Thrombocythemia (Essential) – What client presentations would you see?
advertisement

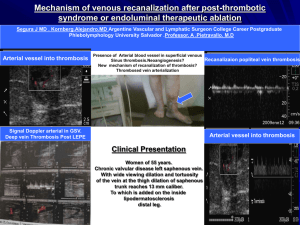
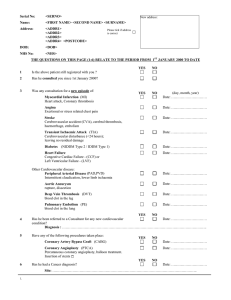
Thrombocythemia (Essential) – What client presentations would you see? (Group I – Lorna Joanna & Andria) Essential thrombocythemia (ET) is a chronic myeloproliferative disorder that causes platelets to be over produced by the bone marrow. Often this overproduction of platelets is seen on a routine complete blood count. The platelet count of ET is greater than 1000 x 103/mm3 or 1000x106/L where as the normal platelet count is 100-400 x 103/mm3 (Fischbach & Dunning, 2008). Sanchez and Ewton (2006) and Mansen and McCance (2006) cite platelet counts greater than 600, 000/ mm3 for ET. The bone marrow is “characterized as hyperplasia of megakaryocytes” (Mansen & McCance, 2006 p.983) in individuals with ET. Other clinical presentations may include an enlarged spleen, enlarged liver and periods of either or both thrombosis and hemorrhage (Mansen & McCance, 2006; Stefano, et al., 2008; Barbui et al., 2004; Sanchez and Ewton, 2006). Clinical presentations vary and ET rarely produces symptoms, yet patient’s can present with abnormal bleeding and or clotting. The Italian Society of Hematology (2004) defines major thrombosis as “stroke, transient ischemic attack, myocardial infarction, angina pectoris, peripheral arterial thrombosis, retinal artery occlusion, deep venous thrombosis and pulmonary embolism” (p. 218). Those with ET who had major thrombosis events are more likely to be over 60 years of age and have a history of previous thrombosis (Stefano et al., 2008). Microcirculatory thrombosis presenting symptoms include: vascular headaches, dizziness, visual disturbances, burning pain sensation in the palms of the hands and soles of the feet (mainly the forefoot and one or more toes), distal paresthesia and acrocyanosis (Barbui et al, 2004: Mansen & McCance, 2006: Stefano et al., 2008). Arterial thromboses are reported three times more often than venous thromboses (Sanchez & Ewton, 2006). Treatment for thrombosis is directed towards prevention of clotting and does not cure the disease. Both cytoreductive and/or antithrombotic treatments are used. ET has elevated platelet production and thus activation, with elevated levels of thromboxane A2 (TA2). The endothelial cell damage with increased TA2 are factors in the formation of platelet-rich thrombi and antiplatelet therapy is used with the rationale of controlling platelet function. Antiplatelet therapy is “recommended in patients with microcirculatory symptoms, provided that no absolute contraindication to anti-platelet therapy is present” (Barbui et al., 2004, p. 226). Cytoreductive or platelet reducing strategies include hydroxyurea, interferon, and anagrelide (Barbui et al, 2004: Mansen & McCance, 2006: Stefano et al., 2008). For further information on platelet lowering strategies for various populations, ages and those with coexisting morbidities, the reader is directed to the algorithm by The Italian Society of Hematology (2004) at http://www.haematologica.org/cgi/reprint/89/2/215 page 219. In contrast to the main presenting symptoms of thrombosis; bleeding occurs less frequently but is still a concern. Sites of bleeding occur in the skin, mucous membranes, brain, eyes, and joints and can present as nose bleeds menorrhagia and gingival bleeding. Other observed signs of bleeding are bruising. Treatment is aimed at stopping the hemorrhage, which is not often severe, and blood transfusion. Mason and McCance (2004) remind readers that ET has bleeding and clotting that co-exist simultaneously and those with ET are not necessarily only clotters or bleeders. Sanchez and Ewton (2006) report “that there is no consistent, specific, or universal recurring cytogenetic abnormality or molecular marker for ET” (p. 1146). However, a promising new molecular marker for ET involving a mutation in the janus kinase 2 gene (JAK2) located on chromosome 9p has been identified (Sanchez and Ewton, 2006). References Barbui, T., Barosi, G., Grossi, A., Gugliotta, L., Liberato, L., Marchetti, M., et al., (2004). Practice guidelines for the therapy of essential thrombocythemia. A statement from the Italian Society of Hematology, the Italian Society of Experimental Hematology and the Italian Group for Bone Marrow Transplantation. Haematologica, 89(2), 215-232. Fischbach, F. & Dunning, M. (2008). A manual of laboratory and diagnostic tests (8th ed.). Lippincott Williams and Wilkins: Philadelphia. Mansen, T. J. & McCance, K. L.(2006). Alterations of leukocyte, lymphoid and hemostatic function. In McCance, K. L., & Huether, S. E. (Eds.). Pathophysiology: The biologic basis for disease in adults and children (5th ed., pp. 955-998). Elsevier Mosby: St. Louis. Sanchez, S. & Ewton, A. (2006). Essential thrombocythemia. Achieves of Pathology and Laboratory Medicine, 130(8), 1144-1150. Stefano, V., Za, T., Rossi, E., Vannucchi, M., Elli, E., et al. (2004). Recurrent thrombosis in patients with polycythemia vera and essential thrombocythemia: incidence, risk factors, and effect of treatments. Haematologica, 93(3), 372-380.