LaGuardia Community College Practical Nursing Program SCL 115 Maternity Child Health Nursing
advertisement

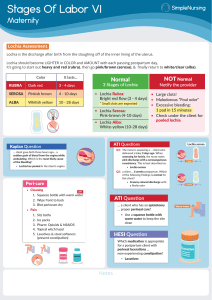
LaGuardia Community College Practical Nursing Program SCL 115 Maternity Child Health Nursing POST PARTUM OBSERVATION Direction: Complete this observation chart by writing the appropriate value, observation and nursing intervention for each of the nursing assessment areas By Anaise E. Ikama Area of Nursing Assessment Fundus Normal P. P. State Describe your observation Descend about 1 finger’s width each day after 24 hours of delivery Uterus three fingers below the umbilicus and firm Perineum Is edematous, tender, and bruised Lochia Lochia rubra (red 3 days after birth), lochia serosa (pinkish lasts 3-10 day), lochia alba (clear mucus lasts 10-21 days) Had perineal laceration of 1 degree Moderate rubra Rectal Area Is edematous, tender, and bruised Intact Breasts First 2-3 days breast are full but soft. By the third day, they become firm and lumpy as blood show increases and milk production begins Soft, non-tender Skin Hyperpigmentation of the skin Nursing Intervention Assess firmness, location and position of the uterus (below or above the umbilicus) Assess for redness (if associated with pain = infection), Edema (should be mild), ecchymosis “bruising”, discharge (no discharge from the perineum should be present) and approximation (suture line should not be separated). Teach patient comfort and hygiene measure Assess for foul odor, firmness, location and position to prevent hemorrhage. Because uncontracted uterus allows blood to flow freely from vessels at the placenta insertion site Assess for REEDA Check the woman’s breast for consistency, size, shape and symmetry. Inspect nipples for redness and cracking, flat or inverted Puffy face, dark around the Assess the skin, noticing its Bladder Abdomen G. I. Elimination Blood Pressure Temperature “chloasma”, and the linea nigra neck area, linea nigra and striae (fade from reddish to silver) Should not be characterized bulging of lower abdomen; spongy feeling mass pubis and fundus; Not distended displace uterus from the midline and increase in lochia Soft, non-tender with linea nigra Soft and non-tender; linea and striae nigra and striae Bowel sound: bursts of continuous sound every 5 to 10 seconds with a gurgling quality, representing the movement of air and fluid through the gastrointestinal tract 120mm Hg/80mm Hg Ranges from 97.8° F (36.5° Celsius) to 99° F (37.2° C). Passed flatus. Growing sound for bowel movement. Did defecate (moderate soft) 127/74 99.4 Hemoglobin 12-16 11.5 Hematocrit 37-47 33.6 VDRL (venereal A negative or nonreactive VDRL Non-reactive pigmentation, striae and linea nigra Observe for fullness, output, burning and pain Continue assessing for tenderness; normal color for linea nigra and striae Continue determining passage of flatus, bowel sounds and defecation. If client is constipated, suggest the importance of eating fibers Take BP, P, and R every 15 minutes for an hour, then every 30 minutes for an hour, and then every hour as long as the patient is stable. Report temperature above 38 C or 104 F and need to be evaluated every 4 hours for the first 24 hours Keep assessing the patient for signs of bleeding Assess patient for any type of bleeding Assess patient for sign and disease research laboratory Urinalysis is compatible with a person not having syphilis PH range from 4.6 to 8.0. For a spot check by dipstick: for Yellow, cloudy with PH of 6.5 protein, the normal values are and no protein in urea approximately 0 to 8 mg/dl. For a 24-hour test: less than 150 mg symptoms of syphilis Continue assessing urine output per 24 hours. Rh Factor Rh positive A positive; negative antibodies Assist the Rh negative mother in the administration of the Rh(D) immune globulin (within 72 hours) after giving birth to a Rh negative infant. Teach the patient about RoGAM