Document 17696758
advertisement

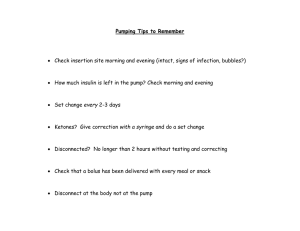
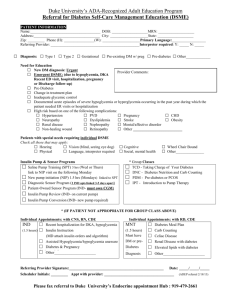
Practical Aspects of Insulin Pumping DeAnn Johnson, RN, BSN, CDE Susie Owen, RN, CDE Overview: Evidence for pump therapy Patient selection Dosing Set and site issues Pump attire Sick Days Travel Case study Discussion BDC results: 1 year pre CSI compared to ea yr thereafter HbA1c Values (1 year pre-CSII compared to each year) 9 n=291 * n=267 * n=196 † n=146 † n=105 † n=59 † HbA1c value (%) 8.5 n=34 † n=11 † 8 Pre-CSII Most Recent 7.5 7 6.5 1 2 3 4 5 6 7 8 Years on CSII *= p<0.001, †=p<0.05. The pre-CSII values for each year represent the initial values for only those with an HbA1c value in that year. Chase HP et al, Diabetes Technology& Therapeutics, 9:421,2007 Severe Hypoglycemia and Insulin Pumps (CSII) Rate of hypoglycemia (events per 100 patientyears) Figure: The Decline of Severe Hypoglycemic Events with CSII Therapy in a General Clinic Population 14 12 10 8 6 4 2 0 Pre-CSII * On CSII Pre-CSII ** On CSII * Maniatis, Chase, et al. ** Scrimgeour, Chase, et al Pediatri,107,351 2001 D T & T 9:421, 2007 (In DCCT: 62per 100 pt. yrs: NEJM, 329, 977, 1993) Who’s a good candidate? Essential Criteria for Pump Initiation Survey of 54 Diabetes Educators * All 54 respondents ranked SMBG as an essential criteria for pump start Lenhard et. al., Infusystems USA 3, 1, 2006 2007 Consensus Statement on Pump Use in Peds- Patient Selection Endorsed by the ADA & European Assoc. for the Study of Diabetes Recurrent severe hypoglycemia Wide fluctuations in bg levels regardless of A1c Suboptimal diabetes control Micro/macro vascular complications Good control but regimen compromises lifestyle Infants and neonates Adolescents with eating disorders Children and adolescents with pronounced dawn phenomenon Pregnant adolescents Ketosis-prone individuals* Competitive athletes Children with needle phobia** Battelino,P.M., Rodriguez,H.D., Kauffman, F. Use of insulin pump therapy in the pediatric age-group: consensus statement from the European Society for Paediatric Endocrinology, the Lawson Wilkins Society and the International Society for Pediatric and Adolescent Diabetes, endorsed by the American Diabetes Association and the European Association for the study of Diabetes Care Diabetes Care 2007:30:, 1653-1662 *Blackett PR: Insulin Pump Treatment for Recurrent Ketoacidosis in Adolescence; Diabetes Care;1995;18:891-892. **Maniatis AK et al, Pediatric Diabetes 2001 June;2(2):51-57. Basal Dosing Half total daily dose. May decrease by 10-30%. Divide over 24 hours Convert Lantus or Levemir dose directly into basal Set pump up in 3 hour increments Consider dilution to U50 (off label) if using <.05 u/Hr. To order diluent for Humalog 1-800-821-0538, for Novolog 1-800-727-6500 Keep timing of basal dosing in mind for disconnections Use alternate increased basals for menses, illness, steroid use and alternate lower basals for high exercise days/nights Basal Dosing Needs B and C= 708 and 83 primarily pubertal subjects D = 152 subjects F = 117 pre-pubertal subjects From Holterhus PM, et al., Diabetes Care, 2007; 30(3):568-73. Bolus Dosing Consider using “Rule of 500 (carbs) & Rule of 1700 (correction)” Bolus 15-30 minutes prior to meal Dual Wave Bolusing Change in blood glucose levels (mmol/L) 5 4 3 2-hour post-prandial 2 4-hour post-prandial 1 0 -1 1 Bolus 2 boluses Square wave Dual Wave Method of bolus administration Mean change in blood glucose levels following four methods of bolus administration. (Chase HP et al. Diab Med 19:317, 2002.) Use of the Combination or Dual Useful for all high fat/ high carb meals May add a unit to total bolus to combat decreased insulin sensitivity Starting point: Take ½ (50%) of bolus immediately and extend the other half (50%) over the next 2 hours Check bg at 2,4 and 6 hours Make > < > adjustments as needed (examples): 180* at 2 hrs. = to 60% Immediate bolus 70* at 2 hrs. = to 40% Immediate bolus 180* at 4 hrs. = to 60% Extended bolus *180mg/dl =10mmol/L Forgotten Boluses – Increase of a half point in A1c if just 2 boluses missed per week!* Use of pump alarms Cell phone alarm “Food in mouth, hand on pump!” Upside down plate Bolus for all carbs (except tx of lows) Parental review Evaluate for eating disorder *Chase HP, et al: Pediatrics 113,221,2004 Exercise Jason Johnson, a pitcher for the Detroit Tigers was diagnosed with Type 1 Diabetes when he was 11. The MLB approved use of insulin pumps during games in 2004. Exercise Dosing Disconnect for duration. Test every 2 hours minimum. May need 50% bolus predisconnection for anticipated missed basal + correction and additional corrections throughout activity. 25-75% decreased temp basal during moderate to intense extended duration activity. May start up to an hour prior. 25-75% reduction to alternate basal for delayed hypoglycemia during the night starting 2 hours prior to expected drop. Potential 25-75% decrease to bolus just prior to activity and/or immediately following. Choosing the Right Site and Set Site and Set Considerations Pinch test Hypertrophy/lipoatrophy Curves Disconnection access Diapers Activities 90 Degree Infusion Sets Cleo Inset Quick set Rapid D Sure T Angled Infusion sets Inset 30 Comfort Silhouette Tender Omnipod Minimize Pain and Anxiety Desensitization: breathing/ distraction/ visualization – bubbles, I Pod Use of inserter Use of buttock/hip Parent wears at saline start Respect rituals Maniatis AK et al, Pediatric Diabetes 2001 June;2(2):51-57. Numbing agents ice – teething rings, cold stones Gigi Waxing Spray L-M-X4 Emla crème, generic lidocaine 2.5% /prilocaine 2.5% crème (discs or use with wax paper) Where to wear? alana-mireilleapparel.com Kangaroo Pump Pockets Mypumpgear.com Pumpwearinc.com store.minimed.com Wearing the Pump Cell Phone/PDA Holders as Pump/PDM Holders Making it Stick (or not) Antiperspirant Skin Prep, IV Prep, Bard wipes Skin Tac / Tac Away Mastisol / Detachol IV3000,Tegaderm Polyskin, Water proof sports tape STR Surgical and Sports Tape Remover Sick Days Test blood or urine ketones if >300 or >240 twice Give a shot and change set if positive Increase fluid intake Use of temp basal Extra tape to site for surgery Vacations 10-50% reduction in dosages Travel letter and current dosing Take along “loaner pump” and/or basal insulin & syringes More frequent set changes