23 HIPAA (Health Insurance Portability and Accountability...
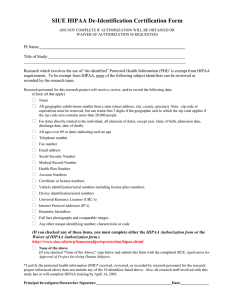
advertisement

23 HIPAA (Health Insurance Portability and Accountability Act) The Health Insurance Portability and Accountability Act of 1996 (HIPAA) required the creation of a Privacy Rule for identifiable health information. The resulting Privacy Rule, finalized in August 2002, set a compliance date of April 14, 2003. While the main impact of the Privacy Rule is on the routine provision of and billing for health care, the Rule also affects the conduct and oversight of research. Researchers, COMIRB staff and members as well as research administration must be aware of these regulations. 23.1 Historical Background The Health Insurance Portability and Accountability Act of 1996 (HIPAA) is an expansive federal law, only part of which is intended to protect the privacy of health care information. HIPAA required Congress to enact a health information privacy law by August 1999 and stated that if it did not act by then, which it did not, the U. S. Department of Health and Human Services (DHHS) must develop privacy regulations. The final Privacy Rule was published on August 14, 2002 The objective of the rule is to protect the privacy of an individual’s health care information. It creates a federal “floor” of protection so that every person in this country has at least the same basic rights and protections, though some may have additional rights depending on state law. 23.2 Effects of HIPAA on Research The final Privacy Rule published on August 14, 2002 included a number of changes in how the Rule applies to research. See the NIH HIPAA Privacy Rule Booklet for Research and the NIH fact sheet on Institutional Review Boards and HIPAA for more information on how HIPAA applies to research. See also Impact of the Privacy Rule on Academic Research, a white paper published by the American Council on Education. 23.3 Patient Rights and Research Under HIPAA, patients have certain rights. Those that may affect research include the right to receive a Notice of Privacy Practices, the right to access, inspect, and receive a copy of one’s own PHI, the right to request an amendment to one’s own PHI, and the right to an accounting of certain disclosures of PHI that occur outside the scope of treatment, payment and health care operations that have not been authorized. 23.4 Research under HIPAA Regulations Investigators that are part of a covered entity conducting research using “Protected Health Information” (PHI) must comply with HIPAA regulations. 23.5 Covered Entities The majority of healthcare schools, centers, and departments within UCD and its affiliates function as covered entities under HIPAA. The UCD - Downtown Campus is not a covered entity under HIPAA Covered entities are health plans (e.g. health insurance issuers), health care clearinghouses (e.g. healthcare billing company), and healthcare providers who electronically transmit health information in connection with eight transactions. Generally, these transactions concern DHHS billing and payment for services or insurance coverage. Covered entities can be institutions, organizations, or persons. 1 23.6 HIPAA Definitions Research - systematic investigation, including research development, testing and evaluation, designed to develop or contribute to generalizable knowledge. This definition is identical with the one used in the DHHS “Common Rule”, separate federal legislation designed to protect human subjects involved in research. HIPAA describes privacy standards for protecting PHI and so applies to research that involves humans’ health information. PHI – Protected Health Information. Health information – any information recorded about past, present, or future physical or mental health or condition of an individual, or the past, present, or future payment for the provision of healthcare to an individual. Health information may be oral, print or electronic. Individually identifiable information: o Name o Postal address (geographic subdivisions smaller than state) o All elements of dates, except year (birth date, if over 89, must be aggregated) o Phone number o Fax number o Email address o Social security number o Medical record number o Health plan number o Account numbers o Certificate/license numbers o URL o IP addresses o Vehicle identifiers o Device ID o Biometric ID o Full face/identifying photo o Any other unique identifying number, characteristic, or code PHI does not include de-identified health information. De-identified information is information that does not identify an individual and for which there is no reasonable basis to believe that information could be used to identify an individual. PHI does not include individually identifiable health information found in education records covered by FERPA (“Family Educational Rights and Privacy Act”), records described at 20 U.S.C. 1232g(a)(4)(B)(iv) (higher education student medical records) and employment records held by the University in its role as employer. Unlike the “Common Rule” regulations, HIPAA regulations also cover research involving deceased individuals. Decedent research involving PHI must be cleared through UCD’s Privacy Officer prior to implementation. The researcher must certify that the access/use of PHI is solely for research involving deceased individuals, all individuals are deceased, and the PHI is necessary for the conduct of the research through a Deceased Research Certification Form. 23.7 HIPAA and Existing Studies Human subject research protocols that were approved after April 14, 2003, must have HIPAA authorizations, a HIPAA waiver, or Data Use Agreement in place. Individuals consented or re-consented into a human subject research protocol after April 14, 2003 must sign an authorization. 2 Any research subject enrolled in a human subject research protocol that uses PHI from a covered entity must sign a HIPAA-compliant authorization form, unless a waiver has been obtained. This form is in addition to the existing Informed Consent document and is federally required. In some cases, the Informed Consent document may be combined with the HIPAA authorization. 23.8 HIPAA Documentation HIPAA documents include HIPAA Authorization Forms, a HIPAA Waiver Form, PreResearch Certification, Data Use Agreement, and Notice of Privacy Practices. 23.9 HIPAA Language / Authorization Forms Note: for VA regulated research only, the HIPAA authorization form must be separate from the informed consent document. Use and disclosure of PHI requires a valid authorization. Authorizations must contain the following elements: o o o o o o Description of PHI to be used or disclosed (identifying the information in a specific and meaningful manner) The name(s) or other specific identification of person(s) or class of persons authorized to make the requested use or disclosure. The name(s) or other specific identification of the person(s) or class of persons who may use the PHI or to whom the covered entity may make the requested disclosure. Description of each purpose of the requested use or disclosure. NOTE: Researchers should note that this element must be research study specific, not for future unspecified research. Authorization expiration date or event that relates to the individual or to the purpose of the use or disclosure (the terms “end of the research study” or “none” may be used for research, including for the creation and maintenance of a research database or repository). Signature of the individual and date. If the Authorization is signed by an individual’s personal representative, a description of the representative’ authority to act for the individual. The Authorization must include the following required statements: o o o o Notice of the covered entity’s ability to deny research-related treatment or limit enrollment in a study unless an authorization is provided to use or disclose the PHI for the research; A statement that the potential exists for information disclosed via the authorization to be subject to redisclosure by the recipient of the information and therefore no longer protected by HIPAA. The Authorization must be written in plain language. A copy of the signed Authorization must be provided to the individual signing it. A research subject may revoke an authorization at any time, provided that the revocation is in writing, except to the extent that the covered entity has taken action based on the authorization and prior to notice of revocation. If revoked, the authorization is not valid and may not be used. COMIRB is responsible for reviewing the HIPAA Authorization Forms prepared by the investigator. The wording on the HIPAA Authorization Form must contain all of the required elements and meet all other requirements as described in this section. If the language on the HIPAA authorization template has been altered, COMIRB should consult the Privacy Officer to ensure that the authorization meets all the UCD 3 requirements. If the HIPAA authorization is revised during the protocol approval period, COMIRB must review the revised document at least by the time of the subsequent continuing review. 23.10 HIPAA Waiver In some cases COMIRB may approve a waiver to use of the HIPAA authorization form. This may occur when COMIRB finds that the research could not be practically done without the waiver, and not without access to and use of the PHI, and that disclosure poses minimal risk to privacy. HIPAA waiver must be reviewed and approved COMIRB as having met the criteria described in this section. Documentation of the panel or chair determination for HIPAA Waiver must be documented using the HIPAA Waiver checklist either as a separate document or as incorporated in another checklist. In whichever format, the signature of the panel Chair or qualified voting member of the COMIRB designated by the Chair must be used to document approval of the request. For VA research only: A copy of the HIPAA Waiver checklist must be sent to the VA Research Office with the approved documents as part of the packet for R&D review. 23.11 Pre-Research Certification Researchers who need access to UCD or an affiliated hospital or research center’s medical records, databases or tissue repositories to use PHI of individuals to assess the feasibility of conducting a study, to design a research study, or to formulate a research hypothesis must submit the Pre-research Certification Form to custodian of the information to be accessed and to the Privacy Officer. PHI accessed in this manner may not be used to recruit subjects. 23.12 Data Use Agreement Researchers may use specific indirect identifiers, also known as a limited data set, through a Data Use Agreement. A limited data set removes the following identifiers of the individual, or of the relatives, employers, or household members of the individual have been removed: a) Names; b) Postal address information, other than town and city, State, and zip code; c) Telephone numbers; d) Fax numbers; e) Electronic mail addresses; f) Social security numbers; g) Medical record numbers; h) Health plan beneficiary numbers; i) Account numbers; j) Certificate/license numbers; k) Vehicle identifiers and serial numbers, including license plate numbers l) Device identifiers and serial numbers; m) Web Universal Resource Locators (URLs); n) Internet Protocol (IP) address numbers; o) Biometric identifiers, including finger and voice prints; and, p) Full face photographic images and any comparable images. A formal agreement known as a Data Use Agreement must be in place between the covered entity that holds the information and the recipient of the information. The data use agreement must identify who will receive the limited data set, establish how 4 the data may be used and disclosed by the recipient, and provide assurances that the data will be protected. The Privacy Officer should be contacted to ensure that an appropriate document is put in place. The Assistant Vice Chancellor for Regulatory Compliance is designated signature authority for UCD. If the covered entity learns that the researcher has violated this agreement, the entity must take reasonable steps to end or repair the violation and, if such steps are unsuccessful, stop disclosing PHI to the researcher and report the problem to the Privacy Officer and as needed to DHHS Office of Civil Rights. No Authorization or Waiver of Authorization is required for the covered entity to use or disclose a limited data set. 23.13 Notice of Privacy Practices UCD and/or the affiliated hospital or research center must provide its Notice of Privacy Practices to all individuals who are patients, human research participants, or enrollees in a group health plan of UCD. The principal investigator is responsible for ensuring that research subjects have received, at some time, the Notice of Privacy Practices as applicable under HIPAA. Inmates may be given the Notice of Privacy Practices document but there is no requirement under HIPAA to provide inmates with this document. 5