Crosswalk for Procedural Nursing MJRs:
advertisement

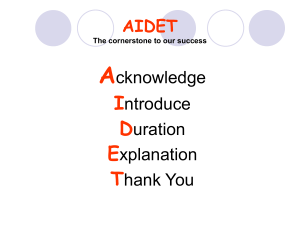
Crosswalk for Procedural Nursing MJRs: MJR: Quality and Safety for Patient Care, Documentation: 25% 1. Care plans and their implementation are completed accurately and within appropriate parameters. (5%) Holding: Intraoperative/Procedure: Care plans intraoperatively are driven by PICIS documentation. PACU/Recovery: 2. Clinical interventions are appropriate, timely and evidence based. (5%) Holding: Intraoperative/Procedure: Clinical interventions intraoperatively are driven by PICIS documentation and preference lists. PACU/Recovery: 3. Patient teaching is completed appropriately and within time parameters. (5%) Holding: Assess patient/family knowledge of the procedure, answer questions, and help reduce pre-procedural anxiety. Explains the process that both the patient and family will experience while in the Perioperative environment. Intraoperative/Procedure: Assess patient/family knowledge of the procedure, answer questions, and help reduce procedural anxiety. Explains the process that both the patient and family will experience while in the Perioperative environment. PACU/Recovery: Assess patient/family knowledge of the post procedural care, answer questions, and help reduce post-procedural anxiety. Explains the process that both the patient and family will experience while in the Perioperative environment. 4. Possesses knowledge of Core Measures, NSI and other key metrics and successfully demonstrates during patient care. (5%) 5. Meeting Unit-specific Enterprise Quality and Safety Goal (Cascade from Leadership Goal) (5%) MJR: Patient Centeredness: 20% 1. Round for outcomes on every patient according to organizational standard. (5%) Holding: Once patient is ready for surgery rounds hourly on assigned patients and checks for bathroom needs, comfort needs and updates on any delays. Intraoperative/Procedure: Once patient is in surgery, initial update and hourly updates to family are provided and documented. If surgical procedure is taking longer than scheduled, and update to the Control Desk Coordinator and the Holding Area Coordinator is provided so next patient can be informed of delays. PACU/Recovery: Once patient is settled in PACU, the family will receive and initial update and hourly update until discharged from unit, or placed in boarding status. If patient is boarding in PACU/Recovery, hourly rounding is expected which will include: positioning, potty needs, pain assessment and needs, personal comfort (blankets/Food/fluids). 2. Models behavioral expectations and demonstrates service of excellence to all customers. (5%) Holding: Anticipates the needs of all care providers and keeps them informed of any needs to get the patient ready for procedure. Communicates in a positive manner at all times. Initiates communication in order to minimize any issue and delays. Maintains awareness of the noise in the environment and works to keep it minimalized to help reduce patient and family anxiety. Keeps all personal conversations away from the patient areas. Intraoperative/Procedure: Anticipates the needs of all care providers and keeps them informed of any needs for procedure. Communicates in a positive manner at all times. Initiates communication in order to minimize any issue and delays. Maintains awareness of the noise in the environment and works to keep it minimalized to help prevent potential errors in handoff communication. Recognizes key times to reduce noise in the OR (induction, counts, emergence), and takes steps to reduce the noise during these critical times. Keeps all personal conversations away from the patient areas. PACU/Recovery: Anticipates the needs of all care providers and keeps them informed of the patient’s progress in phase I. Communicates in a positive manner at all times. Initiates communication in order to minimize any issues. Maintains awareness of the noise in the environment and works to keep it minimalized to help reduce patient and family anxiety. Keeps all personal conversations away from the patient care areas. 3. Establishes a Nurse/Patient therapeutic relationship considering the special needs of the patient and family and demonstrates foundations of service and behavioral expectations. (5%) Holding: Using the AIDET (acknowledge, introduce, duration, explanation, thank you), develop a relationship with patient and family to assess patient/family knowledge of the procedure, answer questions, and help reduce pre-procedural anxiety. Explains the process that both the patient and family will experience while in the Perioperative environment. If prior procedure is running over or patient’s surgical procedure is delayed, set expectations for rounding with both patient and family. Intraoperative/Procedure: Using the AIDET (acknowledge, introduce, duration, explanation, thank you), develop a relationship with patient and family to assess patient/family knowledge of the procedure, answer questions, and help reduce procedural anxiety. Explains the process that both the patient and family will experience while in the Perioperative environment. PACU/Recovery: Using the AIDET (acknowledge, introduce, duration, explanation, thank you), develop a relationship with patient and family to assess patient/family knowledge of the post procedural care, answer questions, and help reduce post-procedural anxiety. Explains the process that both the patient and family will experience while in the Perioperative environment. If patient is going to remain boarding in the environment, set expectations for rounding so that patient and family will know what to expect. 4. Meeting Unit-specific Enterprise Patient Centeredness Goals (Cascade from Leadership Goals). (5%) Holding: Participates in unit based activities to improve the patient experience: AIDET, hourly rounding, thank you cards, noise reduction, and behavioral expectations with all team members. Intraoperative/Procedure: Participates in unit based activities to improve the patient experience: AIDET, hourly updates to the family, thank you cards, noise reduction, and behavioral expectations with all team members. PACU/Recovery: Participates in unit based activities to improve the patient experience: AIDET, hourly rounding, thank you cards, noise reduction, and behavioral expectations with all team members. MJR: Teamwork 20% 1. Exhibits personal engagement in patient and employee satisfaction initiatives. (5%) 2. Exhibits teamwork by assisting fellow employees and working well with other departments and disciplines. (5%) 3. Fosters and models interdisciplinary team collaboration to achieve desired clinical outcomes and improve culture. (5%) 4. Demonstrate behaviors toward resolving conflict with all customers. (5%) MJR: Efficiency 25% 1. Works efficiently and completes tasks within appropriate time parameters. (5%) This includes completion of documentation, required correction of documentation, and accurate recording of patient charges. 2. Improves own work flow based on standard work. (5%) This includes throughput metrics such as on time starts, turnover times, and documentation of delays. 3. Utilizes time management effectively. (5%) 4. Resources are used appropriately i.e. supplies, equipment, and computers. (5%) 5. Reports to work on time and as scheduled. (5%) MJR: Professional Development: 10% 1. Completes all required competencies and are maintained as current by designated deadlines. Attends and participates in staff meetings or other meetings as required. Maintains certifications based on unit-specific requirements. Assumes accountability for professional development