Preface for National Planners: How to use this document
advertisement
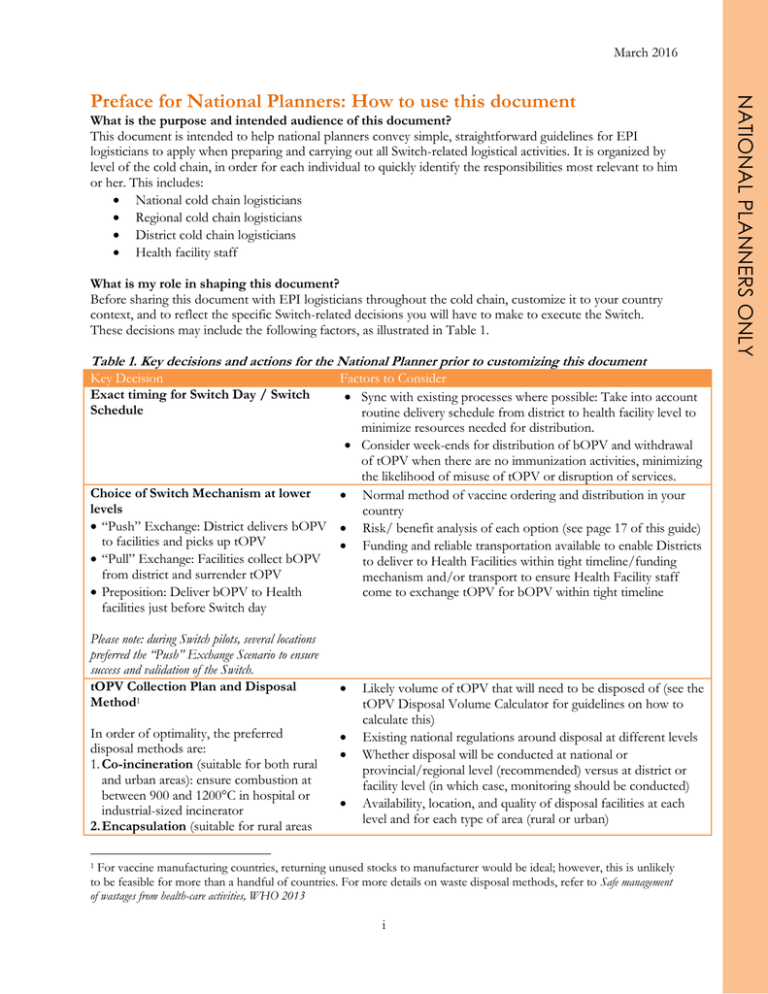
March 2016 What is the purpose and intended audience of this document? This document is intended to help national planners convey simple, straightforward guidelines for EPI logisticians to apply when preparing and carrying out all Switch-related logistical activities. It is organized by level of the cold chain, in order for each individual to quickly identify the responsibilities most relevant to him or her. This includes: National cold chain logisticians Regional cold chain logisticians District cold chain logisticians Health facility staff What is my role in shaping this document? Before sharing this document with EPI logisticians throughout the cold chain, customize it to your country context, and to reflect the specific Switch-related decisions you will have to make to execute the Switch. These decisions may include the following factors, as illustrated in Table 1. Table 1. Key decisions and actions for the National Planner prior to customizing this document Key Decision Exact timing for Switch Day / Switch Schedule Factors to Consider Sync with existing processes where possible: Take into account routine delivery schedule from district to health facility level to minimize resources needed for distribution. Consider week-ends for distribution of bOPV and withdrawal of tOPV when there are no immunization activities, minimizing the likelihood of misuse of tOPV or disruption of services. Choice of Switch Mechanism at lower Normal method of vaccine ordering and distribution in your levels country “Push” Exchange: District delivers bOPV Risk/ benefit analysis of each option (see page 17 of this guide) to facilities and picks up tOPV Funding and reliable transportation available to enable Districts “Pull” Exchange: Facilities collect bOPV to deliver to Health Facilities within tight timeline/funding from district and surrender tOPV mechanism and/or transport to ensure Health Facility staff Preposition: Deliver bOPV to Health come to exchange tOPV for bOPV within tight timeline facilities just before Switch day Please note: during Switch pilots, several locations preferred the “Push” Exchange Scenario to ensure success and validation of the Switch. tOPV Collection Plan and Disposal Method1 In order of optimality, the preferred disposal methods are: 1. Co-incineration (suitable for both rural and urban areas): ensure combustion at between 900 and 1200°C in hospital or industrial-sized incinerator 2. Encapsulation (suitable for rural areas Likely volume of tOPV that will need to be disposed of (see the tOPV Disposal Volume Calculator for guidelines on how to calculate this) Existing national regulations around disposal at different levels Whether disposal will be conducted at national or provincial/regional level (recommended) versus at district or facility level (in which case, monitoring should be conducted) Availability, location, and quality of disposal facilities at each level and for each type of area (rural or urban) For vaccine manufacturing countries, returning unused stocks to manufacturer would be ideal; however, this is unlikely to be feasible for more than a handful of countries. For more details on waste disposal methods, refer to Safe management of wastages from health-care activities, WHO 2013 1 i NATIONAL PLANNERS ONLY Preface for National Planners: How to use this document Suitability of disposal sites: o Availability of technically qualified staff o Accessibility of disposal site after Switch Day o Current readiness or ease of preparing the site o Good management and cleanliness of site Funding and staff availability for disposal monitoring mechanism (recommended though not required) For more guidance on how to develop a waste disposal plan for the Switch, see page 8 of this guide Funding available for unplanned, emergency dispatch of antigens Given that several of these decisions will have financial implications, national planners are recommended to: Advocate early for sufficient funds from national and partner sources to finance relevant Switch activities, based on a comprehensive, costed national Switch plan Design processes which are realistic in light of expected funding Ensure the secured funds efficiently flow down and are received on time at the level at which they are required (e.g. sufficient transportation funds are required at district level for a “push exchange”, and at health facility for a “pull exchange” scenario.) How should I best adapt this document for use in my country? You should adapt this document to retain only the information that is relevant to your country-specific situation and the Switch mechanisms you choose. In order to do this: Replace [text in orange brackets] throughout the guide with the appropriate information for your country. This includes, for instance, the exact date of the Switch. Identify which distribution/disposal scenario [in purple text] applies to your country o Retain the relevant paragraphs which apply to your country situation o Delete the scenarios that do not apply to your country situation Omit this preface (pages i and ii) and share only the adapted guidance with all EPI logisticians at the applicable level. ii NATIONAL PLANNERS ONLY only): Place the vials in hard containers, such as metal drums, and add an immobilizing material, such as cement, bituminous sand or clay. When dry, the drum or container can be sealed and buried in local landfill or a pit in a healthcare facility 3. Sanitary landfill (suitable for rural areas only): Dispose in fenced off sanitary landfill with no recycling activities nor public access Contingency Planning March 2016 Managing the Switch Supply and logistics guide for the switch Contents Introduction: A supply and logistics guide for the switch .......................................................... 2 1. 2. 3. 4. What is “the Switch”? ..................................................................................................................................................... 2 What are the logistics implications of the Switch?.............................................................................................. 2 What is the purpose of this document? ................................................................................................................... 2 Overview of the Switch ................................................................................................................................................... 3 Common Principles for All Levels ............................................................................................. 4 1. 2. 3. 4. 5. 6. tOPV inventories: conduct two inventories at all levels ................................................................................... 4 Calculating tOPV supply requirements until the Switch .................................................................................. 4 Communicating the Switch schedule and plan to lower levels ...................................................................... 5 Distributing bOPV to the next level down .............................................................................................................. 5 Contingency planning and tOPV buffer stock for emergency deliveries ................................................... 5 Disposal of excess tOPV after the Switch ................................................................................................................ 5 Central Vaccine Store ............................................................................................................ 11 1. Conduct inventories at Central Vaccine Store and coordinate inventories at lower levels ............. 11 2. Review and adjust procurement plans based on tOPV inventories ........................................................... 11 3. Communicate the Switch schedule and plan to lower levels ........................................................................ 12 4. Distribute last shipment of tOPV and first shipment of bOPV to lower levels, and organize incountry redistribution as required ................................................................................................................................... 12 5. Coordinate contingency plan and maintain buffer stock for emergency deliveries ........................... 12 6. Dispose of excess tOPV after the Switch................................................................................................................ 13 Regional Vaccine Store .......................................................................................................... 14 1. Conduct inventories at Regional Vaccine Store and coordinate inventory at District Level ........... 14 2. Distribute last shipment of tOPV and first shipment of bOPV to District level, and organize redistribution within region if required ......................................................................................................................... 14 3. Execute Contingency Plan ........................................................................................................................................... 15 4. Dispose of excess tOPV after the Switch................................................................................................................ 15 District Vaccine Store............................................................................................................. 16 1. 2. 3. 4. 5. 6. Conduct inventories at District Vaccine Store .................................................................................................... 16 Receive and properly store tOPV and bOPV in preparation for the Switch ........................................... 16 Establish contingency plan ......................................................................................................................................... 16 Distribute last shipment of tOPV, and organize redistribution within district if required .............. 17 Implement Switch: first shipment of bOPV to health facilities, collection of tOPV.............................. 17 Dispose of excess tOPV after the Switch................................................................................................................ 19 Health Facility Level ............................................................................................................... 20 1. 2. 3. Communicate any unplanned tOPV needs through contingency mechanism ....................................... 20 Execute the Switch ......................................................................................................................................................... 20 Dispose of excess tOPV after the Switch................................................................................................................ 21 Annex 1: Labelling of tOPV bags/containers for disposal ....................................................... 22 Annex 2: Sample tOPV collection form .................................................................................. 23 1 1. What is “the Switch”? Eradicating polio requires a globally coordinated effort to shift from the use of Oral Polio Vaccine (OPV) to Inactivated Polio Vaccine (IPV) through a phased approach. 1. All countries must introduce in 2015 at least one dose of IPV into routine immunization systems as a complement to the OPV schedule. 2. All countries switch from using trivalent OPV (tOPV) to bivalent OPV (bOPV) for routine immunization and campaign immunization activities. This will drastically reduce occurrences of Vaccine Associated Paralytic Poliomyelitis (VAPP) and Circulating Vaccine-Derived Poliovirus (cVDPV). 3. Finally, after global certification of polio eradication, there will be a need for the global cessation of OPV usage, leaving IPV as the sole polio vaccine used in routine immunization. This document centers on the second step of polio eradication: the replacement of tOPV with bOPV (“the Switch”), which will occur in April 2016 across the world. Shortly before this date, all manufacturers will stop producing or distributing tOPV. As of the date of the Switch, no child should be vaccinated with tOPV. The Switch must be a globally coordinated process; ongoing tOPV use after April 2016 would hinder polio eradication due to possible outbreaks of cVDPVs. An overview of the Switch activities is presented on the next page. 2. What are the logistics implications of the Switch? tOPV and bOPV require the same number of doses for full immunization, and have the same administration process and schedule. Thus, the impact of the Switch on vaccine service delivery will be limited. However, the Switch differs from a traditional vaccine replacement process, because tOPV usage must stop on the same day throughout the country, and all unused tOPV must be disposed of as soon as possible thereafter. Thus, the Switch presents unique challenges for supply chain and logistics systems both in country and globally, such as: Careful forecasting of tOPV stock to minimize wastage yet avoid stock outs prior to the Switch The short-term complexity in the cold chain logistics system as both bOPV and tOPV will be stored in the system for a period of time leading up to Switch Day The need for contingency distribution plans in case of stock outs or polio outbreak before the Switch Disposal of all tOPV as soon as possible after the Switch Day, but no later than three months after the Switch Day. Stock management practices for the Switch should, as much as possible, build on existing routine supply and cold chain processes in country. 3. What is the purpose of this document? This document provides guidelines for EPI logisticians to apply when preparing and carrying out all Switchrelated logistical activities. It is organized by level of the vaccine supply chain, in order for each individual to quickly identify the information most relevant to him/her, and can serve as a stand-alone, comprehensive, user friendly checklist for each level. 2 RELEVANT FOR ALL LEVELS Introduction: A supply and logistics guide for the switch 4. Overview of the Switch The table below summarizes the key activities of the Switch. Logistics-related activities for which guidance is provided in this document are bolded. By June 2015 Plan - Establish management structure - Establish National Switch Validation Committee (NSVC) - Conduct situation analysis - Draft national switch plan (budgeted and finalized by Sept 2015) May to September 2015 - Complete detailed tOPV inventory; adjust tOPV delivery (may vary per country) - Secure funding and finalize national switch plan - Develop monitoring plan October to November 2015 Prepare - Complete second tOPV inventory; adjust tOPV orders and/or delivery - Order bOPV - Develop waste management protocol - Hire switch support staff December 2015 to January 2016 - Receive last tOPV delivery to country; - Redistribute remaining tOPV stock within country as required - Prepare training materials and implement communications strategy - Begin bOPV deliveries to countries February to March 2016 - Deliver last 1-2 months of tOPV to periphery; redistribute as needed - Identify switch monitors Implement National Switch Day Validate Two to four weeks prior to the switch - Train switch monitors - Train health workers - Distribute bOPV to periphery and service points A day chosen during the period of 17 April to 1 May, 2016 - Stop use of tOPV and remove tOPV from cold chain - Begin use of bOPV In a two week period after the Switch Day - Validate tOPV disposal at selected sites (switch monitors) - Collect and review data and validate switch (NSVC) 3 RELEVANT FOR ALL LEVELS The guidelines here presented were developed at global level, in order to facilitate a coordinated Switch across countries, and have been adapted by national planners to fit the [country] context. The main principles underpinning this guidance are: Stock management practices for the Switch should, as much as possible, build on existing routine supply and cold chain processes in country There is a “right balance” which must be found between the two imperatives of the Switch: A table summarizing key logistics considerations relevant for all levels is found on page 9. 1. tOPV inventories: conduct two inventories at all levels To help minimize tOPV wastage, two national inventories of tOPV should be conducted in the year leading up to the tOPV/bOPV Switch. The inventory data will help to inform stock procurement and distribution in the lead-up to the switch. The first inventory To be completed as soon as possible, before end of September 2015 Data to be used to adjust quantity and timing of shipments of tOPV in the remaining months before the Switch day to avoid upfront risk of over-stocking. The second inventory To be conducted approximately 6 months before the Switch (~ October /November 2015), prior to the final tOPV shipment Data to more precisely inform the final order, enable in-country redistribution, and minimize overall wastage. While many countries already have stock management tools in place, due to the level of precision required for forecasting for the Switch, physical counts of tOPV will be necessary. The IPV OPV inventory tool 2 developed by UNICEF can be used to support this process. 2. Calculating tOPV supply requirements until the Switch To calculate quantities for the last shipments of tOPV to each level, follow the consumption-based formula: tOPV used over a given period =stock at beginning of period + received stock – current stock If consumption-based method is not possible, or for areas with reliable target populations: Amount of tOPV to distribute to the next level down = ((Annual target population × number of doses needed per child × Wastage factor) × (number of days of stock to be delivered/365)) - (tOPV stock remaining as reflected in the inventory) As the Switch day draws closer, supplies should be calculated based on immunization activities planned and previous consumption, and not just based on target beneficiaries. In preparation, it is important to strengthen mechanisms to review vaccine utilization (and not just distribution), needs assessment and stock management. This could entail for instance, a periodic review meeting of regional district and health facility level vaccine handlers. 2 Available at: http://www.who.int/immunization/diseases/poliomyelitis/endgame_objective2/oral_polio_vaccine/implementation/en/ 4 RELEVANT FOR ALL LEVELS Common Principles for All Levels Countries are encouraged to perform an analysis of their actual consumption compared with target consumption by region after the inventory, and adjust their average consumption and minimum/maximum levels for Regions, Districts and Health Facilities as required. 3. Communicating the Switch schedule and plan to lower levels Staff should use stock distributions taking place over the months leading up to the Switch as an opportunity to remind vaccine store staff at the lower levels of the upcoming timelines and responsibilities. Communication on the distribution plan, contingency plan and contacts (see #5) and the tOPV collection and disposal plan (see #6) should be included as well. 4. Distributing bOPV to the next level down bOPV should be distributed early enough to arrive at the district level at least two weeks before the Switch. Work backwards from this timeline while developing a distribution plan to ensure bOPV arrives in time for distribution at each level. Amount of bOPV to distribute to the next level down = (Annual target population × number of doses needed per person × Wastage factor) × (number of days of stock to be delivered/365) The consumption-based forecasting method described above can be used where appropriate. 5. Contingency planning and tOPV buffer stock for emergency deliveries Supply disruptions may arise from inaccurate forecasting or higher than expected demand or wastage. Contingency plans should be developed to ensure stock outs of tOPV don’t result in children missing out on vaccinations in the lead up to the Switch. One week buffer supply of tOPV should be kept at Central level, ready for distribution for any new/unscheduled delivery o EPI should decide whether any extra stock of tOPV should also sit at the Regional level or if the risk of localized stock outs can be minimized through reallocation of routine stock across health facilities. Focal points should be designated at national, regional, district levels to field emergency requests for additional supply of tOPV Ensure all levels are aware of the procedures and know who to contact in the event of higher than planned use, unusually large demand (e.g. polio outbreak leading to new campaign needs) or unexpectedly large wastage (e.g. temperature excursion). A contingency plan should also be in place in case distribution plans must be adjusted due to delays in delivery of bOPV at any level. This may require a parallel distribution, which may require additional logistics. 6. Disposal of excess tOPV after the Switch On Switch day, all remaining tOPV must be removed from the cold chain at all levels and, after the Switch, tOPV must be rapidly disposed of in order to reduce the risk of cVDPV.3 National planners should develop, communicate, and execute a tOPV collection and disposal plan for the country. The national team may choose to involve the regional and/or district level in the creation of the collection and disposal plan. “The rate of poliovirus inactivation is dependent on numerous conditions, but survival in the environment is finite. Interpolation of the available data indicates that poliovirus infectivity decreases by 90% in soil every 20 days in winter and every 1.5 days in summer, in sewage every 26 days at 23°C, in fresh water every 5.5 days at ambient temperatures, and in seawater every 2.5 days under the same conditions. ” The Biologic Principles of Poliovirus Eradication, Walter R~ Dowdle and Maureen E. Birmingham, JID 1997;175(suppl1):S286-92 3 5 STORE STAFF FOR ALL LEVELS CENTRAL RELEVANTVACCINE tOPV MUST be inactivated 4 prior to disposal. The following are the recommended methods for the inactivation and subsequent disposal of tOPV: • Inactivation by: autoclaving, boiling, chemical inactivation, encapsulation or incineration • Disposal by: transporting to waste facility or burying The inactivation and disposal of tOPV can be summarized through the following four steps: Step 1: Evaluate volumes of tOPV vials to be destroyed Step 2: Determine materials of tOPV vials to be destroyed Step 3: Choose appropriate method to inactivate tOPV Step 4: Dispose of the inactivated tOPV vials Step 1: Evaluate volumes of tOPV vials to be destroyed Volume of tOPV to be disposed Small volume of tOPV defined as 20 vials or less, allow for local level disposal at facility level Large volume of tOPV defined as 20 vials or more, may require additional capacity for disposal of tOPV Step 2: Determine materials of tOPV vials to be destroyed Glass vials- may shatter and harm the operator or may melt and cause damage to the incinerators Plastic vials- incineration or burning of plastics is prohibited in some countries5 Sealed vials -may explode under pressure (incineration & autoclaving) and endanger the operator6,7 Open vials- will allow for safe inactivation of tOPV by any method. However, staff should handle open vials as hazardous infectious waste and take precautions (e.g. wearing personal protective equipment) Step 3: Choose appropriate method to inactivate tOPV tOPV inactivation can be achieved by, autoclaving, boiling, chemical inactivation, encapsulation or incineration of the tOPV waste. The table below describes how each method of inactivation works: Inactivation of tOPV is defined as eliminating the infectious nature of poliovirus in tOPV or otherwise rendering the tOPV vials unusable and inaccessible (encapsulation) 5 Stockholm Convention, Article 5 & Annex C, Part II, (a): http://www.pops.int/documents/convtext/convtext_en.pdf 4 6 7 Guidelines for Safe disposal of Unwanted Pharmaceuticals in and after Emergencies, WHO 1999 Safe management of wastages from health-care activities, WHO 2013 6 RELEVANT FOR ALL LEVELS Disposal of tOPV after the switch should follow national legislation. If national legislation does not provide clear guidance, this section of the guide discusses safe approaches for the disposal of tOPV. Methods for inactivation of tOPV Autoclaving This method uses high-temperature steam. It is the most environmentally friendly method. Glass vials full of liquid (i.e. not opened) should be “loosened” before autoclaving to avoid rupture, unless the autoclave has an integrated shredder. However, vials (plastic or glass) that contain little liquid do not need to be open. After autoclaving, vials will be sterile but must still be disposed of following national or local waste management guidelines for municipal waste. Boiling Boling involves immersing vials in boiling water for approximately 30 minutes, which destroys pathogenic microorganisms. Both glass and plastic vials can be safely boiled. Glass vials can be boiled without opening. After boiling, the inactivated vials should be disposed of following national or local waste management guidelines. Chemical inactivation Chemical inactivation of tOPV involves opening and immersing tOPV vials in 0.5% chlorine solution for at least 30 minutes. The solution should be 9 parts clear water to 1 part household bleach. Immersing 20 vials in 4 liters of solution will safely inactivate tOPV. After this treatment, vials and leftover chlorine solution must both be disposed of following national or local waste management guidelines. Incineration Incineration should be done, at 1100°C or more for safe destruction of glass vials with tOPV (e.g. rotary-kiln incinerators and industrial furnaces). It is important to note that incinerators vary in temperatures reached in primary waste chamber. For instance, low temperature burning (<800°C), which is not recommended because it is environmentally hazardous (e.g. single chamber cement or brick covered incinerators). Additionally, medium temperature burning (800-1100°C) using dual-chamber incinerators may cause glass vials to explode or partially melt, and it is not recommended. Plastic vial incineration may be prohibited in some countries due to toxic emissions but it is possible at medium and higher temperatures (>800°C) if permitted by national emissions guidelines. Also, co-incineration in industrial furnaces (e.g. cement kilns) will both inactivate and destroy tOPV vials and can be done in partnership with and industrial facility. The resulting ash and any other post-incineration residue must be treated as toxic waste and disposed of according to national or local waste management guidelines. Open pit burning of plastics can have a severe negative environmental impact and therefore should not be used as an inactivation method. Encapsulation This method disposes of tOPV without immediate inactivation (and without opening the vials) but makes it inaccessible and puts it beyond use. This method involves filling containers ¾ full with tOPV vials, adding an immobilizing material (e.g. sand, cement, or clay) and sealing and burying the containers. The encapsulated waste must be disposed of following National or local waste management guidelines for municipal waste. 7 Create a national tOPV collection and disposal plan. Estimate the quantity of tOPV that must be disposed of nationally and in each region, remembering that 1 week of tOPV supply for one million inhabitants is roughly 5-8 liters for disposal. o If tOPV deliveries are carefully monitored in the months prior to the Switch Day, most countries should have a minimum of a few days and a maximum of two weeks of remaining tOPV in stock at each service point, i.e. 10-16 liters per population of one million. o This remaining tOPV should be disposed within three months after Switch Day. Estimating tOPV disposal volume. For regions applying the multi-dose vial policy (MDVP): Total litres of tOPV for disposal = 0.005 x wks of tOPV supply to dispose x target population/1000 For regions not applying the MDVP: Total litres of tOPV for disposal = 0.0075 x wks of tOPV supply to dispose x target population/1000 Assumptions: Based on 3.5% newborns, 4 dose EPI calendar, 85% coverage, 30% wastage and 1.5 cc volume per dose including packaging, disposal volume is 0.005 L per 000' population for regions applying the MDVP, 0.0075 L per '000 for others not applying the MDVP. Communicate disposal plan to [relevant subnational] levels. Coordinate with lower subnational levels to check all potential disposal sites for readiness and adjust disposal plan if required Ensure that all selected disposal sites are informed about their task and implement necessary preparations Ensure all health facilities, including private, with tOPV receive a copy of the collection and disposal plan 8 RELEVANT FOR ALL LEVELS Step 4: Dispose of the inactivated tOPV vials After tOPV has been inactivated, the waste must be disposed using the following two recommended approaches: Transport the waste materials to a waste facility (e.g. sanitary land fill, municipal dump, industrial waste site, or other facility meeting national and local waste guidelines); or Bury the waste materials on-site in a secured and fenced-off burial site Summary of key logistics considerations relevant for all levels Topic Inventory OPV procurement Key Points Conduct 2 inventories, at ~12 and 6 months before the switch through a direct physical count of all available tOPV stock and report to the level above. Collect and analyze inventory data prior to placing orders National yes Applies to: Regional District yes yes yes Calculate tOPV requirements so that all tOPV be consumed by [Switch day] with the exception of a minimal amount of extra supply used as contingency stock to be able to respond to the risk of localized stockouts. Estimate of tOPV needs until the switch and bOPV after the switch for your region or for distribution to lower levels. Consider 2 methods: yes yes yes Distribute last shipment of tOPV and first shipment of bOPV to lower levels. Communication The consumption based method should be prioritized for distribution from district to health facility level yes yes yes Use vaccine distribution during the months prior to the switch as an opportunity to keep staff at lower levels informed about the tOPV/bOPV distribution plan. yes yes yes a) in case of doubt about the size of the target populations, follow the consumption-based formula: tOPV used over a given period =stock at the beginning of a period + received stock – current stock . b) for areas with reliable target populations use the following method: ((Annual target population of the region × number of doses needed per person × Wastage factor) × (number of days of stock to be delivered/365)) - (tOPV stock remaining as reflected in the second inventory for this region) Compare the outcome of this method with the real consumption and refer to the first method if the difference is too large. 9 HF (yes) Contingency plan Develop contingency plans with the following elements: a) keep buffer stocks of one week consumption at national and regional levels; b) ensure up to date information of tOPV stocks at lower levels: increase reporting from lower levels to once a week for the last month before the switch; c) ensure all levels are aware of the procedures, know where the buffer is and who to contact d) ensure the availability of means of transport e) ensure contingency funds available for unplanned emergency dispatch of vaccines Pull or Push The actual exchange of leftover tOPV with bOPV on or shortly before switch day can follow the pull method (the exchange takes place in the district store) or the push (exchange at HF level) method. Consider normal method of vaccine distribution in country – best is to stick to what people are used to. Handling tOPV after the switch 1. Remove any remaining tOPV from the cold chain equipment 2. Note in stock registries the amount removed 3. Place in designated bags or containers and write the quantities in doses and date removed from cold chain on the “tOPV for disposal” sticker 4. Transport it to the designated location to be collected/disposed of through the chosen method as per the tOPV collection and disposal plan. yes tOPV disposal tOPV MUST be inactivated prior to disposal. The following are the recommended methods for the inactivation and subsequent disposal of tOPV: • Inactivation by: autoclaving, boiling, chemical inactivation, encapsulation or incineration • Disposal by: transporting to waste facility or burying yes 10 yes yes yes yes yes yes yes yes yes (yes) Only in very specific cases like areas with limited access March 2016 Staff at the Central Vaccine Store are responsible for: 1. Conducting and coordinating at the minimum two tOPV inventories 2. Reviewing and adjusting procurement plans/delivery schedules from suppliers/UNICEF/other agency to avoid overstocking tOPV 3. Communicating the switch schedule and plans (distribution, collection and disposal) to lower levels 4. Distributing last shipment of tOPV and first shipment of bOPV to lower levels, and organizing in-country redistribution as required 5. Putting in place a contingency plan and maintaining a buffer stock for emergency deliveries 6. Collecting and disposing of excess tOPV after the Switch 1. Conduct inventories at Central Vaccine Store and coordinate inventories at lower levels Methodology. Conduct a direct physical count of all available tOPV stock in the Central Vaccines Store. Report data on doses and not on vials, including data on the following: Date of inventory Stocks in doses: o In systems o Physical count Expiration date Manufacturer Packaging (number of doses per vial) Physical location of the stock Supply balances from recent SIA activities (if any) Orders recently received or pending, which are not yet recorded in stock records Update data in the national stock management systems with the revised, accurate figures. Coordination of stock inventories at all levels of the supply chain. Include all types of facilities and vaccine storage points in the inventory exercise, both in the public and private sector, including pharmacies, warehouses or other locations providing or storing tOPV. o A separate coordinating mechanism may be needed for private-sector facilities to report to staff at the Central Vaccine Store. Communicate expectations to regional and/or district-level staff to make their responsibilities for the inventories clear. A national-level directive from the Ministry of Health (i.e., letter or official circular) may be necessary to direct the process and timeline for stock inventories. All levels should conduct their physical count within a one-week time frame to minimize the risk of double-counting stock designated for delivery down the supply chain District and regional-level staff should report (via phone call or SMS message) total tOPV levels up the supply chain, with the national-level staff receiving all data from regional-level stores. Aggregate all the data at the Central Vaccine Store level for analysis (see below). 2. Review and adjust procurement plans based on tOPV inventories Collect and analyze inventory data prior to placing orders for tOPV needed up until the Switch. Use the following formula to calculate the total quantity of tOPV on-hand: 11 CENTRAL VACCINE STORE STAFF Central Vaccine Store Calculate tOPV requirements so that all tOPV will be consumed by [Switch day] with the exception of a minimal amount of extra supply used as contingency stock for response in the event of localized stock outs. One week of contingency stock should be stored at the Central Vaccine Store level. (Additional contingency stock may also be held at the regional level. See #5 on contingency plan, below) 3. Communicate the Switch schedule and plan to lower levels Use in-country distribution as opportunities to remind the regional staff of the Switch timelines and their responsibilities for ensuring a complete switch on Switch day. 4. Distribute last shipment of tOPV and first shipment of bOPV to lower levels, and organize in-country redistribution as required Calculate quantity and distribute last shipments of tOPV. Use the consumption-based formula or target population method, as described above, to calculate the amount of tOPV you must distribute to each region for the final delivery. o If any contingency stock is also to be held at the regional level, include this amount in the allocation and delivery for each region If there are Polio Supplementary Immunization Activities planned, include the quantity required in the allocations delivered to each region It is important to note that the final delivery of tOPV may be a few months ahead of the Switch (e.g., if delivering on a quarterly schedule, the final delivery to the region should be the January 2016 delivery.) Where the first inventory showed an overstock of tOPV of more than three months, adjust delivery for the second to last-delivery as well, using the results from the first inventory. Distribute adequate quantity of bOPV to Regional Vaccine Stores. Central Vaccine Store staff must develop a distribution plan and share it with lower levels. The bOPV should be distributed early enough to arrive at the district level two weeks before the Switch. o i.e., If regional distribution is on a quarterly schedule, the bOPV should be distributed with the January 2016 wave in order to ensure onward distribution to the periphery in time. Ensure that distribution planning is factored into procurement timelines (and vice versa) for bOPV. For example, a January 2016 delivery must be anticipated well in advance in order to ensure orders are placed, funds are transferred, and licensing/registration requirements are met in time. Special delivery requirements (pre-inspection, additional documentation, etc.) should be minimized to the extent possible for the first delivery. Early discussions on these issues with customs authorities, NRA, and central medical stores is highly recommended. Quantities of bOPV for distribution to the regions should be calculated using routine forecasting methods. Ensure that tOPV is clearly labeled and stored separately from bOPV. In order to avoid any risk of being mixed with tOPV deliveries and administered to patients prior to the Switch, keep stocks of bOPV separate from tOPV while awaiting distribution. Store in different cold chain equipment where possible, or on different shelves or opposite sides of the fridge Use special tOPV stickers on tOPV secondary packaging, if available (see example in Annex 1) 5. Coordinate contingency plan and maintain buffer stock for emergency deliveries Store the equivalent of one week of national supply of tOPV at the Central Vaccine Store, ready for distribution for any new/unscheduled delivery 12 CENTRAL VACCINE STORE STAFF Total tOPV = Quantity in-stock – (expired tOPV stock) – (tOPV stock with VVM stage 3 or 4) Dedicate a focal point to field emergency requests for additional supply of tOPV who has the authority to allocate and distribute tOPV accordingly, either through: a. Increasing quantity of next scheduled delivery, or b. Dispatching an out-of-schedule delivery Communicate to regional and district vaccine stores who to contact and under what circumstances 6. Dispose of excess tOPV after the Switch Dispose of all tOPV in the Central Vaccine Store. On Switch Day: 1. Remove any remaining tOPV from the cold chain in the central store 2. Note the amount of tOPV removed in stock registries 3. Place in designated bags or containers marked with the “tOPV for disposal” and write quantity in doses and date of removal from the cold chain on the sticker (see Annex 1) 4. Transport it to the designated disposal site according to the national plan for tOPV collection and disposal Coordinate tOPV collection and disposal at lower levels if applicable as per the national tOPV collection and disposal plan. 13 CENTRAL VACCINE STORE STAFF Regional-level staff are responsible for: 1. Conducting and coordinating at the minimum two tOPV inventories, communicating the inventory process to staff at lower levels of the supply chain, collating and reporting up the inventory data received from district vaccine stores 2. Distributing adequate amounts of tOPV and bOPV to District levels on time for the Switch; and organizing redistribution across districts as required 3. Communicating the switch schedule and plans (distribution, collection and disposal) to lower levels 4. Understanding and putting in place the supply contingency plan communicated from Central Vaccine Store 5. Collecting and disposing of excess tOPV according to guidelines. 1. Conduct inventories at Regional Vaccine Store and coordinate inventory at District Level Methodology. Conduct a direct physical count of all available tOPV stock in the Regional Vaccine Stores. Report data on doses and not on vials, including data on the following: - Date of inventory - Stocks in doses: o In systems o Physical count - Expiration date - Manufacturer and packaging (number of doses per vial) - Physical location of the stock - Supply balances from recent SIA activities (if any) - Orders recently received or pending, which are not yet recorded in stock records Coordination of stock inventories at District level. Communicate to district-level staff their responsibilities in the inventory, including the following: o All levels should conduct their physical count within a one-week time frame to minimize the risk of double-counting stock designated for delivery down the supply chain o District staff should report (via phone call or SMS message) the total tOPV levels as outlined above Compile inventory data received from all district vaccine stores in the region, and collate together into a single database. Report information up via phone call or SMS to the Central Vaccine Store, which is responsible for collating all data nationwide. After the physical count is performed, update data in the national stock management systems with the revised, accurate figures. 2. Distribute last shipment of tOPV and first shipment of bOPV to District level, and organize redistribution within region if required Calculate quantity and distribute final orders of tOPV. Use the consumption-based formula or target population method, as described above, to calculate the amount of tOPV you must distribute to each region for the final delivery: As Switch Day draws closer, supplies should be calculated based on immunization activities planned and previous consumption, and not just based on target beneficiaries. If delivering on a quarterly schedule, use this advice for your January 2016 delivery 14 REGIONAL LEVEL Regional Vaccine Store It is recommended for the Region to provide “tOPV collection forms” (Annex 2) along with the last tOPV shipment, to be completed by Districts on [Switch day] to register all unused tOPV collected for disposal. Distribute adequate quantity of bOPV to District Vaccine Stores. Regional Vaccine Store staff must develop a distribution plan and share it with districts. In order to ensure that enough bOPV is available for administration immediately on the day of the Switch, bOPV should arrive at the District Vaccine Stores at least two weeks before the Switch. Quantities of bOPV for distribution to districts should be calculated using routine forecasting methods. Ensure that bOPV is stored separately from tOPV. In order to avoid any risk of being mixed with tOPV deliveries and administered to patients prior to the Switch, keep stocks of bOPV separate from tOPV while awaiting distribution. Store on different shelves or opposite sides of the fridge Use special tOPV stickers on tOPV secondary packaging, if available (see example in Annex 1) 3. Execute Contingency Plan To ensure that you have sufficient tOPV to last until the day of the Switch: When you receive your final tOPV delivery, conduct a physical count and compare to the total amount you will be required to distribute to each District store; If there is a shortfall in the amount you received or gap due to higher than expected demand or wastage (e.g. a temperature excursion), quantify the additional amount you require Call the identified focal point at the Central Vaccine Store and request the amount and date by when it is required (if there is insufficient time to receive the supply before delivering supply to the next level through the routine delivery schedule, Central Vaccine Store may choose to deliver directly to the level affected). 4. Dispose of excess tOPV after the Switch National planners and the Central Vaccine Store manager will communicate to you the tOPV collection and disposal plan and the role of the Regional Vaccine Store in implementing it. Provide information to design tOPV collection and disposal plan. National-level planners will take the lead in defining a tOPV collection and disposal plan, however they may call upon regional logisticians to participate in its creation. In particular, staff may be asked to: o Collect and share data about available disposal facilities and tOPV collection means at regional level o Check potential disposal sites for readiness so at regional levels the disposal plan can be adjusted if necessary Communicate disposal plan to district level and coordinate disposal (if relevant). Ensure that all selected disposal sites in the region are informed about their task and carry out the necessary preparations Ensure, through the districts if appropriate, that all health facilities in the region, including private, with tOPV receive a copy of the collection and disposal plan Dispose of tOPV in the Regional Vaccine Store. On Switch Day, regional-level logisticians must: 1. Remove any remaining tOPV from the cold chain in the regional store 2. Note the amount of tOPV removed in stock registries 3. Place in designated bags, or containers marked “tOPV for disposal” and write quantity in doses and date of removal from the cold chain on the special tOPV sticker 4. Transport it to the designated location for collection/disposal, as per the national plan for tOPV collection and disposal. 15 REGIONAL LEVEL The role of District-level staff in the Switch will be to: 1. Conduct at the minimum two tOPV inventories and report results up to the Regional Vaccine Store (or Central Vaccine Store where applicable) 2. Receive and properly store tOPV and bOPV in preparation for the Switch 3. Establish contingency plan 4. Distribute last shipment of tOPV and organize redistribution within district as required. 5. Implement Switch (three methods of distribution can be considered, detailed below: push exchange, pull exchange, and where necessary, pre-positioning) 6. Collect and dispose of excess tOPV after the Switch 1. Conduct inventories at District Vaccine Store Methodology. Conduct a direct physical count of all available tOPV stock in the District Vaccines Store. Report data on doses and not on vials, including data on the following: - Date of inventory - Stocks in doses: o In systems o Physical count - Expiration date - Manufacturer and packaging (number of doses per vial) - Physical location of the stock - Supply balances from recent SIA activities (if any) - Orders recently received or pending, which are not yet recorded in stock records Reporting. Report information up via phone call to the Regional Vaccine Store. Update data in the national stock management systems with the revised, accurate figures 2. Receive and properly store tOPV and bOPV in preparation for the Switch Ensure that bOPV is stored separately from tOPV. In order to avoid any risk of being mixed with tOPV and administered to patients prior to the Switch, keep bOPV separate from tOPV while awaiting distribution. E.g. store in different equipment if available, or on different shelves or opposite sides of the fridge Use special tOPV stickers (see Annex 1) on tOPV secondary packaging, if available 3. Establish contingency plan To ensure that all health facilities have sufficient tOPV to last until the day of the Switch, you will need to implement a system to quickly reallocate stock between health facilities when a risk of localized stock out arises. Amount required for routine immunization: When you receive your final tOPV delivery, conduct a physical count and compare to the total amount you will be required to distribute to each health facility If there is a shortfall in the amount you received or due to higher than expected demand or wastage (e.g. a temperature excursion) quantify the additional amount you require Call the identified focal point at the Regional Vaccine Store and request the additional amount and date by when you require it. 16 DISTRICT LEVEL District Vaccine Store 4. Distribute last shipment of tOPV, and organize redistribution within district if required In general, as Switch Day draws closer, supplies provided to health facilities should be calculated based on immunization activities planned and previous consumption, and not just based on target beneficiaries. In preparation, it is important to strengthen mechanisms to review vaccine utilization (and not just distribution), needs assessment and stock management. 5. Implement Switch: first shipment of bOPV to health facilities, collection of tOPV On Switch day, all health facilities must stop tOPV usage. National planners will communicate guidelines on how the Switch will be implemented in your country. An “exchange” process (either “push” or “pull”) between tOPV and bOPV is preferable, in order to avoid presence of tOPV in Health Facilities after the Switch day. However, national planners may recommend a “prepositioning” mechanism under certain circumstances, e.g. for remote facilities with difficult access (security, outbreaks, impracticable roads due to raining season). A mix of several methods may also be used. Scenario 1: Before the Switch On Switch Day (or day before) Risks Benefits* Organized “Push” - Exchange (with no Health Facility disposal) Design a micro-plan/delivery schedule to visit every Health Facility in your district on Switch Day or the day before, and secure the required transportation budget where applicable. Visit each Health Facility to: Collect any remaining tOPV in their cold chain storage and dispose of it according to guidelines and collection/disposal plan. Update stock ledgers accordingly. Put all tOPV in a plastic bag or containers marked with the appropriate sticker “tOPV for disposal” (See Annex 1). Write the quantity in doses and date of removal from cold chain on the sticker Deliver allocated bOPV supply Record the quantity of tOPV collected on the “tOPV collection form” (Annex 2). Will require significant additional funding and logistical capacity, as districts will have to make extra visits to all health facilities Approach with greatest assurance that : All health facilities receive their bOPV uniformly on time tOPV is removed from Health Facilities on time * Please note: Though districts may be using pull mechanism in normal operations, a “push” model for the Switch may be more appropriate to ensure the success and validation of the Switch, even if this may entail some extra effort on the part of the District. Scenario 2: Organized “Pull” - Exchange ( with no Health facility disposal) 17 DISTRICT LEVEL Contingency Buffer Stock: Communicate to all the Health Facilities in your district how to contact you with any unexpected additional need for tOPV Keep track of health facilities’ unused tOPV stock, in order to identify health facilities from which tOPV stock could be relocated in the event of a localized stock out. More generally, keep track on how health facilities are faring compared to recommended minimum and maximum stock levels. Increase reporting from lower levels to once a week for the last month before the switch. Be prepared to swiftly distribute or dispense any additional amount required to Health Facilities up until the Switch Day. Scenario 3: Prepositioning bOPV stock at Health Facilities Before the Switch 1 month prior: Communicate by phone, SMS or in person to every Health Facility the date and time on which they must travel to the District Vaccine Store to drop off remaining tOPV and pick up their allocation of bOPV 2 days prior: Remind all Health Facilities that they MUST bring their remaining tOPV supply in order to receive their bOPV supply Ensure that funds are available at District Vaccine Store to reimburse transportation costs for Health Facility staff to travel for the exchange On “pick Record each Health Facility that successfully exchanges its tOPV for bOPV, and record the up” day quantity of tOPV collected on the “tOPV collection form” (Annex 2). Put all tOPV in a plastic bag or containers marked with the appropriate sticker “tOPV for disposal”. Write the quantity in doses and the date of removal from cold chain on the sticker (see example in Annex 1) Record any Health Facility that forgets to bring their tOPV o If Health Facility-based disposal is NOT allowed: Do not issue bOPV and instruct them to come back the following day/or note that you will need to visit them directly to distribute bOPV and pick up tOPV o In the rare instances where HF-based disposal is allowed: Instruct them on how to destroy their remaining tOPV before issuing their bOPV After “pick The next day: Contact all Health Facilities that did not exchange, to remind them to bring up” day tOPV and pick up bOPV Within three days after Switch day: Directly visit all remaining Health Facilities to collect remaining tOPV and deliver bOPV Risks Possibility for incomplete and untimely exchange of bOPV for remaining tOPV stock, if Health Facility staff are unable/unwilling to travel on designated day Possibility of missed immunization sessions given health care worker time to travel and exchange, unless the Switch day is scheduled the day after a day-off May require additional funds for “mop up” activities on the part of the District Vaccine Store Benefits Less resource intensive for district-level staff than a full “push” delivery of bOPV On Switch Day (Least Stringent: Health Facility Disposal allowed, validation criteria is tOPV usage) Create a microplan listing each Health Facility that receives vaccine supply from you Communicate with every Health Facility regarding Switch date, and follow up with regular reminders Preposition bOPV stock through routine deliveries prior to the Switch Remind Health Facilities to store bOPV and tOPV in separate places within cold storage to reduce confusion. It is recommended to also provide health facilities with stickers “tOPV for disposal on [Switch date]” to clearly mark the secondary packaging on tOPV. (see Annex 1) Stickers should also be placed on designated disposal bags containing all tOPV on the day of the Switch. Communicate (in person, via phone, or by SMS) to each Health Facility to stop using tOPV stock and remove from the cold chain, and begin using bOPV instead. Instruct Health Facilities to put tOPV stock in a closed bag, identified with appropriate sticker “tOPV for disposal on [Switch date]”. Quantity in doses and date of removal from cold chain should also be recorded (see example in Annex 1) If Health Facility-based disposal is allowed: Instruct Health Facilities to dispose of excess tOPV according to disposal guidelines If Health Facility-based disposal is NOT allowed: Instruct Health Facilities to set tOPV bags aside 18 DISTRICT LEVEL Before the Switch Benefits for collection Incomplete and untimely exchange of bOPV for remaining tOPV stock, as there may be confusion or reluctance to Switch tOPV for bOPV Less ability to monitor actual Switch and oversee wastage disposal Less resource intensive than a full “push” or “organized pull” system, and can be performed through routine systems 6. Dispose of excess tOPV after the Switch The national or regional level will communicate the tOPV collection and disposal plan and the role of the District Vaccine Store in implementing it. Provide information to design tOPV collection and disposal plan: District-level staff may be asked to o Collect and share data about available disposal facilities at district and health facility levels, and available tOPV collection means o Check specific potential disposal sites for readiness so the disposal plan can be adjusted if necessary Communicate disposal plan to Health facilities and disposal sites, and coordinate disposal if relevant. Ensure that all selected disposal sites in the district (if any) are informed about their tasks and that they carry out the necessary preparations Ensure that all health facilities in the district, including private sector facilities, with tOPV receive a copy/are aware of the collection and disposal plan and their responsibility with respect to disposal of tOPV Communications for health facilities about tOPV collection and disposal methods can easily be included as part of the information provided about the Switch during routine vaccine distribution points. Dispose of tOPV in the District Vaccine Store. On Switch Day, district-level logisticians must: 1. Remove any remaining tOPV from the cold chain in the district store 2. Note the amount removed in stock registries (record in doses, not vials). 3. Place in bags or containers marked with the appropriate sticker “tOPV for disposal”. Write the quantity in doses and date of removal from the cold chain on the sticker. (see example in Annex 1) 4. Transport it to the designated disposal site or collection point, as per the national plan for tOPV collection and disposal. 19 DISTRICT LEVEL Risks Health Facility Staff are responsible for: 1. Communicating tOPV inventories to upper levels as required 2. Communicating any unplanned tOPV needs through the contingency mechanism 3. Executing the Switch (three scenarios detailed below) 4. Disposing of tOPV, only in the special case where Health facility-level disposal is authorized by national planners. 1. Communicate any unplanned tOPV needs through contingency mechanism In order to minimize excess tOPV that must be disposed of after the Switch, tOPV stock leading up to the Switch will be minimal. Therefore, any unexpected wastage or demand will leave a Health Facility at greater than normal risk of stock out. However, tOPV administration must continue as normal until the day of the Switch. Therefore: When you receive your final tOPV delivery, conduct a physical count and compare to the total amount you require for administration until the day of the Switch If there is a shortfall in the amount of tOPV you received or gap due to higher than expected wastage (e.g. a temperature excursion) or demand, quantify the additional tOPV amount you require Call or SMS the identified focal point at District Vaccine Store and request the additional amount and date by when you require it. 2. Execute the Switch On the day of the Switch, all health facilities must stop tOPV usage. National planners will communicate guidelines on how the Switch will be implemented in your country. An “exchange” process (either “push” or “pull”) between tOPV and bOPV is preferred, in order to avoid presence of tOPV in Health Facilities after the Switch. However, a “prepositioning” mechanism may be needed under certain circumstances, e.g. for facilities with difficult access. Scenario 1: Organized “Push” - Exchange (with no Health Facility disposal) Collect and submit all tOPV remaining in the facility’s fridge to the District representative when they arrive at the Health Facility. You must be absolutely sure not even one vial of tOPV remains in the facility. o Put all tOPV stock in a closed bag, identified with appropriate sticker “tOPV for disposal” and write the quantity in doses and date of removal from the cold chain on the sticker. (see Annex 1) o Note in stock registries the amount removed Begin administering and recording bOPV on the day of the Switch and going forward Scenario 2: Organized “Pull” - Exchange ( with no Health facility disposal) On the scheduled day communicated to you by the District Vaccine Store, travel to the District Vaccine Store with your remaining tOPV in order to pick up your allocation of bOPV. o Put all tOPV stock in a closed bag, identified with appropriate sticker “tOPV for disposal” and write the quantity in doses and date of removal from the cold chain on the sticker. o Note in stock registries the amount removed Exchange tOPV for bOPV Begin administering and recording bOPV on the day of the Switch and forward 20 HEALTH FACILITY Health Facility Level 3. Dispose of excess tOPV after the Switch After the Switch, tOPV must be rapidly disposed of to eliminate the risk of poliovirus infections. A tOPV collection and disposal plan for the country will be communicated to each health facility, including the role of Health-facility logisticians in executing this collection and disposal plan. Scenarios 1 and 2: Exchange (with no Health Facility disposal) Confirm no tOPV remains in the cold chain. As your remaining tOPV has been submitted to/collected by the District, no tOPV should remain in the cold chain at the health facility on Switch day, and the District level will ensure the disposal of the collected tOPV. Therefore, on Switch Day : Confirm that no more tOPV remains in the cold chain If for some reason a small amount of tOPV was overlooked when the tOPV was submitted to/collected by the District level: 1. Remove the tOPV from the cold chain 2. Note in stock registries the amount removed 3. Place in designated bags, or containers marked “tOPV for disposal” and write the quantities in doses and date of removal from the cold chain on the tOPV disposal sticker (see example in Annex 1) 4. Notify the District Level for guidance on collection/disposal Scenario 3: Prepositioning bOPV stock at Health Facilities Dispose of tOPV. On Switch Day: 1. Remove any remaining tOPV from the cold chain equipment 2. Note in stock registries the amount removed 3. Place in designated bags, or containers marked “tOPV for disposal” and write the quantities in doses on the sticker 4. Transport it to the designated location for collection/disposal OR set aside for collection by District, as per the tOPV collection and disposal plan 21 HEALTH FACILITY Scenario 3: Prepositioning bOPV stock at Health Facilities In order to avoid any risk of being mixed with tOPV and administered to patients prior to the Switch, make sure to keep bOPV separate from tOPV before the Switch. On the scheduled day communicated to you by the District Vaccine Store, remove tOPV from the cold chain and dispose/set aside according to guidelines (TBD) o Put all tOPV stock in a closed bag, identified with appropriate sticker “tOPV for disposal” and write the quantity in doses on the sticker. (see example in Annex 1) Begin administering and recording bOPV on the day of the Switch and forward Annex 1: Labelling of tOPV bags/containers for disposal Bags or containers for tOPV that has been removed from the cold chain after the national switch day should be clearly marked as not for use. It will be essential for any labelling to also show the date after which tOPV should not be used. Below is an example of such a sticker for labelling purposes. Countries may also wish to print stickers for labelling secondary packaging on tOPV prior to the Switch, to clearly distinguish it from bOPV and mark for disposal on Switch Day. Date withdrawn from cold chain:_______ Quantity in doses: ___________________ 22 Annex 2: Sample tOPV collection form It is recommended that Districts keep a record of all tOPV collected from each facility on Switch day. If Districts will be passing the tOPV up to a higher level (regional or central) for disposal, these forms should be modified for use at the regional and/or central levels to record tOPV collection as well. tOPV Collection Form – District level Name/ID of Facility District Name: Quantity of tOPV collected (# doses) 23 Signature of responsible staff Date