Equine Diseases
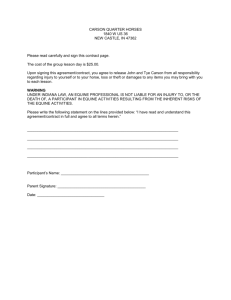
advertisement

Equine Diseases Equine Infectious Anemia (EIA) A ______________ diseases that affects the equine’s _____________ system resulting in recurrent ________________, weight _____________ and __________________. Once an equine is infected, it remains infected for the rest of its life. Chronically infected equine may go for years without showing signs of _______________ only to have the sign recur when stress, environmental conditions or other disease affects the equine. ___________________ and ___________________ are the major natural transmitters of the virus from one equine to another Detection- A blood test called the “_________________ test” is used to detect the presence of EIA. Equine must have a negative Coggins test before they can compete or be placed in events in North Carolina Prevention involves __________________ from equine that are not infected and protection from biting, flying insects. Treatment o There is no effective treatment or vaccination for the disease o In some cases, equine with EIA are required to be __________. Equine Influenza There are two common features of this _______________ infection o Extremely rapid spread of _________________ o Frequent, dry cough Equine with influenza have an elevated temperature of _________________ degrees F which persist up to _______ days The death rate from influenza is very ___________ The virus is spread to other equine when the equine _______________ or ________________ and may be carried by __________________ on equipment that have been in contact with an infected equine. Prevention o Use two __________________ injections of influenza vaccine scheduled 2-4 weeks apart followed by a booster shot at 3-4 month intervals for horses at risk. o __________________ of infected equine and screening animals prior to transportation will reduce the spread of the disease. Treatment o One _______________ of stall rest is recommended for each day the equine has an elevated temperature due to influenza o Maintain a ______________ free environment during the illness and recovery by _______________ hay and providing clean bedding. Equine Rhinopneumonitis This is a _____________ disease caused by _____________ virus. The infection is accompanied by a ____________ colored _______________ discharge among foals. The virus associated with this disease also may cause _______________ in pregnant mares and occasional _____________. Equine may develop a temperature of ______________ degrees F which lasts for ______________________. Equine become infected when they ________________ the virus exhaled by sick or even apparently healthy equine that are infected. Prevention requires a combination of o Sensible management practice o Mares should be isolated and separated from other equine o Thorough cleaning and sanitation in the event of _______________ or _______________ fetus Vaccination o Vaccinate pregnant mares in the ______, _________, and ______________ month of pregnancy. o Young equine should receive two injections followed by a booster according to manufacturer’s recommendations Treatment is limited as there is not specific anti-viral therapy available. Strangles A highly _______________ _________________ infection most commonly found in __________ equine from one to five years of age. Early signs of strangles include ______________, _____________ and loss of _______________ due to difficulty with swallowing. As strangles progresses, the ______________ _____________ and _______________ region may become hot, swollen and painful with _________________ forming and rupturing onto the skin. _______________ from ruptured abscesses may ______________ water buckets and _________________ feeders for months. When strangles develop and abscesses from on internal organs, mortality may be as high as ____________%. Prevention and treatment are used in conjunction. o Treat ruptured abscesses with a mild _______________ solution to hasten healing o Administer _______________ _________________ ____ as an antibiotic treatment until clinical signs no longer exist for five days. o _____________ affected animals from all other equine Vaccinate with 2 or 3 injections one month apart and apply a __________ annually. Equine Viral Arteritis (EVA) EVA is a ___________ infection that causes ____________ illness with ____________ and ______________ discharges, ___________ (stocking up) of the hind limbs and other areas of the body and sometimes _____________. EVA may be passed by respiratory transmission when equine come in close contact. Equine invariable make uneventful clinical recoveries even without treatment Perhaps EVA is most pronounced as a breeding disease through the _______________ spread of the disease by acutely affected stallions. Viral persistence in the stallion can range from several ____________ to the entire _____________ of the equine Mares can be infected either at time of natural breeding or artificial breeding. Prevention o Immunize the breeding stallion population with ______vaccine. o Immunize all mares if they are inseminated with EVA positive semen. Treatment o There is no specific anti-viral treatment for equine with EVA o Infected stallions should receive forced rest if they show symptoms of the disease. Eastern, Western and Venzuelan Equine Encepalomyelitis (EEE, WEE, and VEE) EEE, WEE, and VEE are ____________ infections that result in the ________________ of the __________________. The viral infections are spread by ________________ contact. The virus my live in reservoir hosts such as ___________ and _________________ for long periods of time without harming the host. The virus is transmitted and spread by ________________ (____________) to equine and humans. The viral infection is ___________ transmitted between equine and humans. The disease has high mortality rates: o EEE is _________________% o WEE is _________________% o VEE is _________________% Complete recovery is ____________ with equine frequently continuing to exhibit clumsiness, depression and abnormal behavior. Signs of EEE, WEE, and VEE include _____________, propulsive walking, _____________, and a number of things that indicate the equine is ________________. Prevention focuses on mosquito control. o Use insecticides and repellants when possible and practical o Eliminate _______________ water o Screen stalls, use fans to move air, and limit the use of _____________________ lights in stall areas o Brings equine inside prior to dusk o ____________ with 3 injections at 3, 4, and 6 months of age and give a booster at the beginning of insect season Treatment o There is not specific treatment available Equine Colic Colic is the behavioral signs of __________________ pain in equine characterized by various activities including, but not limited to: ________________________________________________________ ________________________________________________________ ________________________________________________________ True colic is due to ____________ _______________ or disease which causes pain __________% of all colic cases are from two causes o __________________ causes where there is intestinal spasm caused by numerous things such as stress, anxiety, diet change, parasite damage, dewormers, etc. o Large intestinal impaction (__________________) caused most often by improper diet and exercise (Human management is often culprit) Prevention o Use a _____________ management program to avoid problems o Careful rotation of pasture helps reduce levels of parasites o Avoid overstocking pastures o Use “Ivermectin” as a deworming compound o ___________________________________________________ Treatment o Place the equine in a safe environment o Treat with _______________ for pain relief o Treat with _____________ ______________ as a laxative o ________________ feed until the equine has improved and then reintroduce feed gradually o Do not allow the equine to eat too much hay or roughage (lightly grazing the pasture is recommended) Founder Characterized by the hoof collapsing as a result of _____________ (inflammation of the supporting tissue between the hoof wall and pedal bone) Causes lameness in the horse and if left unchecked can cause permanent _________________ or even require ________________. The leading cause of founder is _____________________ disturbance from any number of factors such as ___________________________ ________________________________________________________ Other factors that cause founder are exhaustion, excessive concussion (road founder) contact with black walnut shavings, etc. Prevention o ________________________________ o Avoid ________________ the equine Treatment o Identify cause and direct treatment toward alleviating the problem o Increase blood flow to the _________________ through the use of drugs and IV fluids o Use _________________or ________________ to thin blood o Use anti-inflammatory non-steroidal drugs (______________) to reduce laminar swelling o Pack the frog and sole to increase support o Use specialized shoes to relieve ___________ to the hoof area. Tetanus (Lockjaw) Caused by a _______________ that allows uncontrolled muscle contraction and muscle spasms Affected horses most often have sustained a wound from __________________ prior to the onset of tetanus; however, tetanus bacteria also live in the equine’s _________________ tract Tetanus has become less common due to vaccination, but is still highly _________________ Equine usually die from __________________, cardiac arrest or starvation since their _________________ system does not function Prevention o Vaccination with two doses of toxoid _____________ given one month apart followed by a booster shot annually o Equine that are injured should receive the toxoid booster if there is no record of prior shots Treatment o Administer ________________________ o Aggressively clean the wound o Administer tetanus anitoxin o Use __________________ and muscle _______________ to relieve spasms and muscle pain o Provide IV fluids and nutritional support Potamac Horse Fever (PHF) PHF is a disease which in its extreme form results in _____________ ___________________________________________________________ The occurrence of PHF disease is consistently within __________ miles of a _____________________ PHF is caused by an ______________ that can survive within living cells and must be transmitted through blood cells by insects such as _____________ Equine with PHF are not considered _____________ to other equine Prevention o Vaccinate with two injections one month apart o Give a booster injection annually in May or June Treatment o A veterinarian should use _________________ (anti-microbial drug) for 4-5 days o IV fluids, frog pads, sole support, and anti-inflammatory drugs also help Borreliosis (_____________________) Lyme disease is a _______________ infection transmitted primarily by certain ticks Rare among equine and only a problem where Lyme disease is found among human populations ______________ is the most commonly reported sign of Lyme disease in equine Prevention o Careful grooming to remove ticks o Avoiding ____________-infested areas Treatment o Use antibiotics such as tetracycline and ________________ o Prolonged treatment of 10-30 days usual West Nile Virus (WNV) _____________ infection that can cause inflammation of the brain and often mimics ______________ in equine First introduced in western hemisphere in ____________________ Equine are more often affected by WNV than any other domesticated animal WNV is spread by ___________________ when they bite an infected bird and then bite a human or an equine Equine are not _______________ and do not pose a health risk to other animals or humans About ____________% of horses who show clinical signs either __________ or have to be euthanized Clinical sign of WNV may include ______________, aimless wandering, head pressing, impaired vision, hyper excitability, etc. Prevention o See mosquito and control techniques listed for EEE, WEE and VEE o A veterinarian should vaccinate with “protocol” and follow with a booster injection three weeks later Treatment is still developing