Transforming OMOP CDMv2 to CDMv4: Broadening CER Applicability
advertisement

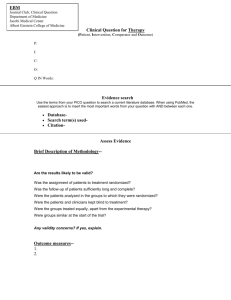
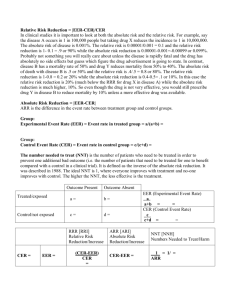
Transforming OMOP CDMv2 to CDMv4: Broadening CER Applicability Michael G Kahn, MD, 1 PhD ; 4 Brandt ; 3 MS ;Daniella 5 PhD ; 6 PhD ; Elias Patrick Hosokawa, Meeker, Lola Ogunyemi, Christian Reich, MD7; Lucila Ohno-Machado, MD, PhD8; Lisa Schilling, MD, MSPH2,3 Patrick Ryan, 7 PhD ; Department of Pediatrics1, Department of Medicine2, Colorado Health Outcomes Program3, University of Colorado Anschutz Medical Campus, Aurora, CO; American Academy of Family Physicians, Leawood, KS4;Rand Corporation, Santa Monica, CA5; Charles Drew University, Los Angeles, CA6; Observational Medical Outcomes Partnership, Foundation of the NIH7; University of California San Diego, San Diego, CA8 ABSTRACT The Scalable Architecture for Federated Translational Inquiries Network (SAFTINet) and the Scalable National Network for Effectiveness Research (SCANNER) are AHRQ-funded projects tasked with constructing distributed research network infrastructures to support comparative effectiveness research. Both projects independently selected the OMOP CDMv2 data model as the starting point for their information model and collaborated closely with the OMOP team to modify CDMv2 to the current CDMv4. The purpose of the modifications is to support a broader array of comparative effectiveness questions than OMOP’s original drug surveillance outcome focus, including those that address the impact of health care delivery system and insurance characteristics. Using a SAFTINet research question as a guide, important CDM revisions are highlighted. Distributed Health Data Network “…a system that allows secure remote analysis of separate data sets, each derived from a different medical organization’s or health plan’s records.” (2) Benefits: • • • • Data owners retain physical and logical control Eliminates need to secure a central repository Minimizes need to disclose PHI Allows local data use/access logging Scalable Architecture for Federated Translational Inquiries Network (SAFTINet) SAFTINet requirements: • Develop a distributed data network that collects and links data from multiple and different healthcare delivery settings • Clinical data from electronic health records (EHR) • Medicaid claims data • Demonstrate capabilities for conducting methodologically rigorous Comparative Effectiveness Research (CER) Comparative Effectiveness Research (CER) • CER is the generation and synthesis of evidence that compares the benefits and harms of alternative methods to prevent, diagnose, treat and monitor a clinical condition, or to improve the delivery of care. • The purpose of CER is to assist consumers, clinicians, purchasers, and policy makers to make informed decisions that will improve health care at both the individual and population levels. (1) Data Needs for CER A SAFTINet CER “use case”: • A prospective, observational comparative effectiveness cohort study to determine the effects of medical home delivery system characteristics on the control of asthma in adults and children. DELIVERY SYSTEM FACTORS + COVARIATES → Enhancing the OMOP common data model to meet the needs of CER CER Data Examples and CDMv4 Storage Locations OMOP common data model (CDMv2) • A critical first step for SAFTINet was to select a common data model that would support comparative effectiveness research (CER) • The lack of interoperability of EHR and other data sources in a multi-institution distributed data network is a challenge for CER and requires: • A flexible common data model • Mapping of idiosyncratic local codes/domains to standardized terminologies • Use of standardized terminologies for concept hierarchies & intelligent queries • The objective for this presentation is to show how the OMOP CDM V2 was enhanced to meet broader needs of CER • The new components of the OMOP CDM V4 are highlighted and linked to CER needs. Specific data elements to be included in limited dataset : Organization Information (Organization Table) Organization ID Organization name Care Site Information (Care Site and Location Tables) Care site ID Care site name (for all encounters) Care site type (for all encounters) Care site location (zip code) Provider Characteristics (Provider Table) Provider ID Provider Type Provider Specialty Provider Home Clinic OUTCOMES (chronic disease control) CER data requirements: 1. Data to identify and track a cohort of patients with a diagnosis of asthma 2. Data to characterize patients, practices, providers, and aspects of health care delivery 3. Data pertaining to health outcomes, including health care utilization, treatment, morbidity and mortality, and patient-reported outcomes 4. Hierarchies and linkages among patients, encounters, providers, practices and organizations Cohort identification criteria: 1. Patients with at least two diagnosis codes for asthma (493.XX) within any 18 month span in the prior 4 years 2. Childhood asthma: age 2-17 years inclusive 3. Adult asthma: >18 years 4. Exclusion criteria: Other respiratory conditions: specific for adults and children (not listed) Characterization of systems, practices, providers and patients 1. Patient and practice demographics 2. Domains representative of the delivery of organized and coordinated care Asthma Outcomes: 1. Poor asthma control as indicated by: An asthma exacerbation in a 6-month period, defined as: • A prescription for oral steroids (as indicated by clinical or administrative claims data), or • A visit pattern indicative of an exacerbation: 3 asthma-related visits (outpatient) occurring in 14 days or less OR asthmarelated ED visit or hospitalization 2. Patient-reported asthma control: Asthma Control Test total score < 20 (poor control) Administrative enrollment data (Payer Plan Period Table) Medication data (Drug Exposure and Drug Era Tables) OMOP common data model (CDMv4) Person Provider Location Care_site Observation_period Visit_occurrence Requirements of a CER-supportive CDM: The CDM must support the analytic availability of: • Longitudinal patient-level data • Identify/track cohorts of interest • Socioeconomic/demographic data (race, ethnicity) • Link patients & outcomes by • Place of Care and affiliated Organization • Care Provider • Geographical locations: patients, places of care • Link patients & outcomes to insurance/payer coverage data • Payers and coverage plan, benefits, enrollment periods • Link patients & outcomes to cost of care data • Drugs, procedures, visits Condition data (Condition Occurrence and Condition Era Tables) Procedure data (Procedure Occurrence Table) Organization Payer_plan_period Drug_exposure Drug_era Drug_cost Condition_occurrence OBJECTIVES Data Type (Source Table in common data model) Patient Demographic data (Person and Location Tables) Condition_era Procedure_occurrence Procedure_cost Observation • Health Outcomes of Interest • Drugs of Interest • Interventions Cohort Death Patient ID Patient Gender Patient Race/ethnicity Patient Year of birth (all patients are under age 90) Patient language of preference Patient socioeconomic status (income level as Percent Family Poverty level) Zip code of residence County of residence Insurance type and benefit plan Enrollment start and end dates All medications for patients included in the sample, for the full seven-year study period, including: Medication code (e.g., NDC code) Dose Units Dosing instructions Quantity Number of refills Prescription date Fulfillment date Associated diagnosis code Diagnostic codes from visits and problem lists Diagnostic start and end dates Associated provider Associated visit Procedure codes for procedures, including E&M, CPT, and ICD-9 PC: Pulmonary function testing Spirometry Mechanical ventilation Continuous nebulized therapy Endotracheal intubation Critical care Date procedure completed Associated diagnosis codes Results of procedure (if available) Encounter ID Encounter data (Visit Occurrence Encounter data for all primary care and specialty care Table) encounters, ED or urgent care visits, and hospitalizations, including: Encounter start date Encounter end date Encounter types Vital signs and assessments (Observation Table) Standardized Vocabulary Condition data (Condition Occurrence Table) Cohort (Cohort table) Death (Death Table) Entity Relationship Diagram Weight (including units) Height (including units) Height percentile (children) Weight percentile (children) Smoking status Pulmonary function test type and results (e.g.,FEV1 from spirometry) Medical history ACT total score ACT item response value (items 1-6) ACT completion date C-ACT total score C-ACT item response values (items 1-6) Observation date Condition data for all diagnoses (from encounters, problem list and chief complaint fields, where available) including: Diagnosis code Condition start date Condition end date Asthma cohort Date of death DISCUSSION Input from researchers, statisticians and analysts in conjunction with several research question “use cases” was used to guide CDM modifications to support broader CER applications. This input was used by data modeling experts to make final CDM revisions. Several tables (Provider, Care Site, Organization) were added in order to: (1) Support assessments of delivery system characteristics and multi-level modeling; (2) Support economic analyses (procedure cost, drug cost, and payer plan period), (3) Improve the capture of mortality information (death), and (4) Support prospective assessment (cohort) REFERENCES 1) Institute of Medicine, Initial Priorities for Comparative Effectiveness Research, June 2009. www.iom.edu/Reports/2009/ComparativeEffectivenessRese archPriorities.aspx 2) Judith C. Maro et al., “Design of a National Distributed Health Data Network,”. Annals of Internal Medicine, Vol. 151, No. 5, September 1, 2009 ACKNOWLEDGMENTS This work was supported by the Agency for Healthcare Research and Quality: R01 HS019908 “Scalable Architecture for Federated Translational Inquiries Network” (SAFTINet) PI: Lisa M. Schilling, MD, MSPH\ R01 HS19913-01 SCANNER: Scalable National Network for Effectiveness Research, PI: Lucila Ohno-Machado, University of California San Diego