Alzheimer Disease
advertisement

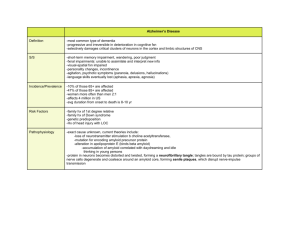
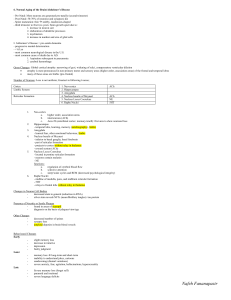
Alzheimer Disease Senile dementia of the Alzheimer type (SDAT), or Alzheimer disease (AD) is becoming more common in developed nations as the population includes more and more older persons. There is no known cause for the disease. It is often not known why some people present as early as 30 or 40 years of age with dementia while others do not present until their late 70's or 80's. At age 60 less than 1% of persons have AD, but by age 85 a fourth to a third of persons have evidence for AD. Thus, in aging populations, AD becomes more prevalent. Familial cases with a defined inheritance pattern account for about 10% of Alzheimer disease. Genetic defects in familial cases have been identified on 4 chromosomes (Blennow et al, 2006): Chromosome Gene 21 Amyloid Precursor Protein (APP) 19 Apolipoprotein E (ApoE) 14 Presenilin 1 (PSEN1) 1 Presenilin 2 (PSEN2) The so-called "early onset" cases of AD in persons in their 30's, 40's, and 50's may have a genetic basis, linked to the APP, PSEN1, and PSEN2 genes. AD cases linked to an APP genetic defect on chromosome 21 may explain the appearance of Alzheimer disease in persons with Down syndrome surviving to middle age. APP encodes for amyloid precursor protein, resulting in fibrillar aggregates of betaamyloid that is toxic to neurons. About half of early onset AD cases are linked to mutations in the presenilin 1 gene on chromosome 14. A presenilin 2 gene has been discovered on chromosome 1, but this defect accounts for less than 1% of cases. (Ertekin-Taner, 2007) The more typical "late onset" cases of AD occurring after age 60 may have underlying genetic defects. A genetic locus on chromosome 19 encodes for a cholesterol transporter called apolipoprotein E (apoE). The E4 variant of apoE, which increases deposition of fibrillar betaamyloid, can be found in 40% of AD cases. However, the presence of apoE4 is neither necessary nor sufficient for development of AD, so testing for it is not warranted. Mutations in the tau gene which codes for tau, a protein that is associated with microtubules, can be found in some AD cases. The abnormal tau may account for helical filaments found in neurofibrillary tangles. (Ertekin-Taner, 2007) Regardless of the cause, the diagnosis of AD is made clinically by the finding of progressive memory loss with increasing inability to participate in activities of daily living. Late in the course of the disease, affected persons are not able to recognize family members and may not know who they are. The definitive diagnosis is made pathologically by examination of the brain at autopsy. Grossly, there is cerebral atrophy, mainly in frontal, temporal, and parietal regions. As a consequence, there is ex vacuo ventricular dilation. The confirmation of a diagnosis of AD is made at autopsy. The pathognomonic microscopic feature of AD is an increased number of neuritic plaques in the cerebral cortex. These neuritic plaques are composed of tortuous neuritic processes surrounding a central amyloid core. Reactive astrocytes and microglia may appear at the periphery of these plaques. Though plaques may easily be found in the hippocampus, their presence in increased numbers in neocortex is necessary for a diagnosis of AD. The amyloid core consists primarily of a small peptide known as Aß which is derived from the larger amyloid precursor protein (APP). Plaques that have the amyloid proteins but lack the neuritic processes are known as diffuse plaques, which do not count toward the diagnosis of AD. Since the number of plaques increases with age, the number needed for diagnosis of AD is agedependent. Other histologic features of AD include neurofibrillary tangles, amyloid angiopathy, and granolovacuolar degeneration. (Mirra et al, 1993) (Perl, 2000) Biochemical evidence points to a loss of the choline acetyltransferase and acetylcholine in the cerebral cortex of patients with Alzheimer disease. Many treatment strategies are based upon reducing the loss of acetylcholine. However, such medications appear to be able to produce moderate symptomatic benefits but not to stop disease progression. There is loss of higher brain functions with AD leading to profound dementia. The course is usually over 5 to 7 years. The immediate cause of death for most persons with Alzheimer disease is pneumonia, typically an aspiration pneumonia. (Klafki et al, 2006