etc.) Not applicable (physicians are not salaried) c) Are work contracts of the salaried medical staff officially with: The hospital Local authority State government Central government Not applicable (self-employed physicians) Comments/clarifications (if any): Section 2b. Special focus on pay-for-performance and other financial incentives for providers The following questions investigate the existence of bonus or pay-for-performance payments for physicians. Question 37. Can primary care providers (physicians or practices) get a payment bonus for the achievement of targets relating to the quality of care furnished (pay-for-performance)? No Yes If so, please answer the questions below: Note: In some countries, several programmes have been implemented that cover different states, regions or different therapeutic areas. The following questions aim to get an overall picture of the types of 21 incentives used in the country as a whole. So, please refer to the most significiant programmes or combination of significant programmes when answering questions below. b. Could you please provide the name(s) and date(s) of implementation of the programme(s) that introduced such payments and provide links to policy documents on line if available: Programme 1. Name: _____________________ Date: Programme 2. Name: _____________________ Date: Programme 3. Name: _____________________ Date: (allow up to 5) Please provide information for the largest pay–for-performance scheme for items c-j c. For those providers participating to the programme(s), do targets typically relate to: (Check all that apply) Preventive care (e.g., vaccination rate) Management of chronic diseases Uptake of IT services (e.g., electronic medical recording or electronic prescribing) Patient satisfaction Efficiency (e.g. share of generics in pharmaceutical prescriptions) Other, please specify : ___________________ d. Is participation: Mandatory for all primary care providers nationwide Mandatory for all primary care providers in a target category (e.g., a region) Voluntary and open to all primary care providers Voluntary but subject to some conditions (e.g., accreditation, practice size, geography etc.) e. Is performance against quality objectives defined in terms of: Absolute measure (e.g., screening rate of 80%) Change over time (e.g., increase in screening rate by 10%) relative ranking (e.g., 10% highest performers earn bonuses) f. Is the bonus payment normally paid to: The organization (e.g., physician group) Directly to individual physicians g. What is the share of participating providers: - In the total number of providers eligible to the programme(s)? ______ - In the total number of primary care providers ? ___________ h. What is the proportion of primary care physicians who earn bonuses? ______(%) i. For the primary care physicians that earn bonuses, what share of their overall revenues do these bonuses account for? _____(%) j. As part of the programmes, do non-financial incentives also exist (e.g., publicized rankings)? Yes If so, please specify: ___________________ No Comments/clarifications (including reference document): Question 38. Can specialists get a payment bonus for the achievement of targets relating to the quality of care furnished (pay-for-performance)? No Yes If so, please answer the questions below: Note: In some countries, several programmes have been implemented that cover different states or regions, different specialties or different therapeutic areas. The following questions aim to get an overall picture of the types of incentives used in the country as a whole. So, please refer to the most significiant programmes or combination of significant programmes when answering questions below. b. Could you please provide the name(s) and date(s) of implementation of the programme(s) that introduced such payments and provide links to policy documents on line if available: Programme 1. Name: _____________________ Date: Programme 2. Name: _____________________ Date: Programme 3. Name: _____________________ Date: (allow up to 5) Please provide information for the largest pay-for- performance scheme for items c-i c. For those providers participating to the programme(s), do targets typically relate to: (Check all that apply) Preventive care (e.g., vaccination rate) Management of chronic diseases Uptake of IT services (e.g., electronic medical recording or electronic prescribing) Patient satisfaction Other, please specify : ___________________ d. Is participation: Mandatory for all specialists nationwide Mandatory for all specialists in a target category (e.g., a region) Voluntary and open to all specialists Voluntary but subject to some conditions (e.g, specialists in a certain network of physicians) e. Is performance against quality objectives defined in terms of: Absolute measure (e.g., screening rate of 80%) Change over time (e.g., increase in screening rate by 10%) relative ranking (e.g., 10% highest performers earn bonuses) f. Is the bonus payment normally paid to: The organization (e.g., physician group) Directly to individual physicians 23 g. What is the share of participating physicians: - In the total number of specialists eligible to the programme(s)? ______ - In the total number of specialists ? ___________ h. What is the proportion of specialists who earn bonuses? ______(%) g. For the physicians that earn bonuses, what share of their overall revenues do these bonuses account for? _____(%) i. As part of the programme, do non-financial incentives also exist (e.g., publicized rankings)? Yes If so, please specify: ___________________ No Comments/clarifications (if any): Question 39. a. Do some acute care hospitals get a payment bonus for the achievement of targets relating to the quality of care furnished (pay-for-performance)? No Yes, If so, please answer the questions below: In some countries, several programmes have been implemented that cover different regions, different types of hospitals or different therapeutic areas. The following questions aim to get an overall picture of the types of incentives used in the country as a whole. So, please refer to the most significiant programmes or combination of significant programmes when answering questions below. b. Could you please provide the name(s) and date(s) of implementation of the programme(s) that introduced such payments and provide links to policy documents on line if available: Programme 1. Name: _____________________ Date: Programme 2. Name: _____________________ Date: Programme 3. Name: _____________________ Date: (allow up to 5) Please provide information for the largest pay-for-performance scheme for items c-i c. For those hospitals that participate to the programmes, do targets typically relate to (check all that apply): Clinical outcomes of care (e.g., acute myocardial infarction 30-day mortality) The use of appropriate processes (e.g., thrombolytic agent received within 30 minutes of hospital arrival for patients with heart attack) Patient satisfaction (subjective appreciation on the quality of care and accommodation) Patient experience (waiting times, information given by medical staff, etc.) d. Is participation: Mandatory for all providers nationwide Mandatory for all providers in a target category (e.g. a region) Voluntary e. Is performance against quality objectives defined in terms of: Absolute measure (e.g., screening rate of 80%) Change over time (e.g., increase in screening rate by 10%) Relative ranking (e.g., 10% highest performers earn bonuses) f. What is the share of participating hospitals? In % of total hospitals providing acute inpatient care: ______ In % of hospitals providing acute inpatient care and eligible to the programme? ____ g. What is the proportion of participating hospitals that earn bonuses? ______(%) h. For those hospitals that earn bonuses, what share of their overall revenues do these bonuses account for? _____(%) i. As part of the programme, do non-financial incentives also exist (e.g., publicize rankings)? Yes If so, please specify: ___________________ No Comments/clarifications (including reference document): Section 3. Patients' choice and competition among providers Please describe the usual or most common situation for health care covered by basic health care coverage*. Question 40. Are patients required or encouraged to register with a primary care physician or practice (i.e., required/encouraged to consult this primary care provider in case of need)? Patients are obliged to register Patients are not obliged to register with a primary care physician (or practice) but have financial incentives to do so (e.g., reduced copayments) There is no incentive and no obligation to register with a primary care physician (or practice) Question 41. Do primary care physicians control access to outpatient specialist care? Primary care physician referral is compulsory to access most types of specialist care (except in case of emergency) Patients have financial incentives to obtain a primary care physicians referral (e.g., reduced copayments), but direct access is always possible 25 There is no need and no incentive to obtain primary care physician referral Question 42. a. Are patients generally free to choose a provider for primary care services*? In countries with federal or otherwise decentralised systems, patient choice may vary across states or regions. For the three following questions, please check only one answer if one proposed option covers more than 80% of the population, check several options if the overall picture is more contrasted. Please indicate what are patients’ rights and entitlements and not what results from local supply constraints. The patient is assigned to a specific provider (e.g. a health center serving a geographical area) The patient’s choice is limited (e.g., to a small geographical area, or to a specific network of providers) Patients can choose any primary care provider but have financial incentives (e.g., reduced copayments) to choose certain providers Patients do not face any incentives to choose one provider over another Question 42b. Can the patient choose his/her individual doctor within the facility he/she has chosen or he/she is assigned to? Yes No Not relevant (primary care services are predominantly provided by physicians in solo practice) Comments/clarifications (if any): Question 43a. Are patients usually free to choose providers for out-patient specialist services? In countries with federal or otherwise decentralised systems, patient choice may vary across states or regions. For the three following questions, please check only one answer if one proposed option covers more than 80% of the population, check several options if the overall picture is more contrasted. Please indicate what are patients’ rights and entitlements and not what results from local supply constraints. The patient is assigned to a specific provider (e.g. a health centre serving a geographical area) The patient’s choice is limited (e.g., to a small geographical area, or to a network of providers) Patients can choose any physician providing out-patient specialist services but have financial incentives (e.g., reduced copayments) to choose certain providers Patients do not face any incentives to choose one provider over another b. If facilities providing out-patient specialist services are not solo practices, can the patient choose his/her individual doctor within the institution he has chosen or he is assigned to? Yes No Not relevant (out-patient specialist are predominantly provided by physicians in solo practice) Comments/clarifications (if any): Question 44. Are patients usually free to choose hospitals for in-patient care? In countries with federal or otherwise decentralised systems, patient choice may vary across states or regions. For the three following questions, please check only one answer if one proposed option covers more than 80% of the population, check several options if the overall picture is more contrasted. Please indicate what are patients’ rights and entitlements and not what results from local supply constraints. Patients can choose any hospital without any consequence for the level of coverage Patients are free to choose any hospital but they have financial incentives to choose some providers (e.g., the closest hospital, or hospitals which have signed specific contract with their insurer, etc.), please specify: ________________________________________ The patient’s choice is theoretically limited (e.g., to a geographical area or to publicy financed hospitals only) but may be expanded in certain circumstances (for instance, if waiting times are too long). Please indicate in which circumstances: ___________________________________ The patient’s choice is strictly limited with no exception (e.g., to a geographical area or publicly funded hospitals). Please specify limitations: ______________________________________ Comments/clarifications (if any): Can patients choose their individual doctor within the hospital? Always Under certain circumstances only (e.g.: if they have a certain type of health insurance, if they are prepared to pay extra-fees…). Please specify ___________________ Usually not The three following questions below seek to understand whether health care services prices are a concern to patients when selecting a provider, and whether information on prices is available to them. Question 45. Are prices of primary care services the same or different across providers? Health care services are free at the point of care All providers charge the same price to patients (partly of fully refunded by coverage schemes) Prices charged to patients can vary across providers (e.g. according to the physician’s status) with possible consequences on patient’s own expenses How available is information about the prices of physicians’ consultations/visits? Information on prices charged by providers is required to be readily available (posted, communicated in advance) Information on prices charged by providers is in practice most often readily available (posted, communicated in advance) Patients generally do not know the price they will pay before meeting the doctor Comments/clarifications (if any): Question 46. Are prices of out-patient specialist services the same or different across providers? Out-patient specialist services are free at the point of care All providers charge the same price to patients (partly of fully refunded by coverage schemes) Prices charged to patients can vary across providers (e.g. according to the physician’s status) with possible consequences on patient’s own expenses 27 How available is information about the prices of out-patient specialist physicians’ consultations/visits? Information on prices charged by providers is required to be readily available (posted, communicated in advance) Information for prices charged by providers is in practice most often readily available (posted, communicated in advance) Patients generally do not know the price they will pay before meeting the doctor Comments/clarifications (if any): Question 47. How available is information about the quality of care of providers? Please complete the following table: Primary care practices Is there any comparable information published on the quality of services? (please tick the box is information is published) If so, what type of information is available: Data on clinical outcomes (e.g., post-operative survival rates, rates of nosocomial infections) Data on the use of appropriate processes (e.g., % of people vaccinated, activities to prevent nosocomial infection, % of hip fractures treated within 48 hours) Data on patient satisfaction (subjective assessment of the quality of interpersonal interactions, the quality of care or of accommodation) Data on patient experiences (objective information about information given by medical staff, etc) . Physicians supplying outpatient services Individual Hospitals Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Of which: data on waiting times Is the information in a form that facilitates comparisons across providers (e.g., league tables)? Who develops and/or publishes such information: Government Insurers Media Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Other NGO's (non governmental organisations) None of the above (please specify) Health care providers Is there evidence that such information is used by prospective patients in selecting providers? Is there evidence that such information is used by providers in informing referrals? Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Yes No N/a Comments/clarifications (if any): Section 4. Workforce training and regulation Question 48a. Is there any limit for entry into initial medical education? (check all that apply) quotas for the total number of medical students intake quotas by speciality budget or capacity constraints in medical education There are no limits Comments/clarifications (if any): b. Who sets these limits? National government Sub-national levels of government Universities Others, please specify: ______________________ c. Have any major changes in medical students intake occurred during the past 5 years? Yes If so, please describe: ____________________ No Comments/clarifications (if any): Question 49. Are medical doctors required to obtain a further qualification in addition to a basic medical degree in order to practice as a primary care physician*? Yes No Comments/clarifications (if any): Question 50. Do formal requirements (e.g., accreditation*) exist for primary care practices or facilities to operate? 29 Yes, it is mandatory Yes, it is voluntary but encouraged No Question 51. Is there a formal system of continuous medical education* (CME) in place for physicians? No Yes, If so, does it apply to all specialities? Yes No (Please describe in comments/clarifications) Is the system mandatory to all physicians? Yes, CME is mandatory but not linked to recertification or relicensing* of physicians Yes, CME is mandatory and linked to recertification or relicensing of physicians No, participation to CME is voluntary Comments/clarifications (if any): Question 52. What are the main issues that the Ministry of Health might have identified in relation to physician supply? Check all that apply No particular issue Difficulties in maintaining the current level of physician supply Difficulties in meeting increasing demand for health care services Difficulties in maintaining the current share of general practitioners in the overall physician supply Identified shortages in some specialties, please specify _________________________ Mal-distribution of physician supply, for instance, geographic variations between rural and urban areas Others, please specify: ___________________________________________________ Comments/clarifications (if any): Question 53. What are the policies in place to address the identified physician supply problems? Check all that apply No particular policy Increase in training capacity Prolong working time for physicians (e.g., incentives for postponing retirement) Targeted immigration policy Incentives to foster the take-up of general practice (financial and non financial) Incentives to foster the take-up of specialties where shortages exist or are expected (financial and non financial) Introduction or expansion of non-physician practitioner roles (e.g., nurse practitioner) Financial incentives to correct perceived geographic mal-distribution Other, please specify : _______________________ Comments/clarifications (if any): Question 54. Is there any regulation that restricts physicians in the location of their practices (relating to density, geographic proximity or other factors)? Yes No Comments/clarifications (if any): Question 55. Is there any limit for entry into nursing education? (check all that apply) quotas for the total number of students intake budget or capacity constraints in nursing education There are no limits Comments/clarifications (if any): Who sets these limits? National government Sub-national levels of government Universities Others, please specify: ______________________ Have any major changes in nursing students intake occurred during the past 5 years? Yes If so, please describe: ____________________ No Comments/clarifications (if any): Section 5. Regulation of supply of hospital services and high-cost medical equipment This section aims to understand the extent to which providers are free to establish and expand capacities in specialised care Question 56. Is there a national accreditation program for hospitals? No Yes If so, who runs the accreditation program? Government Arm’s length body What is the percentage of hospitals accredited nationwide? ______ % 31 Question 57. Is there any regulation of the number and “type” (e.g. obstetric, surgery, etc…) of hospital beds? No, there is no regulation: providers are free to establish and expand capacities Yes If so, does it apply: To all hospitals which operate on the territory To all hospitals which aspire to contract with the main purchaser(s) of services Only to some categories of hospitals, If so, which one(s) (check all that apply): public hospitals private not-for-profit hospitals private for profit hospitals If several types of providers are regulated, is the regulation “integrated” (i.e. does the same regulatory framework apply to all sectors)? Yes No What is the regulatory framework in place (The question will be asked for all sectors or for each type of providers, depending on response to question above)? Check all that apply Quotas are set at central/national level, below which providers can expand capacities Quotas are set at local level, below which providers can expand capacities. Please specify which “local level” (region, municipality, district…) : ____________________ Central government plans and monitors capacities and authorises each investment Local government plans and monitors capacities and authorises each investment Key purchasers agree on new capacities Local agencies representing government and main purchasers agree on new capacities Comments/Clarifications: Question 58. Is there any regulation on the number and location of high-cost equipments (e.g. MRI, PET scan)? No, there is no regulation: providers are free to establish and expand capacities Yes If so, does it apply to: All providers/facilities which operate on the territory All providers/facilities which aspire to contract with the main purchaser(s) of services Only to some categories of providers/facilities, If so, which one(s) (check all that apply): public providers private not-for-profit providers private for profit providers If several types of providers are regulated, is the regulation “integrated” (i.e. does the same regulatory framework apply to all sectors)? Yes No What is the regulatory framework in place (The question will be asked for all sectors or for each type of providers, depending on response to question above)? Check all that apply Quota are set at central/national level, below which providers can expand capacities Quota is set at local level, below which providers can expand capacities. Please specify which “local level” (region, municipality, district…): ____________________ Central government plans and monitors capacities and authorises each investment Local government plans and monitors capacities and authorises each investment Key purchasers agree on new capacities Local agencies representing government and main purchasers agree on new capacities Comments/clarifications: Question 59. Do providers get some incentives to expand capacities in high-cost medical equipments? Providers get financial incentives from national or local authorities (e.g., subsidies) for each investment; Providers get financial incentives from national or local authorities (e.g., subsidies) in some cases (e.g. underserved area, public providers only…). Please specify: __________________________________________ Providers do not get incentives from authorities, investments in such capacities are only a means to attract patients and/or physicians and develop activities. Providers get other types of incentives from national or regional authorities, please specify: Comments/clarifications (if any): Section 6. Price regulation for health care services This section aims to understand how prices paid by key third party payers (key purchasers identified in question 26) are set, as well as the extent to which prices billed to patients can exceed these prices. Please note that the online questionnaire will only include options that are relevant according to responses provided for questions 27, 28 and 31 (in Part II, Section I on “Health care provision”) Question 60. How are fees paid by third-party payers for primary care services determined? (please check all that apply) If fee-for-service is a component or single mode of payment of primary care services 33 a. Are fees based on a common Resource-Based Relative Value Scale (or equivalent)? No Yes, there is one RBRVS for the whole country Yes, there are several RBRVS for different regions/states of the country or different payers b. Are fees (or point values of the RBRVS): Unilaterally set by central/national governments Unilaterally set by key purchasers Negotiated at central level between key purchasers’ and providers’ associations Negotiated at state/regional level between key purchasers’ and providers’ associations Negotiated between individual purchasers and providers Other, please specify __________________________________ And/or if capitation is a component or main payment method of payment of primary care services, how is the capitation determined? Capitation is unilaterally set by key pushasers or government at central level Capitation is negotiated between key purchasers’ and providers’ associations at central level Capitation is negotiated between key purchasers’ and providers’ associations at local level Capitation is negotiated between purchasers and providers Other, please specify And/or if global budget is a component or main payment method of payment of primary care services Budget of each provider is determined by allocation principles defined at central level Budget of each provider is determined by allocation principles defined at local level Budget of each provider is negotiated with key purshasers Other, please specify Question 61. Who defines the price billed to patients for primary care services (if any)? Note: the price billed to patient may be partially or fully covered by any type of health insurance Not applicable, health care services are free at the point of care Providers cannot charge patients beyond the rate defined for basic health insurance payments (which may include statutory copayments); Providers can charge any price in some circumstances (depending on their status, or on patients’ status), please specify: ________________________________________ Providers can charge any price but receive guidance (e.g. from the medical association) Providers can charge any price without any guidance Comments/clarifications (if any): Question 62. How are fees paid by third-party payers for outpatient physicians services determined? (check all that apply) If fee-for-service is a component or single mode of payment for out-patient specialist services a. Are fees based on a common Resource-Based Relative Value Scale (or equivalent)? No Yes, there is one RBRVS for the whole country Yes, there are several RBRVS for different regions/states of the country or different payers b. Are fees (or “the point value” of RBRVS) Unilaterally set by central/national governments Unilaterally set by key purchasers Negotiated at central level between key purchasers’ and providers’ associations Negotiated at state/regional level between key purchasers and providers Negotiated between individual third-party payers and providers Other, please specify And/or if global budget is a component or single mode of payment for out-patient specialist services Budget of each provider is determined by allocation principles defined at central level Budget of each provider is determined by allocation principles defined at state/regional level Budget of each provider is negotiated with key purchasers Other, please specify Please specify the interested parties involved in the process (e.g., physician associations, statutory health insurance funds, etc) if relevant. ____________________________________________________ Question 63. Who defines the price billed to patients for out-patient specialist services (if any)? Note: the price billed to patient may be partially or fully covered by any type of health insurance Not applicable, health care services are free at the point of care Providers cannot charge patients beyond the rate defined for basic health insurance payments (which may include statutory copayments); Providers can charge any price in some circumstances (depending on their status, or on patients’ status), please specify: _________________________________________________ Providers can charge any price but receive guidance (e.g. from the medical association) Providers can charge any price without any guidance Comments/clarifications (if any): Question 64. How are prices paid to hospitals by key purchasers established for acute inpatient services? (check all that apply) Public hospitals If DRG is the main payment mechanism of acute hospital services DRG weights are defined at central level DRG “point value” are set unilaterally by government or key purchasers at central level and identical for all hospitals of the country DRG “point values” are negotiated between key purchasers’ and providers’ associations at central level DRG “point value” are set unilaterally by local government or key purchasers and identical for all hospitals in the locality (e.g. region) DRG “point values” are negotiated between key purchasers’ and providers’ associations at local/sub-national level DRG “point values” are set unilaterally by individual key purshasers DRG “point values” are negotiated between individual key purchasers and individual hospitals 35 Other, please specify If Fee-for-service is the main payment mechanism of acute hospital services A Resource-Base Relative Value Scale is established at central level Fees are set unilaterally by key purchasers (or government) at central level. Fees are set unilaterally by key purchasers (or government) at local/sub-national level Fees are negotiated at central level between key purchasers and providers Fees are negotiated at local/sub-national level between key purchasers and providers Fees are negotiated between individual key purchasers and providers others, please specify If Global budget/line item is main the payment mechanism of acute hospital services Budget of each provider is determined by allocation principles defined at central level Budget of each provider is determined by allocation principles defined at local/sub-national level Budget of each provider is negotiated with financing authorities If per diem payments are the main payment mechanism of acute hospital services Per diem payments are set unilaterally by government or key purshaers at central level and identical for all hospitals of the country Per diem payments are negotiated between key purchasers’ and providers’ associations at central level Per diem payments are set unilaterally by local government or key purchasers and identical for all hospitals in the locality (e.g. region) Per diem payments are negotiated between key purchasers’ and providers’ associations at local/sub-national level Per diem payments are set unilaterally by individual key purshasers Per diem payments are negotiated between individual key purchasers and individual hospitals Private hospitals If DRG is the main payment mechanism of acute hospital services DRG weights are defined at central level DRG “point value” are set unilaterally by government or key purchasers at central level and identical for all hospitals of the country DRG “point values” are negotiated between key purchasers’ and providers’ associations at central level DRG “point value” are set unilaterally by local government or key purchasers and identical for all hospitals in the locality (e.g. region) DRG “point values” are negotiated between key purchasers’ and providers’ associations at local/sub-national level DRG “point values” are set unilaterally by individual key purshasers DRG “point values” are negotiated between individual key purchasers and individual hospitals Other, please specify If Fee-for-service is the main payment mechanism of acute hospital services A Resource-Base Relative Value Scale is established at central level Fees are set unilaterally by key purchasers (or government) at central level. Fees are set unilaterally by key purchasers (or government) at local/sub-national level Fees are negotiated at central level between key purchasers and providers Fees are negotiated at local/sub-national level between key purchasers and providers Fees are negotiated between individual key purchasers and providers others, please specify If Global budget/line item is main the payment mechanism of acute hospital services Budget of each provider is determined by allocation principles defined at central level Budget of each provider is determined by allocation principles defined at local/sub-national level Budget of each provider is negotiated with financing authorities If per diem payments are the main payment mechanism of acute hospital services Per diem payments are set unilaterally by government or key purshaers at central level and identical for all hospitals of the country Per diem payments are negotiated between key purchasers’ and providers’ associations at central level Per diem payments are set unilaterally by local government or key purchasers and identical for all hospitals in the locality (e.g. region) Per diem payments are negotiated between key purchasers’ and providers’ associations at local/sub-national level Per diem payments are set unilaterally by individual key purshasers Per diem payments are negotiated between individual key purchasers and individual hospitals Comments/clarifications (if any): Question 65. Who defines the price billed by hospitals to patients for in-patient acute care services (if any)? Note: the price “billed to patient” may be partially or fully covered by any type of health insurance, please do not consider access to comfort accommodation services (e.g. TV, telephone…) when answering, but only prices for medical services. Not applicable, services are free at the point of care (or only entail a small copayment) Hospitals cannot charge patients beyond the rate defined for third-party payers’ payments (which may include statutory copayments); Hospitals can charge any price in some circumstances (depending on providers’, physicians’ or patients’ status), please specify: -------------------------------------- Providers are always freely determines their prices Comments/clarifications (if any): Section 7. Regulation / monitoring of health providers’ activity Question 66. Are physicians required or incentivised to comply with treatment guidelines or practice protocols established? No, there is no incentive or obligation There are financial incentives (rewards) Compliance is compulsory, but without effective monitoring and/or sanctions 37 Compliance is compulsory, with effective monitoring or sanctions Comments/clarifications (if any): Question 67. Is there any regulation/control on health provider activity? (Check all that apply) Health insurance funds or the national or local health service usually monitors the volume of physician activity. Physicians usually receive feedback about their activity or prescriptions. Prescription targets or budgets are defined. Compliance with guidelines is monitored. Other, please specify ________________________ No regulation/control Comments/clarifications (if any): Section 8. Coordination and continuity of care Question 68. Are case management programs* commonly used for patients with complex conditions requiring chronic care and Long-Term Care? No Yes If so, are case management services provided by: Management doctors Management nurses Case managers (with qualifications other than nurses and doctors) Comments/clarifications: Question 69a. Please provide the percentage of primary care physician keeping (or reporting to keep) electronic medical records for patient contacts routinely: _______________________ Comments/clarifications: Question 69b. Do physicians transfer or exchange information electronically for diagnosis or treatment purposes across different health care providers? Regularly Regularly, in some settings only (e.g., hospital, labs) Occasionally Rarely Comments/clarifications: Question 69c. Do primary care doctors/clinics routinely utilise a patient registration system? Yes No Comments/clarifications: Question 70. Describe how at a national/federal level awareness has been raised of the need to assess and treat multiple morbidity in a systematic manner both within the primary care and hospital settings. Specifically; a. Are you planning the development of guidelines for multiply occurring chronic conditions and if so which ones? Yes No b. Have there been changes to training programmes for generalist doctors (ie GPs/family physicians, geriatricians, general internists) which are aimed at improving the assessment/treatment of multimorbidity ? Yes No c. Is the impact of multi-morbidity currently (or intended to be) monitored in terms of : patient satisfaction impact on the health economy quality of care and patient outcomes None of the above Question 71. Are the following risk factors usually or systematically monitored in primary care? Over weight/obesity: Poor physical activity: Smoking status: Alcohol misuse: Yes No Yes No Yes No Yes No If so, do primary care physicians have a standard referral intervention at their disposal for the listed risk factors? No Yes, If so, please provide examples of standard referral interventions available (e.g., referral to stop smoking centres) in comments/clarifications. Comments/clarifications (if any): 39 Question 72. What is the predominant mode of provision of out-of-hours* primary care? a) Rural area: Primary care physicians within one practice or organized in a group of practices look after their patients on out-of-hours schedules Primary care physicians from several groups in a region provide after-hours PC mostly in nonprofit, large-scale organizations; e.g., telephone triage and advice, office for face-to-face contact, and house calls Companies employing doctors take over the provision of after-hours care Hospital emergency departments provide primary care by taking care of health problems after office hours Walk-in after-hours PC centres for face-to-face contact with a primary care physician or nurse Other out-of-hours primary care service schemes in place b) Urban area : Primary care physicians within one practice or organized in a group of practices look after their patients on out-of-hours schedules Primary care physicians from several groups in a region provide after-hours PC mostly in nonprofit, large-scale organizations; e.g., telephone triage and advice, office for face-to-face contact, and house calls Companies employing doctors take over the provision of after-hours care Hospital emergency departments provide primary care by taking care of health problems after office hours Walk-in after-hours PC centres for face-to-face contact with a primary care physician or nurse Other out-of-hours primary care service schemes in place Question 73. Are some patients maintained in acute care settings because of a lack of suitable alternatives (e.g. Long-term care or rehabilitation beds, nursing homes, home care)? Yes No Is there any estimate of this problem (e.g. number of “bedblockers”) ? Yes If so, please provide a reference document in comments/clarifications No Comments/clarifications: PART III. GOVERNANCE AND RESOURCE ALLOCATION Note: This Governance Section intentionally does not include questions on all aspects of Governance that we consider to be important. The OECD secretariat already collects information through a variety of sources, especially in the Governance Directorate (e.g. Government at a Glance). In addition, the Health Committee is collecting information on Information and Communication Technology (ICT), including privacy. The OECD will seek to synthesize the diverse sources of available information in describing health system governance. Please note that questions on Health Technology Assessment, currently included in part II of the questionnaire, will be moved to this part of the questionnaire (in section 1). They are not included in this draft since you already provided comments on them. Section 1: Health system stewardship Section 2: Budgeting process Section 3: Patients rights and citizens’ involvement Section 1. Health system stewardship Question 74. Are targets set for improvements in population health outcomes ? No Yes If so, Who sets these targets? (Multiple responses are possible, e. g. in cases where different targets are set for each sub-national jurisdiction.) ___________________________________________________________________________ Please provide a few examples of targets: ____________________________________________________________________________ Please provide the references or a weblink for document(s), where relevant: ____________________________________________________________________________ Comments/clarifications: Question 75. Does the government set targets for overall health system performance (e.g., cost, quality, access to care) ? No Yes If so, who sets these targets? (Multiple responses are possible, e. g. in cases where different targets are set for each sub-national jurisdiction.) __________________________________________________________________________ Please provide a few examples of targets: __________________________________________________________________________ Please provide the references or a weblink for document(s), where relevant: __________________________________________________________________________ Comments/clarifications: 41 Question 76. Who is responsible for setting and implementing public health policy? Please check all that apply Policy setting Implementation The central/federal Ministry/Department of Health Quasi-autonomous agency (arm’s length body) Regional/State governments Local /municipal governments Other Comments/clarifications: Question 77. How does the Ministry/Department of Health influence other central/federal government Departments/Ministries to achieve health objectives? Please check all that apply The Ministry/ Department of Health’s ordinary course of business is to interact with other Ministries or Departments There are joint targets shared between the Ministry/Department of Health and other Ministries or Departments There is shared funding with other ministries or departments for specific targeted programmes. There is a permanent inter-Ministerial/Departmental platform or coordination committee to ensure coordinated action across Ministries/Departments (including for specific priorities, e.g. AIDS) Health Impact Assessment is required for policies defined and implemented outside of the Ministry/Department of health If so, how often is health Impact Assessment performed? Always Often Rarely Never Comments/clarifications: Question 77b. Is there a well-defined government strategy to implement “health in all policies” Yes If so, please provide the full reference or a weblink for the document(s) setting out this strategy: : ______________________________________________________________________________ No Comments/clarifications: Question 78. Who is responsible for service standards/quality? For each column (i-iii) please select all rows that apply. Institution i. Hospital licensing ii. Clinical iii. Guidelines Inspection of providers’ settings Continuing professional education requirements for health workers Explicit quality standards (i.e. maximum waiting times, hospital acquired infections) Central/Federal government Agency—quasi autonomous Regional/state government Local/municipal governments Professional associations Association of subnational authorities Health insurance funds Other, please specifiy in comments and clarifications Comments/clarifications: Question 79. How are the services or benefits covered by basic health coverage defined (check all that apply)? a) For medical/surgical procedures: A positive list is established at the central level A negative list (of non-covered procedures) is established at the central level Individual health insurance funds establish their own positive lists (e.g., services that are required to be covered) Individual health insurance funds establish their own negative lists (e.g., services that are excluded from coverage) Providers under budget constraints establish their own positive lists at the local level The benefit basket is not defined, every procedure performed by a clinician is considered by basic primary coverage schemes Comments/clarifications: 43 b) For pharmaceuticals A positive list is established at the central level A negative list (of non-covered procedures) is established at the central level Individual health insurance funds establish their own positive lists (e.g., services that are required to be covered) Individual health insurance funds establish their own negative lists (e.g., services that are excluded from coverage) Providers under budget constraints establish their own positive lists at the local level The benefit basket is not defined; prescription drugs that are approved for marketing are systematically covered by basic primary coverage schemes Comments/clarifications: Question 80. Who performs Health Technology Assessment (HTA) in your country? (check all that apply) An independent body is responsible for HTA in the health sector at central level Main purchasers (health insurance, government) perform HTA at central level. Main purchasers (health insurers, governments) perform HTA at local level to inform their decisions Several independent bodies perform HTA at the request of purchasers or providers groups (e.g. hospitals) HTAs are generally not performed Comments/clarifications: Do health technology assessments generally include results of economic evaluation (original or based on literature review)? No Yes, If so: what is the perspective adopted for economic evaluation? (Public) payer perspective Health system perspective (including consequences for patients or other payers) Societal perspective Do health technology assessments normally take into account affordability or budget impact of the use of the health technology or medicine? Yes No Comments/clarifications: Question 81. Is HTA used in the following circumstances? (check all that apply) For pharmaceuticals: HTA is systematically used to determine whether a new medicine should be covered HTA is used in some circumstances (e.g. on request of a stakeholder) to determine whether a medicine should be covered HTA is used to determine the reimbursement level* or the reimbursement price* of medicines For medical procedures HTA is systematically used to determine whether a new medical procedure should be covered HTA is used in some circumstances (e.g. on request of a stakeholder) to determine whether a medical procedure should be covered HTA is used to determine the reimbursement level* or the reimbursement price* of medical procedures For medical devices HTA is systematically used to determine whether a new medical device should be covered HTA is used in some circumstances (e.g. on request of a stakeholder) to determine whether a medical device should be covered HTA is used to determine the reimbursement level* or the reimbursement price* of medical devices For high cost-equipment (e.g. MRI equipment) HTA is systematically used to determine whether (services related to) a new high-cost equipment should be covered HTA is used in some circumstances (e.g. on request of a stakeholder) to determine whether (services related to) a new high-cost equipment should be covered HTA is used to determine the reimbursement level* or the reimbursement price* of services related to a new high-cost equipment. More generally, HTA is used to establish practice guidelines for health professionals HTA is used to determine objectives for pay-for-performance schemes Section 2. Budgeting process Question 82a. For the latest fiscal year, please indicate (in national currency) the total amount of public expenditure for health covered by the central/federal (decentralized) level of of government (including subnational transfers earmarked for health): __________________________________________ (Note that public expenditures on health include spending by public social health insurance funds where relevant) Comments/clarifications: 45 Question 82b. Which of the following funding sources are used to finance health expenditures? Please check all that apply Revenues from general taxation Revenues from taxes earmarked to the health system Revenues from payroll contributions to social health insurance Revenues from mandatory health insurance premiums Question 83. Central/federal spending. Who has the main responsibility for the following tasks? Please check all that apply a. Proposing the annual expenditure ceiling and/or allocation for the health system. Parliament/Legislature Cabinet of Ministers/Executive Cabinet Ministry/Department of Health Ministry/Department of Finance/Treasury Health Insurance Funds Regional governments Agency – quasi autonomous, please specify ________________ Other, please specify ________________ Comments/clarifications: b. Approving the annual health expenditure and/or allocation for the health system. Parliament/Legislature Cabinet of Ministers/Executive Cabinet Ministry/Department of Health Ministry/Department of Finance/Treasury Health Insurance Funds Regional governments Agency – quasi autonomous, please specify ________________ Other, please specify ________________ Comments/clarifications: c. Monitoring health expenditures and signaling when there is a risk of spending above the approved limit. Parliament/Legislature Cabinet of Ministers/Executive Cabinet Ministry/Department of Health Ministry/Department of Finance/Treasury Health Insurance Funds Regional governments Agency – quasi autonomous, please specify ________________ Other, please specify ________________ Comments/clarifications: d. Proposing measures for readjustment of health expenditures in order to stay within the approved limit or to limit theamount of overspend. Parliament/Legislature Cabinet of Ministers/Executive Cabinet Ministry/Department of Health Ministry/Department of Finance/Treasury Health Insurance Funds Regional governments Agency – quasi autonomous, please specify ________________ Other, please specify ________________ Comments/clarifications: e. Implementing agreed-upon readjustment measures. Parliament/Legislature Cabinet of Ministers/Executive Cabinet Ministry/Department of Health Ministry/Department of Finance/Treasury Health Insurance Funds Regional governments Agency – quasi autonomous, please specify ________________ Other, please specify ________________ Comments/clarifications: f. Ex post evaluation of expenditures with recommendsations for improving expenditure management/efficiency of the health system. Parliament/Legislature Cabinet of Ministers/Executive Cabinet Ministry/Department of Health Ministry/Department of Finance/Treasury Health Insurance Funds Regional governments Agency – quasi autonomous, please specify ________________ Other, please specify ________________ Comments/clarifications: 47 Question 84a. Is expenditure for health subject to approval in the executive budget proposal or is it authorised by permanent legislation (e.g. mandatory/entitlement expenditures)? Subject to budget approval Authorised by permanent legislation Both types of expenditure exist Comments/clarifications: Question 84b. If there are expenditures for health authorised by permanent legislation, how are they treated in the executive budget proposal? Subject to approval in the executive budget proposal Estimates included in the budget for presentational purposes Not presented in the budget Comments/clarifications: Question 85. Please provide a web link to health specific budget documents as proposed and as enacted: _______________________________________________________________ Comments/clarifications: Question 85b. Do the budgeting process and budget documents include the following (check all that apply): Budget allocation (or health expenditure ceilings) by category of health care services (e.g. hospital in-patient services, primary care, pharmaceuticals, etc….) If so, please provide the number of categories explicitely considered in the budget: ______ As well as the exact reference to the full list of categories Budget allocation to specific health objectives (e.g. cancer care, improving coordination of care) ? If so, please provide three examples of programs with significant budgets 1. ________________________________________________________ 2. ________________________________________________________ 3. ________________________________________________________ Budget allocations/transfers to lower levels of governments? Distinction between operating and capital costs in the budget for health ? Comments/clarifications: Question 86. Are the following measures likely to be regularly undertaken in response to spending exceeding targeted levels? For each row, please indicate whether this option is legally possible and whether it has occurred in the last three fiscal years. Legally Possible? Method Used in the last 3 years Supplemental budget appropriations are made Health Insurance Fund deficits increase Sub-national budget deficits increase Providers (e.g. hospital) accumulate deficits Cuts in payment rates to hospitals Cuts in health personnel wage bill Cuts in physicians’ fees Cuts in pharmaceutical prices Cuts in pharmaceutical reimbursements Cuts in the benefit package (delisting of services) Increase in patients fees/co-payments/deductibles Rationing of health services (strict budgets for providers) Claw-back requested from providers Other, please specify: ___________________ Comments/clarifications: Question 87. Is there any early warning system to prevent the risk of spending beyond the budget targets? No Yes If so, please describe the process: ___________________________________________ Comments/clarifications: Question 88. Is it possible to isolate the “health budget deficit” from general government deficit? No Yes, if so, please indicate where the information on “health budget deficit” can be found, as well as the amount of this deficit for 2011 (or latest year available)? Comments/clarifications: Note: Question 89 will only be completed by federal health systems 49 Question 89. This question will seek to understand and characterize transfers and grants to lower levels of government: 1. Does the national/central government provide sub-national levels with specific health grants? check all that apply Yes, through grants for a broad range of health responsibilities Yes, through specific grants for specific health programs and objectives No, they receive general grants (also covering health) None of the above 2. When determining the amount of transfers/grants given to sub-national governments for health, are any equalization or distribution formulas used? Select one. Yes, for all spending Yes, for some, please specify: _________________________ No Comments/clarifications: Section 3. Patient’s rights and citizens’ involvement Question 90. Is there a formal definition of patients’ rights at the national level (e.g. a patient charter)? No Yes If so, Please provide web link to charter: _____________________________________________________________ Which are the institution(s) responsible for handling reported violations against the patient’s charter? _____________________________________________________________ Are these institutions responsible for sub-national levels as well? Yes No Comments/clarifications: Question 91. Is there a formal role for citizen or patient representatives in the following areas (e.g. participation on decision-making bodies): Licensing of pharmaceuticals Yes No Coverage or reimbursement Yes No Health technology assessment Yes No Decisions relating to hospital planning (if relevant) Yes No Definitions of public health objectives Yes No Other (please specify) Yes No Comments/clarifications: 51