Water and Major Minerals
advertisement

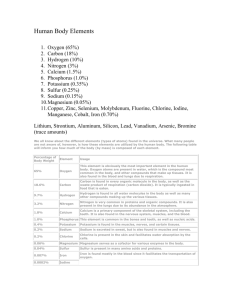
Water and Major Minerals I. Water and the Body Fluids The main role of water is to maintain an appropriate water balance to support vital functions. To maintain water homeostasis, intake from liquids, foods, and metabolism must equal losses from the kidneys, skin, lungs, and feces. A. Water’s roles in the body 1. Carries nutrients and waste products 2. Maintains the structure of large molecules 3. Participates in metabolic reactions 4. Solvent for minerals, vitamins, amino acids, glucose and others 5. Lubricant and cushion around joints, inside the eyes, the spinal cord, and in amniotic fluid during pregnancy 6. Regulation of body temperature 7. Maintains blood volume B. Water Balance and Recommended Intakes 1. Intracellular fluid (inside the cells) makes up about two-thirds of the body’s water. 2. Extracellular fluid (outside the cells) has two components—the interstitial fluid and plasma. 3. Water Intake a. Thirst is a conscious desire to drink and is regulated by the mouth, hypothalamus, and nerves. b. Dehydration occurs when water output exceeds input due to an inadequate intake or excessive losses. 1. 1-2% loss of body weight – thirst, fatigue, weakness, vague discomfort, and loss of appetite 2. 3-4% loss of body weight – impaired physical performance, dry mouth, reduction in urine, flushed skin, impatience, and apathy 3. 5-6% loss of body weight – difficulty in concentrating, headache, irritability, sleepiness, impaired temperature regulation, and increased respiratory rate 4. 7-10% loss of body weight – dizziness, spastic muscles, loss of balance, delirium, exhaustion, and collapse c. Water intoxication is excessive water contents in all body fluid compartments. It is rare. 4. Water sources include water, other beverages, fruit, vegetables, meat, cheese, and the byproduct of metabolism. An intake of 1450 to 2800 milliliters of water is usually represented by: a. Liquids – 550 to 1500 mL b. Foods – 700 to 1000 mL c. Metabolic water – 200 to 300 mL 5. Water losses occur through urine output, water vapor from the lungs, sweating, and feces. An output of 1450 to 2800 milliliters of water is usually represented by: a. Kidneys – 500 to 1400 mL 198 b. Skin – 450 to 900 mL c. Lungs – 350 mL d. GI tract – 150 mL 6. Water Recommendations a. 1.0 to 1.5 mL/kcal expended for adults (approximately 2-3 liters for a 2,000 kcalorie expenditure b. 1.5 mL/kcal expended for infants and athletes c. ½ cup per 100 kcal expended d. Adequate Intake for males is 3.7 L/day. e. Adequate Intake for females is 2.7 L/day. f. Both caffeine and alcohol can have a diuretic effect. 7. Health Effects of Water a. Meeting fluid needs b. Protect the bladder, prostrate, and breast against cancer c. Protect against kidney stones 8. Kinds of water IM CI 12.2 a. Hard Water 1. Water with high calcium and magnesium content 2. Leaves residues 3. May benefit hypertension and heart disease b. Soft water 1. Water with high sodium and potassium content 2. May aggravate hypertension and heart disease 3. Dissolves contaminate minerals in pipes 4. Practical advantages c. Other types of water: 1. Artesian water – water drawn from a well that taps a confined aquifer in which the water in under pressure 2. Bottled water – drinking water sold in bottles 3. Carbonated water – water that contains carbon dioxide gas, either natural or added 4. Distilled water – free of dissolved minerals 5. Filtered water – water treated by filtration with lead, arsenic, and some microorganisms removed 6. Mineral water – water from a spring or well that contains about 250-500 parts per million of minerals 7. Natural water – water from a spring or well that is certified to be safe and sanitary 8. Public water – water from a city or county water system that has been treated and disinfected 9. Purified water – water that has been treated to remove dissolved solids 10. Spring water – water originating from an underground spring or well 11. Well water – water drawn from ground water by tapping into an aquifer 199 C. Fluid and Electrolyte Balance – Several minerals including sodium, chloride, potassium, calcium, phosphorus, magnesium, and sulfur are involved in fluid balance. 1. Dissociation of Salt in Water a. Dissociates into positive ions called cations and negative ions called anions b. Ions carry electrical current so they are called electrolytes. c. Solutions are called electrolyte solutions. d. Positive and negative charges inside and outside the cell must be balanced. e. Milliequivalents is the concentration of electrolytes in a volume of solution. 2. Electrolytes Attract Water a. Water molecules are neutral, polar b. Oxygen is negatively charged. Hydrogen is positively charged. c. Enables body to move fluids 3. Water Follows Electrolytes a. Sodium and chloride are primarily outside the cell. b. Potassium, magnesium, phosphate and sulfur are primarily inside the cell. c. Osmosis is the movement of water across the cell membrane toward the more concentrated solutes. d. Osmotic pressure is the amount of pressure needed to prevent the movement of water across a cell membrane. 4. Proteins Regulate Flow of Fluids and Ions a. Proteins attract water and regulate fluid balance. b. Transport proteins regulate the passage of positive ions. c. Negative ions follow. d. Water flows toward the more concentrated solution. e. The sodium-potassium pump uses ATP to exchange minerals across the cell membrane. 5. Regulation of Fluid and Electrolyte Balance a. Digestive juices of GI tract contain minerals and these are reabsorbed as needed b. Kidneys maintain fluid balance using ADH c. Kidneys maintain electrolyte balance using aldosterone II. The Minerals—An Overview Major minerals are found in large quantities in the body, while trace minerals are found in small quantities. Minerals receive special handling in the body. They may bind with other substances and interact with other minerals, thus affecting absorption. A. Inorganic Elements 1. Major minerals or macrominerals retain their chemical identity when exposed to heat, air, acid, or mixing. 2. Minerals can be lost when they leach into water. B. The Body’s Handling of Minerals 1. Some behave like water-soluble vitamins. 2. Some behave like fat-soluble vitamins. 3. Excessive intake of minerals can be toxic. 200 C. Variable Bioavailability 1. Binders in food can combine chemically with minerals and prevent their absorption. 2. Phytates are found in legumes and grains. 3. Oxalates are found in spinach and rhubarb. D. Nutrient Interactions 1. Sodium and calcium 2. Phosphorus and magnesium 3. Often caused by supplements E. Varied Roles 1. Sodium, potassium and chloride function primarily in fluid balance. 2. Calcium, phosphorus and magnesium function primarily in bone growth and health. III. Sodium Sodium is one of the primary electrolytes in the body and is responsible for maintaining fluid balance. Dietary recommendations include a moderate intake of salt and sodium. Excesses may aggravate hypertension. Most of the sodium in the diet is found in table salt and processed foods. A. Sodium Roles in the Body 1. Maintains normal fluid and electrolyte and acid-base balance 2. Assists in nerve impulse transmission and muscle contraction 3. Filtered out of the blood by the kidneys B. Sodium Recommendations 1. Minimum Adults: 500 mg/day 2. Adequate Intake (2004) a. For those 19-50 years of age, 1,500 mg/day b. For those 51-70 years of age, 1,300 mg/day c. For those older than 70 years of age, 1,200 mg/day 3. The upper intake level for adults is 2,300 mg/day. 4. Maximum % Daily Value on food labels is set at 2400 mg/day. C. Sodium and Hypertension 1. Salt has a great impact on high blood pressure. Salt restriction does help to lower blood pressure. 2. Salt sensitivity is a term to describe individuals who respond to a high salt intake with high blood pressure. 3. Dietary Approaches to Stop Hypertension (DASH) is a diet plan that helps to lower blood pressure. D. Sodium and Bone Loss (Osteoporosis) 1. High sodium intake is associated with calcium excretion. E. Sodium in Foods 1. Large amounts in processed foods (approximately 75% of sodium in the diet) 2. Table salt (approximately 15% added sodium in the diet) 3. Sodium may be present in surprisingly high amounts if chloride is removed. 4. Moderate amounts in meats, milks, breads and vegetables (approximately 10% of sodium in the diet) 201 F. Sodium Deficiency 1. Sodium and water must be replaced after vomiting, diarrhea or heavy sweating. 2. Symptoms are muscle cramps, mental apathy, and loss of appetite. 3. Salt tablets without water induce dehydration. 4. Be careful of hyponatremia during ultra-endurance athletic activities. G. Sodium Toxicity and Excessive Intakes 1. Edema and acute hypertension 2. Prolonged high intake may contribute to hypertension. IV. Chloride Chloride in an essential nutrient that plays a role in fluid balance. It is associated with sodium and part of hydrochloric acid in the stomach. A. Chloride Roles in the Body 1. Maintains normal fluid and electrolyte balance 2. Part of hydrochloric acid found in the stomach 3. Necessary for proper digestion B. Chloride Recommendations and Intakes 1. Recommendations a. Adequate Intake (2004) 1. For those 19-50 years of age, 2,300 mg/day 2. For those 51-70 years of age, 2,000 mg/day 3. For those older than 70 years of age, 1,800 mg/day b. Upper intake level is 3,600 mg/day 2. Chloride Intakes a. Abundant in foods b. Abundant in processed foods C. Chloride Deficiency and Toxicity 1. Deficiency is rare. 2. Losses can occur with vomiting, diarrhea or heavy sweating. 3. Dehydration due to water deficiency can concentrate chloride to high levels. 4. The toxicity symptom is vomiting. V. Potassium Potassium is another electrolyte associated with fluid balance. It is associated with hypertension. It is found in fresh foods—mostly fruits and vegetables. A. Potassium Roles in the Body 1. Maintains normal fluid and electrolyte balance 2. Facilitates many reactions 3. Supports cell integrity 4. Assists in nerve impulse transmission and muscle contractions 5. Maintains the heartbeat B. Potassium Recommendations and Intakes 1. Adequate Intake (2004) 202 a. For all adults, 4,700 mg/day 2. Fresh foods are rich sources. 3. Processed foods have less potassium. C. Potassium and Hypertension 1. Low potassium intakes increase blood pressure. 2. High potassium intakes prevent and correct hypertension. D. Potassium Deficiency 1. Symptoms include muscular weakness, paralysis, confusion, increased blood pressure, salt sensitivity, kidney stones, and bone turnover. 2. Later signs include irregular heartbeats, muscle weakness, and glucose intolerance. E. Potassium Toxicity 1. Results from supplements or overconsumption of potassium salts 2. Can occur with certain diseases or treatments 3. Symptoms include muscular weakness and vomiting. 4. If given into a vein, potassium can cause the heart to stop. VI. Calcium Most of calcium (99%) is found in the bones. The remaining calcium (1%) is found in the blood and has many functions. Bone and blood calcium are kept in balance with a system of hormones and vitamin D. Blood calcium remains in balance at the expense of bone calcium and at the risk of developing osteoporosis in later years. A. Calcium Roles in the Body 1. Calcium in Bones (99% of calcium in the body) a. Hydroxyapatite are crystals of calcium and phosphorus. b. Mineralization is the process whereby minerals crystallize on the collagen matrix of a growing bone, hardening of the bone. c. There is an ongoing process of remodeling constantly taking place. 2. Calcium in Body Fluids a. Calmodulin is an inactive protein that becomes active when bound to calcium and serves as an interpreter for hormone and nerve-mediated messages. b. Ionized calcium has many functions. 3. Calcium and Disease Prevention a. May protect against hypertension b. DASH diet that is rich in calcium, magnesium, and potassium c. May be protective relationship with blood cholesterol, diabetes, and colon cancer 4. Calcium and Obesity a. Maintaining healthy body weight b. Calcium from dairy foods has better results than calcium from supplements. c. More research is needed. 5. Calcium Balance a. Works with vitamin D b. Works with parathyroid hormone and calcitonin c. Calcium rigor develops when there are high blood calcium levels and causes the muscles to contract. 203 d. Calcium tetany develops when there are low blood calcium levels and causes uncontrolled muscle contractions. e. Abnormalities are due to problems with hormone secretion or lack of vitamin D. f. Bones get robbed of calcium before blood concentrations get low. 6. Calcium Absorption a. Absorption rate for adults is 25% of calcium consumed. b. Calcium-binding protein is needed for calcium absorption. c. Factors that enhance absorption 1. Stomach acid 2. Vitamin D 3. Lactose 4. Growth hormones d. Factors that inhibit absorption 1. Lack of stomach acid 2. Vitamin D deficiency 3. High phosphorus intake 4. High-fiber diet 5. Phytates in seeds, nuts, and grains 6. Oxalates in beet greens, rhubarb, and spinach B. Calcium Recommendations and Sources 1. Calcium Recommendations (1997 Adequate Intake) a. AI Adolescents: 1300 mg/day b. AI Adults: 1000 mg/day if 19-50 years of age c. AI Adults: 1200 mg/day if greater than 50 years of age d. Upper level for adults: 2500 mg/day e. Peak bone mass is the bone’s fullest potential in size and density developed in the first three decades of life. 2. Calcium in Milk Products a. Drink milk. b. Eat yogurt and cheese. c. Add dry milk during food preparation. 3. Calcium in Other Foods a. Tofu, corn tortillas, some nuts and seeds b. Mustard and turnip greens, broccoli, bok choy, kale, parsley, watercress, and seaweed (nori) c. Legumes d. Oysters and small fish consumed with bones e. Mineral waters, calcium-fortified orange juice, fruit and vegetable juices, highcalcium milk f. Calcium-fortified cereals and breads D. Calcium Deficiency 1. Osteoporosis is the disease where the bones become porous and fragile due to mineral losses. 2. No obvious symptoms of mineral loss in bones appear. It is silent. 3. Deficiency in children can present as stunted growth. 204 4. Toxicity symptoms include constipation, increased risk of urinary stone formation, kidney dysfunction, and interference with the absorption of other minerals. VII. Phosphorus Most of the phosphorus is found in the bones and teeth. It is also important in energy metabolism, as part of phospholipids, and as part of genetic materials. A. Phosphorus Roles in the Body 1. Mineralization of bones and teeth 2. Part of every cell 3. Genetic material (DNA and RNA) 4. Part of phospholipids 5. Energy transfer 6. Buffer systems that maintain acid-base balance B. Phosphorus Recommendations and Intakes (1997 RDA) 1. RDA Adults: 700 mg/day for ages 19-70 years 2. Upper intake level for those 19-70 years of age is 4,000 mg/day. 3. Sources include all animal foods including meat, fish and poultry, milk and eggs C. Phosphorus toxicity symptoms include the calcification of nonskeletal tissues, especially the kidneys. VIII. Magnesium Magnesium supports bone mineralization, and is involved in energy systems and in heart functioning. It is widespread in foods. A. Magnesium Roles in the Body 1. Bone mineralization 2. Building of protein 3. Enzyme action 4. Normal muscle contraction 5. Nerve impulse transmission 6. Maintenance of teeth by preventing dental caries 7. Functioning of the immune system 8. Blood clotting B. Magnesium Intakes (1997 RDA) 1. RDA Adult Men: 400 mg/day for 19-30 years of age 2. RDA Adult Women: 310 mg/day for 19-30 years of age 3. Upper level for adults: 350 mg nonfood magnesium/day 4. Nuts and legumes, whole grains, dark green vegetables, seafood, chocolate and cocoa 5. Hard water and some mineral waters C. Magnesium Deficiency 1. Deficiencies are rare. 2. Symptoms a. Weakness and confusion b. Convulsions in extreme deficiency 205 c. Bizarre muscle movements of the eye and face d. Hallucinations e. Difficulties in swallowing f. Growth failure in children 3. Develops from alcohol abuse, protein malnutrition, kidney disorders and prolonged vomiting and diarrhea D. Magnesium and Hypertension 1. Protects against heart disease and hypertension 2. Low magnesium restricts walls of arteries and capillaries. E. Magnesium Toxicity 1. Symptoms from nonfood magnesium are diarrhea, alkalosis, and dehydration. IX. Sulfate Sulfate requirements are met by consuming a varied diet. It is found in essential nutrients including protein. There is no recommended intake and there are no known deficiencies. X. Highlight: Osteoporosis and Calcium Osteoporosis is one of the most prevalent diseases of aging. Strategies to reduce risks involve dietary calcium. A. Bone Development and Disintegration 1. Cortical bone is the outer shell compartment of bone. a. Creates the shell of long bones b. Creates the shell caps on the end of bones c. Releases calcium slower than trabecular bone d. Losses can begin in the 40s. 2. Trabecular bone is the inner lacy matrix compartment of bone. a. Can be affected by hormones in the body signaling the release of calcium b. Provides a source for blood calcium when needed c. Losses can become significant in the 30s for men and women. 1. Results in type I osteoporosis 2. Can result in spine and wrist fractures and loss of teeth 3. Women are affected 6 times as often as men. 3. Losses of both trabecular and cortical bone result in type II osteoporosis. a. Can result in compression fractures of the spine b. Hip fractures can develop. c. Twice as common in women as in men 4. The diagnosis of osteoporosis is performed using bone density tests. 5. Individual risk factors for osteoporosis are also considered. B. Age and Bone Calcium 1. Maximizing Bone Mass a. Children and adolescents need to consume enough calcium and vitamin D to create denser bones. 206 b. With a higher initial bone mass, the normal losses of bone density that occur with age will have less detrimental effects. 2. Minimizing Bone Loss a. Ensuring adequate intakes of vitamin D and calcium are consumed b. Hormonal changes can increase calcium losses. C. Gender and Hormones 1. Men at lower risk than women 2. Hormonal changes 3. Rapid bone loss in nonmenstruating women 4. Medications can be used that inhibit osteoclasts or stimulate osteoblasts. 5. Soy offers some protection. D. Genetics and Ethnicity 1. Genes may play a role. 2. Environment also – diet and calcium 3. Physical activity, body weight, alcohol, and smoking have a role. E. Physical Activity and Body Weight 1. Muscle strength and bone strength go together. 2. Heavy body weights and weight gains place a stress on bones and promote bone density. F. Smoking and Alcohol 1. Smokers a. Less dense bones b. Damage can be reversed when smoking stops. 2. Alcohol abuse a. Enhances fluid excretion, thus increases calcium losses b. Upsets hormonal balance for healthy bones c. Slows bone formation d. Stimulates bone breakdown e. Increases risks of falling G. Dietary Calcium – the key to prevention H. Other Nutrients 1. Adequate protein 2. Adequate vitamin D 3. Vitamin K protects against hip fractures. 4. Magnesium and potassium help to maintain bone mineral density. 5. Vitamin A 6. Omega-3 fatty acids 7. Fruits and vegetables 8. Reduce salt 207 I. A Perspective on Supplements 1. Calcium-rich foods are best. 2. Supplements may be needed when requirements are not met through foods. 3. Types of supplements a. Antacids contain calcium carbonate. b. Bone meal or powdered bone, oyster shell or dolomite are calcium supplements. c. Contain lead?? d. Small doses are better absorbed. e. Different absorption rates from different types of calcium supplements J. Some Closing Thoughts – Age, gender and genetics are beyond control. There are effective strategies for prevention that include adequate calcium and vitamin D intake, physical activity, moderation of alcohol, abstaining from cigarettes, and supplementation if needed. 1. List the roles of water in the body. 2. List the sources of water intake and routes of water excretion. 3. What is ADH? Where does it exert its action? What is aldosterone? How does it work? 4. How does the body use electrolytes to regulate fluid balance? 5. What do the terms major and trace mean when describing the minerals in the body? 6. Describe some characteristics of minerals that distinguish them from vitamins. 7. What is the major function of sodium in the body? Describe how the kidneys regulate blood sodium. Is a dietary deficiency of sodium likely? Why or why not? 8. List calcium’s roles in the body. How does the body keep blood calcium constant regardless of intake? Ca’s roles: bone structure, cell membrane integrity, transport of ions, muscle action, nerve impulses, regulates blood vessel wall muscle tone, helps regulate blood pressure, aids blood clotting, acts as cofactor for enzymes. When levels fall, intestinal absorption increases, bone withdrawal increases, and kidney excretion diminishes; these processes are regulated by a system of hormones and vitamin D. Excessive intakes of calcium can cause kidney stone formation. 9. Name significant food sources of calcium. What are the consequences of inadequate intakes? 10. List the roles of phosphorus in the body. Discuss the relationship between calcium and phosphorus. Is a dietary deficiency of phosphorus likely? Why or why not? 208 P’s roles: bone structure, part of DNA and RNA, activates enzymes, part of ATP, part of lipid structure and cell membranes. They combine as calcium phosphate in the crystals of bone and teeth, providing strength and rigidity. A deficiency is unlikely because phosphorus is abundant in animal tissues, eggs, and milk. 11. State the major functions of chloride, potassium, magnesium, and sulfur in the body. Are deficiencies of these nutrients likely to occur in your own diet? Why or why not? Chloride: maintains pH balance, allows nerve transmission and muscle contraction, catalyst in metabolism; potassium: maintains fluid and electrolyte balance and cell integrity; magnesium: bone structure, protein synthesis, energy metabolism, muscle relaxation; sulfur: protein structure. Deficiency of chloride is unusual but it can cause fluid and electrolyte problems; deficiency of potassium can cause increase in blood pressure, kidney stones and bone turnover. 209 Iron and Calcium in Your Diet The two minerals most likely to fall short in the diet are iron and calcium. Interestingly, both are found in protein-rich foods, but not in the same foods. Meats, fish, and poultry are rich in iron but poor in calcium. Conversely, milk and milk products are rich in calcium but poor in iron. Including meat or meat alternates for iron and milk and milk products for calcium can help defend against iron deficiency and osteoporosis, respectively. Determine whether these food choices are typical of your diet. Food choices Calcium-fortified foods (such as corn tortillas, tofu, cereals, or juices) Dark green vegetables (such as broccoli) Frequency per week Iron-fortified foods (such as breads or cereals) Legumes (such as pinto beans) Meats, fish, poultry, or eggs Milk or milk products Nuts (such as almonds) or seeds (such as sesame seeds) Small fish (such as sardines) or fish canned with bones (such as canned salmon) Whole- or enriched-grain products 1. Do you eat a variety of foods, including some meats, seafood, poultry, or legumes, daily? 2. Do you drink at least 3 glasses of milk—or get the equivalent in calcium—every day? 210