Cancer: Psychological Factors 1
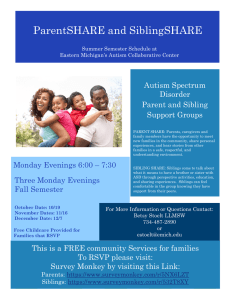
advertisement

Cancer: Psychological Factors Running head: CANCER: PSYCHOLOGICAL FACTORS Childhood Cancer: Psychological Factors and Family Relationships Jennifer Schmedes University of Evansville PSYC 490 Instructor: Dr. John Lakey 12 November 2007 1 Cancer: Psychological Factors 2 Personal Relevance Preface After I receive my Bachelor of Science degree in psychology at the University of Evansville, I plan to attend graduate school to earn a doctorate degree in clinical psychology with a specialization in health psychology. With this degree, I hope to work with children and their families who are afflicted with medical illnesses or conditions. Cancer is a particular interest of mine because of the psychological comorbidity and numerous treatment considerations involved. In graduate school, I want to study cancer from a psychologist’s perspective. I am particularly interested in parent-child relationships affected by a child receiving a diagnosis of cancer. Since a medical diagnosis can be extremely stressful for the parent or caregiver, the need for strong communication, understanding of the diagnosis, and adequate coping mechanisms is pertinent. I want to work with families to address these issues. Therefore, the objective of this thesis is to outline the major psychological factors involved with the diagnosis of childhood cancer as well as the various psychosocial variables that should be considered in treatment or therapy. Many dismiss these issues as an expected occurrence with the diagnosis of cancer, however, if left unaddressed could have serious implications, particularly for parent-child or sibling relationships. It is my aim to become more familiar with the research literature addressing these topics in order to better prepare myself for the research I would like to conduct in graduate school. Cancer: Psychological Factors Abstract It is important to view childhood cancer not only from a medical perspective, but from a psychological one as well. The psychological wellbeing of the child, their siblings and parents may all be greatly affected by the diagnosis, prognosis, treatment, remission, relapse or terminal stages of cancer. Open and early communication, maintaining normality, and adaptive coping strategies seem beneficial to the whole family. The psychosocial issues of these individuals should be considered as well, including schooling, employment difficulties, financial strain, and religious considerations. While cancer has notably many negative consequences, family members are able to identify positive aspects of the cancer experience, including a more open outlook on life, increased maturity in the child with cancer, and increased empathy and helping behaviors from siblings. 3 Cancer: Psychological Factors 4 Table of Contents Personal Relevance Preface . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2 Abstract . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .3 Table of Contents . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4 Introduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .5 Parent-Child Relationships . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .14 Sibling Relationships . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 25 Family Therapy . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .30 Psychosocial Considerations in Treatment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .32 Identifying Positive Aspects in Cancer . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .39 Conclusions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .40 References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .41 Cancer: Psychological Factors 5 Childhood cancer: Psychological factors and family relationships A parent’s first reaction to the diagnosis of their child with cancer is often characterized with complete shock, the belief that their child will die, or the inability to grasp any information given to them (Clarke, Davies, Jenney, Glasler, & Eiser, 2005). Many also felt it was a disaster and that they would not be able to get through it (Clarke et al., 2005). Cancer is undeniably one of the most stressful events a person could face in their life. Changes affect not only a child with cancer, but their siblings, parents, and family as a whole. The diagnosis, unpredictability of the prognosis, and feelings of lack of control over the illness are only a few of the psychological factors associated with childhood cancer (Houtzager, Grootenhuis, Hoekstra-Weebers, & Last, 2005). Some argue that above anything else, cancer is characterized by change; it is therefore often viewed in a developmental perspective as various critical periods or stages, including the diagnosis, treatment, remission, relapse, and for some, entry into the terminal stage (Eiser & Havermans, 1992; Kazak & Nachman, 1991). During each of these stages, different psychological factors must be considered, including how various relationships and psychosocial factors will be affected. Childhood cancer typically affects families during their early child-rearing years, with an average diagnosis at ages 3 to 4 and an average treatment span of 2 to 3 years (Kazak & Nachman, 1991). Childhood cancer was once viewed as a terminal illness; however, advancements in various medical treatments have altered this view to a chronic disease (Kazak & Nachman, 1991). The introduction of chemotherapy and radiotherapy, the centralization of care, and improved supportive care have raised survival rates to approximately 65% across childhood cancers (Eiser, 1998). Larger survival percentages have thus lead to improvements in therapeutic Cancer: Psychological Factors 6 options for families. However, the diagnoses of cancer continue to increase among children and adolescents (Cure Search, 2005). The treatment stage of cancer often involves many distressing side effects and changes that the child experiences. Alopecia, the loss of hair all over the body, was noted as one of the most distressing aspects as it leads to embarrassment of the child and tends to elicit teasing from other peers (Eiser, 1998). Children typically experience nausea and mouth ulcers due to chemotherapy, which may result in conditioned nausea at the presence of the hospital or chemotherapy related environments; disturbances in taste, resulting in food choice and eating habits seem to occur as well (Eiser, 1998). Chemotherapy can also affect sleep, resulting in moodiness and lethargy (Eiser, 1998). While symptoms from various treatments for cancer decrease once treatments have stopped, a range of late-term effects have recently been introduced (Eiser, 1998). Many of which do not get introduced to the parents as possible sideeffects, since knowledge of the susceptibility and prevalence is limited; therefore, presenting even more consequences of treatment to already distressed parents may not aid, but rather cause parents to become even more distressed (Eiser, 1998). Survivors of childhood cancer may face many difficulties as well, including physical changes, long-term psychological and educational effects, and behavioral difficulties. Long-term adverse physical consequences of cancer are numerous, including growth and endocrine functioning and fertility. Abnormal growth and dysfunction of the endocrine system are predominately associated with radiotherapy for cancer in the thyroid gland, pituitary gland, and gonads (Eiser, 1998). Radiotherapy to the central nervous system can also trigger an abnormal onset of puberty due to effects on the hypothalamic-pituitary axis (Oglivy-Stuart & Shalet, 1993). However, growth failure has also been linked to malnutrition during chemotherapy and Cancer: Psychological Factors 7 radiotherapy, since symptoms may include fatigue, nausea, painful swallowing, mouth sores, and a sore throat in specific cancers, resulting in a decrease in food intake (Haylock, 1987). Therefore, close monitoring of the patient’s weight is important because some can lose up to two pounds a day (Haylock, 1987). Over time, this could have significant health consequences. Severe growth failure may lead to the life-long use of sex hormone replacement therapy for both males and females to ensure that puberty and secondary sex characteristics will develop (Eiser, 1998; Oglivy-Stuart & Shalet, 1993). Females in particular seem to be more vulnerable to growth and endocrine dysfunction due to radiation therapy treatments in the abdomen or pelvic area (Oglivy-Stuart & Shalet, 1993). The effects of radiation therapy also seem to be dependent on the age of the child and the dosage and duration of the treatment (Oglivy-Stuart & Shalet, 1993). The evidence on the effects of cancer treatments on fertility is limited for both males and females, though some predictions have been offered. Chemotherapy, but in particular radiotherapy in the abdomen, pelvic, and gonads of both females and males, has shown fertility effects (Eiser, 1998; Oglivy-Stuart & Shalet, 1993). For females, a higher risk for miscarriages, pregnancy complications, infertility, or premature menopause seems to be present, dependent on dosage and duration of the treatment (Eiser, 1998; Oglivy-Stuart & Shalet, 1993). Infertility is also a risk factor for males who undergo radiation therapy near their gonads (Oglivy-Stuart & Shalet, 1993). Further documentation will allow researchers to determine more specific risks, including how to minimize them and who may be the most vulnerable. However, a prominent problem that exists concerning the risk of infertility for males and females is if, how, and when to tell a child those risks. Many physicians and parents do not express these concerns, possibly in an attempt to minimize distress (Zebrack, Casillas, Nohr, Adams, & Zeltzer, 2004). On the other hand, telling a patient that they may be infertile may lead to risky sexual behaviors even when a Cancer: Psychological Factors 8 small chance of fertility exists (Zebrack et al., 2004). It is therefore important to keep children informed concerning all the aspects of cancer treatment and the risks involved, but in a developmentally appropriate way. Other long-term physical consequences of cancer and treatments for cancer include cardiac dysfunction, kidney and liver damage, and damage to sensory systems. Specific anticarcinogen drugs that originally demonstrated promising results in reducing solid tumors and cancer growth have now been shown to cause cardiac toxicity (Myers et al., 1977; Olson et al., 1988). In a study, 63% of cancer survivors reported at least one physical disability or abnormality, of which 25% reported visual difficulties (Gray et al., 1992). Other long-term physical problems have been associated with the liver, lungs, and gastrointestinal tract disorders (Greene & Fergusson, 1982). These late-term effects often do not get mentioned by physicians since empirical evidence is minimal or conflicting. However, when and how to give the child and family information regarding the possibilities of these long-term effects remains in question. Besides the physical consequences of cancer and cancer treatments, cognitive impairment is another risk factor that can commonly occur due to long absences from school. However, some cancer treatments have been directly related to cognitive impairment, including cranial irradiation, surgery, and chemotherapy. Other variables include the age of the child at the time of diagnosis, the medication, dosage, and duration of the treatment as well as the type of cancer. In general, the younger the child, the greater the dosage of radiation or anti-cancer drug, and the greater the duration of treatment will increase the likelihood of a child developing cognitive impairments. Children who have Acute Lymphocytic Leukemia and solid brain tumors, which are the two most common childhood cancers, are more likely to have aggressive treatments involving the central nervous system; thus, children with cancers involving the central nervous Cancer: Psychological Factors 9 system are much more likely to experience cognitive deficits due to treatment in that area (Armstrong, Blumberg, & Toledano, 1999). Deficits typically appear 2 to 5 years after treatment has ceased and may include a one to five grade level discrepancy among peers (Peckham, Meadows, Bartel, Marrero, 1988). Attention and concentration deficits seem to be the most common cognitive factors among survivors of cancer. Other problems include poor performance in times of stress and forgetting previously learned material (Peckham et al., 1988). These deficits are more likely to be present in non-verbal intelligence tasks, but do occur in verbal intelligence tasks as well (Peckham et al.). The various cognitive impairments, depending on the severity, can be overcome with help outside the classroom as well as extra effort from the teacher once the child has returned to school (Eiser, 1998). Special education may also be utilized when needed. While impatience, frustration, and exasperation may initially exist due to the various cognitive impairments present, repeated teaching and extra patience from parents and teachers can help the child progress with time (Eiser, 1998). Most importantly, children should return to school as soon as medically possible, and while in the hospital, parents should be active in facilitating educational activities when appropriate. While it may take longer to obtain the same status of educational level as those who did not have childhood cancer, it remains possible for most. A study confirmed that long-term survivors of childhood cancer obtained an equal educational level in comparison to control groups (Stam, Grootenhuis, & Last, 2005). During the treatment and remission stages of cancer, many behavioral difficulties may be introduced. Frequent visits to the hospital or clinic may result in defiant behaviors; a lack of complete understanding of the necessity of painful and lengthy medical procedures may also result in resentment and difficulties in compliance (Eiser & Havermans, 1992). Often, children Cancer: Psychological Factors 10 who had more information concerning the necessity of the treatments were more likely to comply. Upon returning to school, children may have increased behavioral problems as well, which may be exacerbated by teasing from peers. Studies have indicated the likelihood of children becoming more sensitive and isolated when they returned to school (Vance & Eiser, 2001), possibly due to teasing or the changes inflicted by having cancer and undergoing treatment. Outside the classroom, long-term survivors have shown less risk-taking behaviors, such as less substance abuse and gambling (Stam et al., 2005). The longevity associated with cancer treatment may additionally lead to many issues associated with peer interaction and normal developmental behaviors (Kazak & Nachman, 1991). Childhood cancer survivors tend to be more cautious and sensitive in their relationships, for some resulting in feelings of dissatisfaction or difficulties initiating and maintaining relationships (Eiser, 1998; Gray et al., 1992). Difficulty maintaining relationships could also be attributed to the child with cancer having spent a great amount of time around adults for multiple years, thus increasing their maturity. Their peers may then seem immature in comparison. This maturity could then result in social isolation or withdrawal (Challinor, Miaskowski, Moore, Slaughter, & Franck, 2000). Some survivors even become resentful of a “lost childhood” (Eiser, 1998), or the period of time lost when the child could have been building relationships and friendships. However, childhood cancer survivors do show more interest in relationships than control groups and are more likely to think about other people (Gray et al., 1992). Concerning more intimate relationships, childhood cancer survivors have shown delays in psychosexual development (Stam et al., 2005), possibly due to their sensitivity and cautiousness when entering and sustaining relationships. Cancer: Psychological Factors 11 Difficulties initiating and maintaining relationships prompted an investigation on socialcomparison and survivors of cancer, which indicated that both the survivors and mothers of survivors of cancer tended to use favorable or optimistic comparisons (Eiser & Eiser, 2000). This finding however could be attributed to differences in personality and levels of self-esteem (Eiser & Eiser, 2000). Even though cancer survivors tended to use favorable social comparisons, concerns about physical appearance were still noted (Eiser & Eiser, 2000). If cancer survivors cannot achieve a favorable social comparison, they may retreat and avoid situations that may lead to unfavorable social comparisons, such as those including previous relationships or family functions (Eiser & Eiser, 2000). Since changes in physical appearance and physical limitations seem to pervade among cancer survivors, activities that involve physical activity may be avoided in an attempt to protect themselves from unfavorable social comparisons (Eiser & Eiser, 2000). In terms of psychological diagnoses, rates seem to be consistent with the national average (Butler, Rizzi, & Bandilla, 1999). This conflicts with many preconceived notions that having cancer as a child makes that person more likely to receive a psychological diagnosis, such as post traumatic stress disorder, major depressive disorder, or generalized anxiety disorder. However, there are notable psychological consequences of childhood cancer, such as anxiety, distress, and withdrawal, but are typically described as situational (Butler et al., 1999). Major life-style changes, self-esteem issues (Eiser, 1998), and delayed development concerning their autonomy when compared to same-age peers (Stam et al., 2005) have also been apparent. The ways in which children cope is particularly important during the long period of stress associated with cancer. When children evaluate the stressful situation they are in, they are more likely to use problem-based coping in times of a higher perception of control, whereas they are more likely to use emotion-focused coping in times of a lower perception of control (Sorgen & Cancer: Psychological Factors 12 Manne, 2002). Children seem to experience less distress when these models are used (Hampel, Rudolph, Stachow, Lab-Lentzsch, & Petermann, 2005) in comparison to using problem-focused coping in times of a perception of less control. This ability to perceive control over a situation and apply coping skills seems to increase with age (Sorgen & Manne, 2002). Also, in this particular study, no child showed clinical signs of distress, which confirms previous research (Butler et al., 1999; Sorgen & Manne, 2002). Sorgen and Manne (2002) found that stressors typically involved school or hospital-related topics; not being to able to apply the perceived correct coping skills to a situation seemed to be related to even more stress. Therefore, health care providers should aid in a child’s perception of control and attempt to expand problemfocused coping to more issues, which in the end would be more beneficial for the child. However, an attempt at using problem-focused coping in situations perceived as more out of the child’s control may result in failure (Sorgen & Manne, 2002); over time, this could be particularly detrimental toward the child. Overall, children with cancer do seem to have better adaptive coping responses in comparison to healthy controls and greater situational variability in coping (Hampel et al., 2005). Surprisingly, Grootenhuis and Last (2001) found that entering a stage of relapse or second diagnosis did not alter previously used coping strategies. Therefore, a perceived increase in the uncontrollability of the situation did not alter cognitive control strategies, which illustrated continued resilience (Grootenhuis & Last, 2001). While entering a stage of relapse typically indicates a decreased chance of survival, defensiveness and remaining optimistic were still indicated by those children (Grootenhuis & Last, 2001). Grootenhuis and Last (2001) suggested that the use of optimism did not seem to be correlated with denial-like control strategies, which would be constant across the prognosis; therefore, the continued use of optimism could be Cancer: Psychological Factors 13 related to resilience. In general, children with cancer use more positive self-instructions in situations involving active coping in comparison to children with other chronic illnesses (Hampel et al., 2005). In the terminal stage, the parents, well siblings, and the child with cancer must prepare for bereavement. When curative efforts fail, parents may turn to more aggressive treatment options as a last resort, often resulting in even more pain and distress experienced by the child in their last weeks or months of life (De Graves & Aranda, 2005). Health care providers note that children are nearly always offered further treatment options, even when these would be medically unrealistic (De Graves & Aranda, 2005). These more aggressive treatment options could be substituted for palliative or hospice care, which would ease suffering for not only the child but the family as a whole. However, discontinuing curative efforts may diminish hope; therefore, integrating palliative care throughout the course of cancer treatment may be more beneficial than introducing it at the end of the child’s life (De Graves & Aranda, 2005). De Graves and Aranda (2005) argued that hope is the most important foundation throughout all of the stages of cancer, including the terminal stage. The continuation of fostering hope during this time is important in order for the family to not feel abandoned during what would be the most stressful and upsetting stage of cancer (De Graves & Aranda, 2005). Unfortunately, during the terminal stage children may experience an increase in physical symptoms, such as pain, possibly due to aggressive treatment options. Thus, the most important needs for the child become adequate pain control and symptom management, in an attempt to make this stage of cancer less difficult (Jones, 2006). Also, many children who have entered the terminal stage of cancer die in critical care settings when hospice services could have been utilized. Hospice centers are also Cancer: Psychological Factors 14 more likely to address psychosocial needs by providing counseling and support services; ideally, these services should continue after the child has died (Jones, 2006). During the terminal stage, it is also important for the child to receive age-appropriate information regarding what is happening and to retain the ability to participate in decisionmaking situations (Jones, 2006). Adolescents in particular seem to need a sense of personal control (Jones, 2006). Attempts to gain a greater sense of self and autonomy are common feats for adolescents, which could potentially be affected by having cancer (Freyer, 2004). With respect to this, physicians and parents often do consider the adolescent’s wishes in continuing or discontinuing treatment, regardless of their legal status (Freyer, 2004). Temporary life-sustaining treatment, instead of palliative care, is at times used for survival goals, such as graduation, school dances, and other important school functions (Freyer, 2004). Granting these wishes instills the adolescent with a sense of control and purpose in their remaining time. Parent-Child Relationships While the child is directly affected by cancer and the associated treatment regimens, parents are considerably affected as well, though indirectly. A parent must first rely and trust medical personnel in order to begin treatment for their child (Eiser & Havermans, 1992). This requires parents and doctors to remain open and honest when communicating in order to maximize the wellbeing of the family and minimize concerns and incorrect preconceived notions about cancer (Eiser & Havermans 1992). Quality and honest communication between physicians, parents, and children at the beginning of treatment can then continue throughout the course of the child’s cancer, making transitions between stages easier than if they were based on minimal communication (Freyer, 2004). However, it appears that parents do not always view their child’s illness the same way that medical personnel do. For instance, parents tended to be more Cancer: Psychological Factors 15 optimistic about their child’s prognosis than the medical staff, regardless of medical information provided concerning the child (Eiser & Havermans 1992). This could then affect the knowledge of the child in perhaps a beneficial or detrimental manner. The source of this information typically differs among children as well, oftentimes depending on the age of the child. The majority of children received their diagnosis from a physician after the age of five; whereas children younger than five were typically told by their parents (Eiser & Havermans, 1992). This is important because the number of sources for a child appears to make a difference in the child’s affect. In this sense, the greater number of sources of information equates to a greater number of social supports (Eiser & Havermans, 1992). However, some children may also seek information from as many people as possible in order to compare the information they were given, which may result in conflict if their parents gave them minimal or less factual information. Eiser and Havermans (1992) noted that following the initial diagnosis, children quickly made good-bad distinctions, which could have been incorrect depending on their source. This may include the integration of information from various medical staff, other children, or the television. Parents should therefore be aware that children may know more than what the parents perceive and by disguising their emotions and giving minimal information, children can oftentimes sense this and act accordingly. Communication is therefore an important factor in parent-child relationships concerning cancer. Clarke et al. (2005) identified four main ways in how parents communicated with their children—through the use of optimism, realism, pessimism, and factual information. When utilizing optimism, parents communicated by telling their child that medicine will help them get better (Clarke et al.). If parents used realism to communicate with their ill child, they may have stated for instance that the medication will hopefully make them better, but that some unpleasant Cancer: Psychological Factors 16 side effects may occur, such as the loss of hair or nausea (Clarke et al.). When pessimism was used, parents eliminated the positive aspects of the medicine and only mentioned the negative, such as that the medicine will make the child feel ill (Clarke et al.). For example, one parent in the study said: “I have told her that her life depends on this (medication) and to not do it is just plain daft’” (Clarke et al., 2005, p. 277). The use of factual information refers to educating the child about the names of the medications the child is taking or when to take the medication; however, this form of communicating still lacks what the medication does and why it is important for the child to take it. The age of the child may influence through what manner the parents decide to communicate with their child. Typically, the older the child, the more factual information was given, including a clearer time frame of how long the treatment may last (Clarke et al.). The amount of detail revealed to the child with cancer also differed among parents. Clarke et al. (2005) identified four communication styles for parents, including the use of minimal information, ambiguous information, factual information, and full information. Parents who used a minimal information communication style typically concealed the severity of the disease in fear of causing more anxiety in the child (Clarke et al.). Those who were characterized with an ambiguous information communication style told their child that they had leukemia for instance; however, they did not mention that leukemia was a type of cancer (Clarke et al.). This may be an attempt to shield the child from pre-conceived notions that cancer equates to inevitable death. A third communication style was the use of factual information, such as the diagnosis of cancer, but still concealing information pertaining to the severity of the prognosis. Unlike the first three communication styles, parents who used a full information communication style did reveal the severity of the cancer and the possibility of death. Clarke et al. suggested that Cancer: Psychological Factors 17 parents who described themselves as shocked were more likely to use a full information communication style, telling the child everything that they themselves understood. A full information communication style should be cautioned in use since a child’s knowledge of their own mortality may have significant emotional consequences, possibly resulting in ineffective coping (Eiser & Havermans, 1992). In general, more information was provided when children were experiencing symptoms in comparison to those who were not experiencing adverse sideeffects (Eiser & Havermans, 1992). Also, providing more information about the etiology of cancer may effectively reduce self-blame among children diagnosed with cancer (Eiser & Havermans, 1992). The amount of information and the manner in which it is given seems to be affected by the age of the child. In general, a full information communication style was used for older children (Clarke et al., 2005). Older children were also more likely to receive information regarding how the treatments work and how they may feel at various stages. For younger children, such as in preschool, some parents argued that it was impossible for children at that age to understand the situation and therefore chose to conceal information (Eiser & Havermans, 1992). Also, the use of analogies or metaphors is a common communication method utilized by parents of children with cancer; however, the use of metaphor may not be age appropriate and therefore would not be effective (Eiser & Havermans, 1992). Also of importance is that age and time of the initial diagnosis is associated with better adjustment; children who were informed of the diagnosis within the first year as well as children who were six years or older were better adjusted than others (Eiser & Havermans, 1992). Furthermore, observation studies have described children’s ability to acquire knowledge and make inferences by observing and assessing their environment. This is important to consider, Cancer: Psychological Factors 18 especially if children are given very little information about their condition and proposed treatment schedule. These children could then pick up cues from various adults or other children with cancer and may create a wrong impression of their own prognosis. If parents are masking their feelings, children may sense this and experience more anxiety than if they had an open conversation about cancer and the child’s prognosis (Eiser & Havermans, 1992). Children have been found to be better adjusted if they were directly informed about information regarding cancer, treatment, and their prognosis in comparison to children who learned information by eavesdropping (Eiser & Havermans, 1992). Also, if children sense that their parents are covering up their emotions, the child may interpret this as more serious than it may be and mask their own emotions as well, leaving parents to believe that they are simply not aware or have no interest in what is happening, despite that the child may be completely fearful or lonely (Eiser & Havermans, 1992). In general, the more open communication that existed in the family, the less defensiveness and greater self-esteem the child exhibited (Eiser & Havermans, 1992). Children in families with open communication appeared to have less maladaptive coping responses as well (Murray, 2001). Communication was also predictive of psychosocial adjustment, despite the severity of the diagnosis or treatment regimens (Eiser & Havermans, 1992). However, there is some variability as some children who lack information concerning their diagnosis were better adjusted than those who had adequate information about cancer (Eiser & Havermans, 1992). Overall, there appears to be a fine line between how much information is too much, but it is important to consider the needs of the child as well. More specifically, 44% of participants felt they did not receive enough information regarding cancer and their treatment (Gray et al., 1992). An open relationship among family members could ameliorate this. Cancer: Psychological Factors 19 Concerning the care for the ill child, mothers tend to assume the primary role, while fathers often assume care for the other siblings. This could ultimately result in inconsistent treatment of the ill child and well siblings (Horwitz & Kazak, 1990). Furthermore, this separation could then affect the relationship of the mother and father, who no longer have a combined role in all their children’s lives, possibly contributing to the reportedly high rates of loneliness among parents of children with cancer (Eiser, 1998). Because mothers involve most of their time in the ill child’s life, they become more involved with medical staff and less involved with other social obligations; on the other hand, fathers tended to have competing obligations between family and work and may become disconnected from medical staff (Kazak & Nachman, 1991). Gender roles may switch as well. Since mothers of children with cancer tend to become the primary caretaker of the child, the father may be left with responsibilities that were previously assigned to the mother. For instance, the father may become more involved in cooking and doing other household chores while the mother busies herself with caring for their ill child (McGrath, Paton, & Huff, 2005). This separation may lead to differences in coping. Interestingly, mothers have been found to describe their ill and well children as more alike (Eiser & Havermans, 1992; Horowitz & Kazak, 1990). Horowitz and Kazak (1990) suggested that this could be a form of adaptability, choosing to believe that their children were more alike in order to downplay the impact of the cancer on the child. This illustrates how reinterpretation could be used as a coping strategy for mothers (Horowitz & Kazak, 1990). Kazak and Nachman (1991) identified differences among mothers and father’s coping: while fathers tended to score higher on denial measures, mothers tended to utilize religion and information seeking to cope. The use of religion as a coping mechanism from only one parent seems to be beneficial; however, information seeking as a Cancer: Psychological Factors 20 coping mechanism from only one parent seems to be detrimental toward the parental relationship (Goldbeck, 2001). Also, McGrath et al. (2005) found that males tended to be less likely to talk about their feelings and more likely to vent through physical activity, such as sports. However, it should be cautioned in generalizing this to the population due to the small sample size in the before-mentioned study. Older parents appear to cope better than younger parents; however, despite age, once a year has lapsed from the child receiving the initial diagnosis of cancer, parents typically begin to feel better (Kazak & Nachman, 1991). Of important note is that a mother’s coping has been reported as one of the most important factors in a survivor’s adjustment (Eiser, 1998). Social support is important in coping as well. Overall, there appears to be a positive relationship between support-seeking coping and perceived support in both men and women concerning anxiety (Norberg, Lindblad, & Boman, 2006). More specifically, parents reported that perceived support was more influential than support-seeking behaviors (Norberg et al., 2006). However, support-seeking behaviors seemed to be more important for mothers in regards to anxiety and were therefore utilized more often than by males (Norberg et al.). Norberg and colleagues also suggested a reciprocal relationship between support-seeking behavior and mood; they furthermore stated that support-seeking behavior may be dependent on different mood states. Interventions should therefore focus on improving the person’s perception of support from others (Norberg et al.). During all the stages of cancer, parental changes are likely to occur, including tolerance and discipline. As parental emotions flux, this may result in a decrease of parental tolerance and an increase in parental expectations (Shapiro & Brack, 1994). Shapiro and Brack (1994) noted that emotions change frequently for both parents and children along with changes in prognosis Cancer: Psychological Factors 21 and treatment regimens. However, there does not appear to be a difference between parental discipline of mothers of children with cancer and those with healthy children (Jelalian, Stark, & Miller, 1997). There were non-significant results comparing these two groups in the following discipline strategies: positive reinforcement, punishment, rationalization, and giving in (Jelalian et al., 1997). Consistent with previous research, there were significant results pertaining to more conflict concerning discipline, feeling less in control of situations requiring discipline, and less consistency in discipline (Jelalian et al.; Shapiro & Brack, 1994). In general, studies on parental discipline are difficult to generalize as they often rely on self-report measures or interviews. In the face of the interviewer, the parent may want to appear as a competent disciplinarian and thus affect overall findings (Jelalian et al., 1997). While it appears that parenting styles remain constant with children diagnosed with cancer, the severity of the prognosis and treatment may affect conflict as well as disciplinary styles; in this study however, parental discipline was investigated during the diagnosis stage of the child and thus can only be generalized toward mother-child relationships in the diagnosis stage (Jelalian et al.). Jelalian and colleagues suggested that parents may act more lenient when their child is experiencing physical symptoms and then maintain typical discipline when the child felt better. Also, many mothers noted their understanding of the importance of maintaining discipline as suggested by health care professionals (Jelalian et al.). It is therefore important for health care providers to acknowledge worries about disciplining their ill child, while encouraging the most normalcy as possible, which means the use of consistent discipline whenever possible. Difficulties may arise in particular with adolescents. Since disagreements are typical between adolescents and their parents, this may prove to be more difficult if an adolescent has been diagnosed with cancer (Kazak & Nachman, 1991). Oftentimes, this involves refusal of Cancer: Psychological Factors 22 treatment, and since some adolescents are considered legal on some terms, their choice to refuse treatment cannot be challenged in court (Blotcky, Cohen, Conatser, & Klopovich, 1985). In an attempt to predict refusal among adolescents, Blotcky and colleagues (1985) investigated common factors among adolescents who refused treatment, as well as their mothers, and compared them to adolescents who did consent to treatment. The adolescents who refused treatment scored higher on trait anxiety and external locus of control measures but lower on state anxiety and subjective distress measures; their mothers scored higher on religiosity and trait anxiety in comparison to mothers of children who consented to treatment. Interestingly, there were no differences between family satisfaction, hopelessness, satisfaction with their physician, the mother’s coping or the mother’s state anxiety. Adolescents also offered explanations for their refusal, of which the primary reason was fear of how they would look (Blotcky et al.). Other factors included fear of their friends’ reactions, side effects of the treatment, and painful medical procedures (Blotcky et al.). Despite having at least one other person try to convince the adolescent to consent to treatment, all of the participants still believed their chances of survival were “excellent” or “good” (Blotcky et al.). These results suggested that adolescents who refused treatment believed the situation was out of their control, which could also be explained by the mothers’ scores since their reports of religiosity and trait anxiety were high (Blotcky et al, 1985). Also, it does not seem that using scare tactics to get adolescents to consent to treatment will aid, but rather worsen the situation (Blotcky et al.). Offering more information concerning the negative consequences of cancer may escalate their already high levels of anxiety; therefore, programs that seek to decrease anxiety among adolescents who refuse treatment may result in more adaptive responses to cancer treatment (Blotcky et al.). Cancer: Psychological Factors 23 Parent-child relationships before the diagnosis of cancer can also predict the quality of life of the child once in remission. Orbuch, Parry, Chesler, Fritz, and Repetto (2005) suggested that high-quality parent-child relationships before the child was diagnosed with cancer predicted the child’s well-being in the future, particularly concerning psychological well-being. The researchers additionally found that the quality of the spiritual domain in the child’s life positively correlated with parent-child relations (Orbuch et al., 2005). The psychological and spiritual elements of one’s life may have been altered by the parent-child relationship since these areas are associated with how people think, question, and adapt to life (Orbuch et al.). On the other hand, no relationships were found between medical fears and the physical well-being of the child and parent-child relationships (Orbuch et al.). This may be because medical fears and worries concerning the body may be realistic, rational fears given the hardships associated with cancer (Orbuch et al.). Gender differences did exist in this study. While mothers were only significantly associated with psychological well-being, fathers were significantly associated with psychological, social, and spiritual well-being (Orbuch et al., 2005). Interestingly, the survivors of cancer reported higher quality relationships with their mothers than their fathers (Orbuch et al.). Mothers may have taken precedence simply because of the amount of time spent with the child, as they tend to spend more time with the child during treatments and overall care (Clarke et al., 2005; Orbuch et al.). However, the importance of the changes seen in the father-child relationship should not be overlooked. The researchers suggested that fathers may have engaged in non-normative or non-stereotypical roles due to their child’s diagnosis of cancer, which consequently may have improved their relationship with their child (Orbuch et al.). Age was not a factor in this study either, suggesting generalizability toward all age groups. Cancer: Psychological Factors 24 Parents also differed in how they felt about medical treatments. Since mothers tended to be the primary figure in the child’s care, they may have felt that they do not get enough support from their husbands or partners (Clarke et al., 2005). Many however felt that over time the treatment and schedules of treatment became easier (Clarke et al.). On the other hand, many did feel an extreme responsibility associated with the regimented schedule of treatments for the child; this is turn resulted in responses associated with anxiety and fears that they would forget to do something (Clarke et al.). However, once treatments ceased, parents were often confronted with stress and fears of the child relapsing (Eiser, 1998). This may occur because treatment schedules are at times the only controlled aspect in childhood cancer; when this ends, the parents are faced with a period of uncontrollability again (Eiser, 1998). Besides the parent-ill child relationship, it is important to address the parent-well child relationship, since changes typically occur here as well. Overall, it seems that parents generally spend less time with their well children as time-consuming demands for the child with cancer increase (Shapiro & Brack, 1994). Well children may then have to spend more time with parental substitutes, such as other family members, neighbors, or friends (Shapiro & Brack, 1994). Shapiro and Brack (1994) noted that parents reported concerns for their well children and their loneliness, fears and neglect now that the child with cancer received much of the attention. However, well siblings may be left at home as an attempt to have a “normal” life while parents spend their time at treatment facilities (Shapiro & Brack, 1994). Shapiro and Brack (1994) noted that this situation could be worse with families who live in rural areas and have to travel long distances for treatment. Thus, sibling relationships can also be affected by a child having cancer. Cancer: Psychological Factors 25 Sibling Relationships Predictability of how siblings will react to the diagnosis of their sibling with cancer depends on many factors, some of which remain unknown (Houtzager et al., 2005). Kazak and Nachman (1991) reported that themes of loss and change often describe siblings of those diagnosed with cancer. Common emotions include: fears of becoming ill, anxiety, anger, and guilt, all of which were reported as needed to be hidden from parents (Havermans & Eiser, 1994; Houtzager et al., 2001; Kazak & Nachman, 1991; Shapiro & Brack, 1994). Shapiro and Brack (1994) noted that siblings worried when their ill siblings fell, appeared sick, or unhappy. Younger children in particular may experience these feelings yet lack the ability to verbalize what may be bothering them (Eiser & Havermans, 1992). In a study, the majority of siblings reported their biggest worry was that their sibling would die (Havermans & Eiser, 1994), indicating some understanding of the seriousness of the situation. Little research has concentrated on how siblings learn about cancer and how their parents attempt to keep them informed on their ill sibling (Eiser & Havermans, 1992). A majority of siblings receive information from their parents, although some indicated a desire to talk with a physician (Havermans & Eiser, 1994). However, Havermans and Eiser (1994) found that while most children are told the diagnosis of their sibling, none were informed on the prognosis or possible side-effects. In retrospect, some siblings indicated they would have wanted more information, but did not want to bother their parents (Havermans & Eiser, 1994). Because of the amount of attention focused on the child with cancer, siblings may also feel isolated and less important than their brother or sister (Eiser & Havermans, 1992; Kazak & Nachman, 1991). Well siblings noted that they spent less time with their ill sibling as well (Shapiro & Brack, 1994). This may even turn to jealousy over the amount of time their parents Cancer: Psychological Factors 26 spent with their ill brother or sister (Kazak & Nachman, 1991). As attention shifts toward the sibling with cancer, this may in turn result in sibling rivalry (McGrath et al., 2005). Making the well sibling feel important or special therefore seems to abate the rivalry or lack of attention they receive (McGrath et al.; Shapiro & Brack, 1994). Eiser and Havermans (1992) stated that siblings specifically with adaptational problems were more likely to perceive themselves as being ignored, unwanted, misunderstood, isolated, or that no one was there to listen to their fears and concerns. Houtzager and colleagues (2005) attempted to predict well sibling coping and functioning in a study by comparing parental reports of their children before diagnosis and self-reports of functioning and coping after the diagnosis was given. This study had some limitations however, such as using information provided after the diagnosis of their child that was based on information prior to this period. Approximately 40% of children who had emotional and behavioral difficulties prior to the diagnosis of their sibling exhibited serious problems with adjustment, which required psychosocial care; however, only 2% of children without emotional or behavioral difficulties prior to the diagnosis of their sibling showed serious adjustment problems after their sibling was diagnosed (Houtzager et al.). This illustrated the possible predictability of how siblings will react when faced with an extreme stressor and change in their life, such as the diagnosis of their sibling with cancer. Therefore, this knowledge could be beneficial in developing programs or services to help prevent or treat adjustment and coping difficulties in siblings at risk (Houtzager et al.). When compared to their peers, Houtzager and colleagues (2005) found that siblings aged 7-18 experienced more cognitive and emotional difficulties. Approximately 50% of siblings reported negative feelings such as anger, jealously, sadness, and fear; a majority of siblings also Cancer: Psychological Factors 27 noted the absence of positive feelings such as cheerfulness, enthusiasm, happiness, and selfconfidence (Houtzager et al.). Additionally, siblings aged 7-11 noted more motor difficulties than their peers, such as in walking, running, playing, and overall changes in stamina (Houtzager et al.). These characteristics may have resulted from distress due to their sibling’s diagnosis or worries concerning their own health (Houtzager et al.). In general, those siblings who remained positive adjusted better to their sibling’s illness and maintained a better sense of control (Houtzager et al., 2005). Adjustment to their ill sibling’s diagnosis may also be better predicted by their beliefs and attitudes rather than their overall knowledge of cancer (Eiser & Havermans, 1992). Siblings who asked more questions about their sibling’s illness and who wanted to understand cancer better were more likely to experience fewer positive emotions (Houtzager et al.). Children and adolescents who attempted to understand their sibling’s situation by asking more questions may have experienced less positive emotions because by asking more questions about cancer, this may have led to more negative information received. This could potentially be controlled if parents are present when siblings receive information concerning cancer as well as their brother or sister’s diagnosis or in how much information parents decide to disclose to their children (Houtzager et al.). Health care providers should be cautious of early signs of somatic or psychosocial difficulties, as these could predict later functioning difficulties and more negative emotions (Houtzager et al.). Early detection of poor coping skills is equally important in identifying those at risk for maladaptive coping strategies (Hampel et al., 2005). Houtzager, Grootenhuis, and Last (2001) examined control strategies in siblings of those diagnosed with cancer. In general, the researchers found that siblings of children with cancer were highly dependent on secondary control strategies, which are attempts to gain control of the Cancer: Psychological Factors 28 situation by adapting to the environment without regard to the child’s actual preferences. These are also known as cognitive control strategies (Grootenhuis & Last, 2001). In order to gain control, the sibling typically employed one or more of the following cognitive control strategies: optimism, wishful thinking, the belief that medical caregivers had the ultimate power over the situation, and adequate interpretation of emotion (Grootenhuis & Last, 2001; Houtzager et al., 2001). Lack of control is usually expressed through anxiety, so group therapy was provided in this study for siblings of those diagnosed with cancer to address anxiety, feelings of lack of control, and how to improve their control strategies (Houtzager et al., 2001). Siblings were assessed before and after five group meetings, which showed a decrease in overall anxiety (Houtzager et al.). The siblings may have achieved this through gaining knowledge about family relations, being able to share their experiences in a common environment, and by being educated about the illness and treatment (Houtzager et al.). A major perceived advantage of the group was that siblings of those diagnosed with cancer were able to discuss matters that they did not feel comfortable discussing at home or with their parents; the group therapy therefore provided an outlet for this (Houtzager et al.). Gender differences did exist in this study. While boys had relatively high levels of anxiety before the group, these levels reduced to normal levels of anxiety after participation; however, the girls’ levels of anxiety were slightly higher than that of the boys after participation (Houtzager et al., 2001). This may be explained by the limited number of participants or a lack of control group in the study. Differences between the siblings of a child with a tumor and siblings of a child with either leukemia or lymphoma were also apparent. The siblings of children with leukemia or lymphoma exhibited a greater decrease in anxiety levels, which showed how the Cancer: Psychological Factors 29 type of cancer could be a variable in treatment options. Houtzager and researchers concluded that this difference may be attributed to the greater uncertainty of survival for a child with a tumor, which thusly affects anxiety levels and feelings of control. On the positive side, children expressed that they enjoyed the group and wished it met more often, finding it reassuring to be with other children who were experiencing the same emotions (Houtzager et al., 2001). The siblings may have also felt special because their parents were now going to the hospital for them instead of their ill sibling, which may have contributed to the decrease in feelings of isolation (Houtzager et al.). Other attempts have been made to give attention toward the siblings of children with cancer. Retreats and summer camps for families with children with life-threatening illnesses have become increasingly popular within the past decade. The positive aspects of these experiences are numerous; however, one essential advantage of having these retreats is that children who need medical supervision often cannot attend other summer camp programs, whereas they can with summer camps specifically designed for children who need constant medical supervision. These allow families to spend quality time with one another and often attempt to increase communication, education and a sense of normalcy in their lives. Wellisch, Crater, Wiley, Belin, and Weinstein (2006) investigated children with cancer who went on a one week summer camp retreat with their siblings. The siblings reported no significant affective changes after the camp, while the patients did (Wellisch et al., 2006). The positive affective changes did not occur immediately after camp, but rather four to six months later (Wellisch et al.). This could be attributed to outside factors, but the affective changes indicated after a period of time are important for future program design considerations. For both the patients and siblings, pleasurable memories about the camp were retained four to six months later (Wellisch Cancer: Psychological Factors 30 et al.). Also of note was that twelve campers, including six siblings and six patients, indicated suicidal ideation (Wellisch et al.). Importantly, they were able to engage in the camp activities, and the researchers recommended that children who have cancer or siblings of those with cancer who exhibit signs of suicidal ideation should be encouraged to go to camp as it could possibly aid in their depression or low self-esteem. In another study that utilized summer camps, Murray (2001) investigated the self concepts of siblings of those with cancer. In comparison to controls, the siblings’ self-concepts were higher after the camp ended, as measured by the Personal Attribute Inventory for Children (Murray, 2001). This suggests that activities designed specifically for the siblings of children with cancer may be useful by providing social support, thus increasing their self-concept (Murray, 2001). In comparison to the previously mentioned study, perhaps this summer camp, which only had well siblings as participants, was better able to address the needs of siblings in comparison to a camp for both cancer patients and their siblings. Also, early identification of children with low self-concepts could benefit from programs designed by psychologists or implemented by pediatric nurses to address these issues (Murray, 2001). Family Therapy If a child receives the diagnosis of cancer, this inevitably affects the family dynamic in many ways. Undue stress, anxiety, control issues, and adjustment difficulties are merely a few of the issues that arise during the diagnosis and unpredictability of the prognosis and treatment for the child with cancer. It should be noted that there are many disease variables that can also impact the family system as well, such as the type of cancer and the amount of hospitalizations (Kazak & Nachman, 1991). Because cancer affects the entire family, family intervention programs may be more beneficial than individual counseling services. Unlike individual therapy, Cancer: Psychological Factors 31 family interventions can focus on strengthening parent-child and sibling relationships, as highquality parent-child relationships have been associated with a greater quality of life for cancer survivors (Orbuch et al., 2005). Interventions could also focus on improving mother-child and father-child relations concerning emotional connection and openness (Orbuch et al.). However, using stereotypes of mothers as the primary nurturer should be disregarded as counseling efforts should focus on improving both the mother and father’s adjustment and resilience concerning their child (Orbuch et al.). Overall, it appears that family cohesiveness predicts positive adaptive responses from family members (Murray, 2001). Providing therapy for a family must encompass all the environments that affect overall functioning. These various environments, from a social ecological approach, are symbolized as concentric rings. The child is represented as the central ring, which means that the child may influence the various environments or vice versa (Kazak & Nachman, 1991). When caring for a child with cancer, of particular importance are the rings representative of the family, social support, and health care systems (Kazak & Nachman, 1991). How these systems interact with the child is therefore a crucial factor in providing therapy for the family. Concerning control strategies for families, Kazak & Nachman (1991) stated there is a lack of research, including strategies that address anxiety other than that felt due to painful medical procedures. This is important since children may mirror the anxiety of their family members (Kazak & Nachman, 1991). Interventions to address anxiety among family members may therefore be beneficial and need to be further investigated. There has however been a study to specifically address control strategies in sibling relationships, which was beneficial in reducing anxiety (Houtzager et al., 2001). Cancer: Psychological Factors 32 While developing intervention programs is one issue, the feasibility of these programs is yet another that should be addressed. Svavarsdottir and Sigurdardottir (2005) investigated the practicability of offering a family intervention program to parents of children with cancer. This included a website with educational information, guidance, and a blog for open communication and support interviews. All of the parents in the study were thankful for the interview, which allowed the parents to express themselves freely (Svavarsdottir & Sigurdardottir 2005). A majority of the parents felt the website was accessible, understandable, and helpful, but more importantly, 75% of the parents felt that other families could benefit from such an intervention (Svavarsdottir & Sigurdardottir 2005). Both the mother and father’s general wellbeing were significantly higher after the intervention as well (Svavarsdottir & Sigurdardottir 2005). From the administrative perspective all of the clinical nurses in the study reported positive responses concerning the intervention and the feasibility of the program (Svavarsdottir & Sigurdardottir 2005). Having positive responses from both the administrative and receptive sides of the intervention program supports the feasibility of such programs and the welcome and need for them. Psychosocial Considerations in Treatment All therapeutic options should consider psychosocial factors when treating a child with cancer. Awareness of these factors is necessary to fully understand the child and family’s needs, since stressors not only come from having cancer and treating it, but by what is also affected by having cancer. As could be predicted, better overall psychosocial adjustment has been associated with a better prognosis, including early knowledge of the diagnosis, a shorter treatment schedule, and a lack of relapses (Clarke et al., 2005; Eiser & Havermans, 1992). Cancer: Psychological Factors 33 Examples of psychosocial factors include lengthy treatments and hospitalizations that could disrupt schooling and socialization with peers. Also, treatments may involve traveling long distances that may require the family to either uproot and move temporarily or separate between two cities. Lengthy treatments as well as traveling and relocation costs could then cause a financial burden to an already distressed family. Therefore, finances should be addressed in the treatment process. Overall support from family, friends, and coworkers seems to be crucial as well. In particular, this may include a family’s religion, which can be an important factor in treatment and coping among children with cancer and their families. Besides the physical health of the child that may have been affected by chemotherapy, radiation treatments, surgery, amputation, or basic inpatient and outpatient care, all other factors that these could affect should be considered (Shapiro & Brack, 1994). Disruption in schooling is an important issue to address not only for the child with cancer, but for the siblings as well. Shapiro and Brack (1994) found that most well siblings reported few changes in their school functioning; however, parents often reported the opposite. There was also a difference between well sibling and parental reports of knowledge concerning what peers at school knew of what was happening. While parents believed children at school knew what was happening, well siblings indicated otherwise (Shapiro & Brack, 1994). Shapiro and Brack (1994) noted that well siblings also reported worries about their friends’ reactions to their sibling’s cancer. School personnel, such as the teacher and counselor, could help in these situations by discussing cancer and why either the well sibling or ill child may act differently during class; they could also emphasize the importance of support and normalcy (Shapiro & Brack, 1994). This may relieve the burden of a child telling their friends what is happening in their life as well as foster better understanding of cancer and the changes involved with treating Cancer: Psychological Factors 34 it. For instance, increased absences from the well sibling as well as lengthy absences from the child with cancer may both be explained to the class. This may include a discussion concerning when the ill child will be able to return to school, and that it may only be for a shortened time due to fatigue or other matters relating to illness (McGrath et al., 2005) School support seems to be crucial. In general, the better the communication that existed between the parent and well sibling, the better the prediction of the child in social and school interactions (Eiser & Havermans, 1992). However, Shapiro and Brack (1994) noted that many well siblings indicated they had no one they felt they could talk to, so school counselors could aid significantly in this situation. By making an effort to talk to the child, this may encourage a more open conversation than what may occur between a parent and child, since the child may feel they have to censor themselves in front of the parent (Eiser & Havermans, 1992; Houtzager et al., 2001; Kazak & Nachman, 1991; Shapiro & Brack, 1994). School counselors and teachers may therefore be a better judge of adjustment than parents or self-report measures (Shapiro & Brack, 1994). Teachers could also give the well sibling a special assignment, such as a presentation on cancer to the class, which could foster understanding from the class as a whole as well as give extra attention toward the well sibling (Shapiro & Brack, 1994). Feelings of importance and comfort in talking about cancer may develop from such a special assignment. Reintegration into school may prove to be an additional problem as school could be disrupted for both the ill child and well siblings (Katz, Varni, Rubenstein, Blew, & Hubert, 1992; McGrath, 2005). Katz et al. (1992) implemented a school reintegration program for children with cancer with reports of overall perceived benefits from teachers, parents, and the child. Teachers in particular noted the knowledge gained by school personnel concerning cancer, peers’ understanding of cancer, and social acceptance of peers as specific benefits to this program (Katz Cancer: Psychological Factors 35 et al.). The program consisted of counseling, educational presentations, a liaison between the school and hospital, and follow-ups. The researchers emphasized the importance of school reintegration as soon as medically possible in order to curb social and academic deficiencies that may occur due to childhood cancer. The researchers also suggested that education of cancer be implemented in regular school health education curriculums in order to promote overall understanding and positive attitudes toward individuals with cancer (Katz et al., 1992). Health education curriculums could correct preconceived notions about cancer as well, including what children hear from television, the radio, and unreliable sources (Eiser & Havermans, 1992). Eiser and Havermans (1992) stated that many children equate cancer with smoking, believing lung cancer to be the only type of cancer. A school curriculum that addressed cancer could also significantly aid in how children should react if one of their classmates has cancer, which could possibly reduce inappropriate behaviors from peers who do not understand what they are going through (Eiser & Havermans, 1992). Children noted that a great source of stress was from being teased or criticized when they were at school, which was generally directed toward being bald, thin, or that the child with cancer was “contagious,” resulting in exclusion from play and other activities (Eiser & Havermans, 1992). Programs or curriculums educating children about cancer could promote greater understanding and empathy as well as eradicate some of the unpleasantries, such as teasing. Specific programs for children with cancer could also be implemented for school integration to address how to handle teasing and talk comfortably about cancer to their peers. While school absence is a common issue for children with cancer and their siblings, parents may experience lengthy absences from work. Oftentimes one parent, typically the mother, has to stop working in order to fully care for the ill child (McGrath et al., 2005; Shapiro Cancer: Psychological Factors 36 & Brack, 1994). The father may have employment strains as well, including taking time off or reducing the number of hours working in order to be with the child (McGrath et al.). Changes in employment may then affect changes in income as a dual-based income reduces to a single income. While changes in employment may be necessary in order to care for the child, this inevitably affects the finances of not only expensive medical treatments, but relocation fees and extra transportation as well (McGrath et al.). Future employment is also a risk factor among children with cancer. Potential employers may have prejudices that cancer survivors will have poor attendance and need to take time off often (Eiser, 1998). Discrimination has even been noted in the armed forces (Eiser, 1998). Employment issues typically stem from ignorance and discrimination concerning cancer survivors; potential employers may assume they will become ill again and need to take time off, will not work as hard as other individuals, or have insurance problems that employers will not want to comply with (Eiser, 1998). However, general knowledge and the prevalence of long-term effects concerning employment remain predominately unknown. While the entire family readjusts to the various stressors related with childhood cancer, their coping mechanisms and support network becomes crucial. Religion is therefore a psychosocial factor that becomes especially important for many parents when their child has been diagnosed with cancer and has to endure lengthy treatments. The majority of Americans claim they are actively affiliated with a religious denomination, which means that a lot of families facing childhood cancer may use religion as a coping mechanism or foundation for hope (Schneider & Mannell, 2006). Spirituality, or the sense of meaning and purpose in one’s life without a specific religious affiliation, can also serve as a coping strategy (Schneider & Mannell, 2006). For this paper, the terms religion and spirituality will be used interchangeably and may Cancer: Psychological Factors 37 refer to both secular and non-secular associations; these terms are often used interchangeably since many people have their own definitions for each. When facing childhood cancer, parents often confront role changes in which spirituality is sometimes used to instill meaning and provide a sense of purpose (Schneider & Mannell, 2006). Schneider and Mannell (2006) suggested that using spirituality provided comfort, support, and a sense of control over a highly distressing situation. Surprisingly, the parental quality of life seems to benefit most when only one parent utilized religion as a coping mechanism in comparison to both parents (Goldbeck, 2001). Also, many viewed religion as a sense of strength rather than the ultimate power over their child’s cancer; many in fact used it in a positive light, rather than using religion when the child’s health was deteriorating (Schneider & Mannell, 2006). Prayer assisted as a further coping tool, of which both personal prayers and prayers from others were indicated as helpful (Schneider & Mannell, 2006). Prayer also aided in the sense of control, since it was something concrete that the parents could do (Schneider & Mannell, 2006). Some did however question the use of prayer and its ability to heal; despite this, parents still utilized prayer based on the belief that it could not make anything worse (Schneider & Mannell, 2006). However, others noted their concern, believing the exact opposite could occur as a result of prayer. Faltering faith is of course another issue concerning parents of children with cancer. Parents indicated that their spirituality tended to fluctuate depending on how well or not well their child was doing, at times questioning the power of religion (Schneider & Mannell, 2006). Most however indicated that despite fluctuations in their faith, they typically returned to their beliefs (Schneider & Mannell, 2006). This may however be dependent on the prognosis of the Cancer: Psychological Factors 38 child or at what stage the child is in. Others may lose their spirituality due to the difficulty in trying to understand why a child would have to suffer through cancer (Schneider & Mannell, 2006). In conclusion, completely losing one’s spirituality seems rarer than fluctuations occurring in one’s faith during the treatment stage of the child. Those who are religious may have to face practical limitations as well, such as not being able to attend church or spiritual gatherings due to the time spent with their ill child. Medical personnel can therefore provide information pertaining to religious services offered by the hospital or aid in bringing a spiritual advisor to the hospital for the family (Schneider & Mannell, 2006). If religion is perceived as helping in support, strength, and purpose for the entire family, then health professionals should be aware of this and aid in facilitating this strength during the treatment of the child. Support services and the availability of psychosocial programs to address these many psychosocial factors involved in the treatment of childhood cancer, as well as others not mentioned here, is however another topic. A national survey was conducted to determine the prevalence of three types of psychosocial programs and who administered them. These included pain or anxiety management, anticipatory emesis control, and support groups for pediatric oncology patients. The majority of facilities in the U.S. offered social work services, typically within the first month of diagnosis; however, pain and anxiety management programs and anticipatory emesis programs were only accounted for in 23% of oncology centers (Kaufman, Harbeck, Olson, & Nitschke, 1992). This figure is slightly distressing since many oncology patients experience nausea due to chemotherapy, anxiety, and pain due to medical procedures. Costs of professionals and their training have a potentially large factor in the offering of various psychosocial intervention programs. While a psychologist, who has extensive training, can offer Cancer: Psychological Factors 39 all three of these services, hiring a social worker would be more cost-effective; however, their training can only offer support groups. Therefore, cost factors seem to play a role in reasons for offering or not offering particular psychosocial programs. Not offering psychosocial programs could be detrimental to the child as well as the whole family, since this would allow greater anxiety, distress, and physical symptoms to occur, when they could be controlled and aided by psychosocial intervention programs. Identifying Positive Aspects in Cancer While childhood cancer has notably many negative consequences, positive aspects can be identified as well. Many children with cancer and their family members have been found to show growth in various areas of their lives as a result of living with cancer. The majority of participants in a study indicated that cancer in the long run had a positive impact on their lives and had increased their self-confidence (Gray et al., 1992). Survivors have indicated a more open outlook on life as well (Eiser, 1998). Some parents reported an overall increase in maturity in their child after receiving a diagnosis of cancer (Clarke et al., 2005), which may be attributed to an increase in contact with adults, such as hospital personnel. An increase in coping mechanisms has also been noted in children and adolescents with cancer. Hampel and colleagues (2005) suggested that exposure to a major stressor such as a life-threatening or chronic illness may make children less vulnerable to other minor stressors, thus improving their coping skills. Cancer has even motivated some survivors to pursue work involved with helping or teaching (Eiser, 1998). Other perceived benefits have been noted from siblings of children with cancer, including increased empathy (Shapiro & Brack, 1994). Some siblings of children with cancer have also shown more helping behaviors, the giving of gifts, sharing, and showing affection (Eiser & Havermans, 1992). Siblings have even noted their own increases in maturity, a change in values Cancer: Psychological Factors 40 concerning their life, and an increase in caring toward those with a handicap (Havermans & Eiser, 1994). The family as a whole noted that doing more things together as a family was a positive aspect of the experience (Shapiro & Brack, 1994). This may however only be experienced by those families who utilized support services or family retreats for children with cancer or lifethreatening illnesses. The support from charitable organizations and gifts from friends was also a benefit to the family (Shapiro & Brack, 1994). Families even expressed a less materialistic approach toward life (Eiser, 1998). Overall, a new appreciation for life seems to be a common feeling among families affected by childhood cancer (Eiser, 1998). Conclusions Cancer poses unique issues for children pertaining to their physical, mental, and social development. Physical effects may include both short and long-term consequences of treatment, all of which could contribute to the child’s mental health. The difficulty of facing the challenges of cancer may at times be overwhelming not only for the child, but for the child’s parents, siblings, and friends, possibly resulting in maladaptive coping responses or a lack of understanding. A full understanding in how the physical, mental, and social aspects of cancer influence each other is necessary for optimal treatment. The use of education and maintaining open and truthful relationships in a developmentally appropriate way seems to be the most beneficial to all who are directly or indirectly affected by cancer. Perhaps this greater understanding allows people to retrospectively find some positive aspect in the childhood cancer experience. Cancer: Psychological Factors 41 References Armstrong, F. D., Blumberg, M. J., & Toledano, S. R. (1999). Neurobehavioral issues in childhood cancer. School Psychology Review, 28, 194-203. Blotcky, A. D., Cohen, D. G., Conatser, C., & Klopovich, P. (1985). Psychosocial characteristics of adolescents who refuse cancer treatment. Journal of Consulting and Clinical Psychology, 53, 729-731. Butler, R. W., Rizzi, L. P., & Bandilla, E. B. (1999). The effects of childhood cancer and its treatment on two objective measures of psychological functioning. Children’s Health Care, 28, 311-327. Challinor, J., Miaskowski, C., Moore, I., Slaughter, R., & Franck, L. (2000). Review of research studies that evaluated the impact of treatment for childhood cancers on neurocognition and behavioral and social competence: Nursing implications. Journal of the Society of Pediatric Nurses, 5, 57-74. Clarke, S., Davies, H., Jenney, M., Glasler, A., & Eiser, C. (2005). Parental communication and children’s behaviour following diagnosis of childhood leukaemia. Psycho-Oncology, 14, 274-281. Cure Search. (2005). Incidence. Retrieved October 31, 2007, from http://www.curesearch.org/ our_research/index_sub.aspx?id=1475 De Graves, S. & Aranda, S. (2005). When a child cannot be cured—reflections of health professionals. European Journal of Cancer Care, 14, 132-140. Eiser, C. (1998). Practitioner review: Long-term consequences of childhood cancer. Journal of Child Psychology and Psychiatry, 39, 621-633. Cancer: Psychological Factors 42 Eiser, C. & Eiser J. R. (2000). Social comparisons and quality of life among survivors of childhood cancer and their mothers. Psychology and Health, 15, 435-450. Eiser, C. & Havermans, T. (1992). Children’s understanding of cancer. Psycho-Oncology, 1, 169-181. Freyer, D. R. (2004). Care of the dying adolescent: Special considerations. Pediatrics, 113, 381388. Goldbeck, L. (2001). Parental coping with the diagnosis of childhood cancer: Gender effects, dissimilarity within couples, and quality of life. Psycho-Oncology, 10, 325-335. Gray, R. E., Doan, B. D., Shermer, P., Vatter Fitzgerald, A., Berry, M. P., Jenkin, D., & Doherty, M. A. (1992). Surviving childhood cancer: A descriptive approach to understanding the impact of life-threatening illness. Psycho-Oncology, 1, 235-245. Greene, P. E. & Fergusson, J. H. (1982). Late effects of therapy. The American Journal of Nursing, 82, 443-446. Grootenhuis, M. A. & Last, B. F. (2001). Children with cancer with different survival perspectives: Defensiveness, control strategies, and psychological adjustment. PsychoOncology, 10, 305-314. Hampel, P., Rudolph, H., Stachow, R., Laß-Lentzsch, A., & Petermann, F. (2005). Coping among children and adolescents with chronic illness. Anxiety, Stress, and Coping, 18, 145-155. Havermans, T. & Eiser, C. (1994). Siblings of a child with cancer. Child: Care, Health, and Development, 20, 309-322. Haylock, P. J. (1987). Radiation therapy. The American Journal of Nursing, 87, 1441-1446. Cancer: Psychological Factors 43 Horwitz, W. A. & Kazak, A. E. (1990). Family adaptation to childhood cancer: sibling and family systems variables. Journal of Clinical Child Psychology, 19, 221-228. Houtzager, B. A., Grootenhuis, M. A., Hoekstra-Weebers, J. E. & Last, B. F. (2005). One month after diagnosis: quality of life, coping and previous functioning in siblings of children with cancer. Child: Care, Health, & Development, 31, 75-87. Houtzager, B. A., Grootenhuis, M. A., & Last, B. F. (2001). Supportive groups for siblings of pediatric oncology patients: Impact on anxiety. Psycho-Oncology, 10, 315-324. Jelalian, E., Stark, L. J., & Miller, D. (1997). Maternal attitudes toward discipline: A comparison of children with cancer and non-chronically ill peers. Children’s Health Care, 26, 169182. Jones, B. L. (2006). Companionship, control, and compassion: a social work perspective on the needs of children with cancer and their families at the end of life. Journal of Palliative Medicine, 9, 774-788. Katz, E. R., Varni, J. W., Rubenstein, C. L., Blew, A., & Hubert, N. (1992). Teacher, parent, and child evaluative ratings of a school reintegration intervention for children with newly diagnosed cancer. Children’s Health Care, 21, 69-75. Kaufman, K. L., Harbeck, C., Olson, R., & Nitschke, R. (1992). The availability of psychosocial interventions to children with cancer and their families. Children’s Health Care, 21, 2125. Kazak, A. E. & Nachman, G. S. (1991). Family research on childhood chronic illness: Pediatric oncology as an example. Journal of Family Psychology, 4, 462-483. Cancer: Psychological Factors 44 McGrath, P., Paton, M. A., & Huff, N. (2005). Beginning treatment for pediatric acute myeloid leukemia: The family connection. Issues in Comprehensive Pediatric Nursing, 28, 97114. Murray, J. S. (2001). Self-concept of siblings of children with cancer. Issues in Comprehensive Pediatric Nursing, 24, 85-94. Myers, C. E., McGuire, W. P., Liss, R. H., Ifrim, I., Grotzinger, K., & Young, R. C. (1977). Adriamycin: The role of lipid peroxidation in cardiac toxicity and tumor response. Science, 197, 165-167. Norberg, A. L., Lindblad, F., & Boman, K. K. (2006). Support-seeking, perceived support, and anxiety in mothers and fathers after children’s cancer treatment. Psycho-Oncology, 17, 335-343. Ogilvy-Stuart, A. L. & Shalet, S. M. (1993). Effect of radiation on the human reproductive system. Environmental Health Perspectives, 101, 109-116. Olson, R. D., Mushlin, P. S., Brenner, D. E., Fleischer, S., Cusack, B. J., Chang, B. K., & Boucek, R. J. (1988). Doxorubicin cardiotoxicity may be caused by its metabolite, doxorubicinol. Proceedings of the National Academy of Sciences of the United States of America, 85, 3585-3589. Orbuch, T. L., Parry, C., Chesler, M., Fritz, J., & Repetto, P. (2005). Parent-child relationships and quality of life: Resilience among childhood cancer survivors. Family Relations, 54, 171-183. Peckham, V. C., Meadows, A. T., Bartel, N., & Marrero, O. (1988). Educational late effects in long-term survivors of childhood acute lymphocytic leukemia. Pediatrics, 81, 127-133. Cancer: Psychological Factors 45 Schneider, M. A. & Mannell, R. C. (2006). Beacon in the storm: An exploration of the spirituality and faith of parents whose children have cancer. Issues in Comprehensive Pediatric Nursing, 29, 3-24. Shapiro, M. & Brack, G. (1994). Psychosocial aspects of siblings’ experiences of pediatric cancer. Psycho-Oncology, 28, 264-273. Sorgen, K. E. & Manne, S. L. (2002). Coping in children with cancer: Examining the goodnessof-fit hypothesis. Children’s Health Care, 31, 191-207. Stam, H., Grootenhuis, M. A., & Last, B. F. (2005). The course of life of survivors of childhood cancer. Psycho-Oncology, 14, 227-238. Svavarsdottir, E. K. & Sigurdardottir A. (2005). The feasibility of offering a family level intervention to parents of children with cancer. Scand J Caring Sci, 19, 368-372. Vance, Y. H. & Eiser, C. (2001). The school experience of the child with cancer. Child: Care, Health & Development, 28, 5-19. Wellisch, D. K., Crater, B., Wiley, F. M., Belin, T. R., & Weinstein, K. (2006). Psychological impacts of a camping experience for children with cancer and their siblings. PsychoOncology, 15, 56-65. Zebrack, B. J., Casillas, J., Nohr, L., Adams, H., & Zeltzer, L. K. (2004). Fertility issues for young adult survivors of childhood cancer. Psycho-Oncology, 13, 689-699.