Health Disparities Among the Mentally Ill Prepared for Psychiatry Research Day
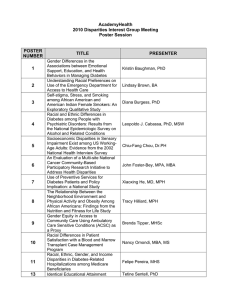
advertisement

Health Disparities Among the Mentally Ill Prepared for Psychiatry Research Day October 21, 2009 Rosalie A. Torres Stone Assistant Professor of Psychiatry Psychiatry Department Center for Mental Health Services Research Mortality and Morbidity and Preventable Conditions • Patients with severe mental illness (SMI) such as schizophrenia, die 25 years earlier than the general population. Suicide and injury account for about 30-40% of excess mortality (NASMHPD Report 2006) • In Massachusetts 1998 – 2000, among persons 25 to 44, cardiovascular mortality was 6.6 times higher among DMH clients than the general population (the deceased population was more likely to be younger, less educated and African American) (NASMHPD 2006) • Largely due to treatable medical conditions (cardiovascular, metabolic disorders, diabetes and infectious diseases) • Modifiable risk actors such as tobacco use (Vanable, Carey et. al. 2003; de Leon and Diaz, 2005), alcohol use and misuse, obesity, diabetes, (Goff, Cather et al. 2005), poor nutrition, infrequent physical activity (Daumit, Goldberg et al., 2005), and in some cases the medication itself Other Factors associated with increased risk of morbidity and mortality • Higher rates of vulnerability factors: homelessness, victimization/trauma, unemployment, poverty, incarceration, social isolation • Lack of access to appropriate care and lack of coordination between mental health and general health care providers (patient, provider, system level factors) • However, co-occurrence of diabetes and depression disproportionately affects low-income Hispanics served in primary care. Among Latinos, Type 2 diabetes is the 5th leading cause of death (CDC 2004) • Puerto Ricans have the highest rates compared to other Latino subgroups particularly those with less than high school education (Burrell et. al. 2009; Smith and Barnett 2005) • The increased prevalence is thought to be due to poorer control of blood sugar levels, lower access and quality of diabetes care, cultural, social and perhaps, inactivity and genetic factors (NASMHPD 2006) IOM Report • The IOM (2003) reported that minorities were less likely to receive the health care they needed even after taking into account health insurance coverage and other economic and health factors. • The findings indicated that health disparities goes beyond “access” issues (Smedley 2008). • What others factors contribute to racial and ethnic health disparities? ….factors outside the health care arena Patterns of Behavior Embedded in a Social Context • In a recent study, Cabassa et. al. (2008) examined the explanatory models of depression, perceived relationships between diabetes and depression, and depression treatment experiences of low income, Spanish-speaking Hispanics with diabetes and depression. In this study: • The respondents perceived depression as a serious condition linked to the accumulation of social stressors. • The respondents perceived a reciprocal relationship between diabetes and depression. • Depression interfered with self care behaviors and management of diabetes. Sociocultural Context • In addition, the respondents feared the addictive and harmful properties of antidepressants and worried about taking too many pills and the stigmas attached to taking antipsychotic medications. These concerns were prevalent in their communities. • This study highlighted the importance of understanding the social dimensions surrounding the experience of depression in developing treatments, engaging Hispanic patients and improving treatment adherence. Racial Inequality and Community Level Factors • Racial disparities in health should be understood not only in individual characteristics but in patterned racial inequalities in exposure to societal risks and resources (Williams and Jackson 2005) • The residential concentration of African Americans is high and distinctive • The related inequities in neighborhood environments, socioeconomic circumstances, and access to medical care are all important factors in initiating and maintaining racial disparities in health. Social and Community Level Considerations • Perceptions of neighborhood safety is associated with physical exercise, and this association is greater for minority group members than whites. • Access to recreational facilities, green space? • Availability of cost of health products in grocery stores • Tobacco and alcohol are heavily marketed in low income areas. Policy Recommendations We need policies to address the social and community level determinants of health disparities in underserved communities. • • • • • • • • Strategies to improve coordination of relevant state agencies (e.g., education, housing, employment, and poverty) State can create incentives for better food resources in underserved communities Promote community level interventions for health-behavior promotion (e.g., smoking cessation and exercise) Monitoring environmental degradation Expand health care coverage Improve the capacity and number of providers in underserved communities Increase knowledge base on causes and interventions to reduce it (e.g., teach disease prevention) Provide training and reimbursement to community health educators Conclusion Health is shaped by many factors from the biological, the social and political. Elimination health disparities is complex: • Insurance coverage, access or quality of care • Intertwined with race, social class and gender relations • Providing equity involves health plan purchaser, payers, and providers of care What we know: Inequities result in loss of productivity, use of services at a later stage of illness, and health care and social costs to all.