Activity and Exercise Dr. Abdul-Monim Batiha Assistant Professor Critical Care Nursing
advertisement

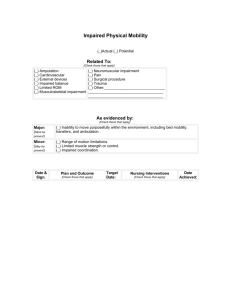
Activity and Exercise Dr. Abdul-Monim Batiha Assistant Professor Critical Care Nursing Philadelphia university Describe four basic elements of normal movement. Four Basic Elements of Normal Movement Body alignment (posture) Joint mobility Balance Coordinated movement Body Alignment/Posture Brings body parts into position that promotes optimal balance and body function Person maintains balance as long as line of gravity passes through center of gravity and base of support Figure 44-1 The center of gravity and the line of gravity influence standing alignment. Joint Mobility ROM is maximum movement possible for joint ROM varies and determined by: Genetic makeup Developmental patterns Presence or absence of disease Physical activity Coordinated Movement The mechanisms involved in maintaining balance and posture are complex and involve informational inputs from the labyrinth (inner ear), from vision (vestibuloocular input), and from stretch receptors of muscles and tendons (vestibulospinal input). Mechanisms of equilibrium respond, frequently without awareness. Proprioception Awareness of posture, movement, changes in equilibrium and awarness of Knowledge of position, weight, resistance of objects in relation to body Balance Smooth, purposeful movement Result of proper functioning of cerebral cortex, cerebellum, basal ganglia Cerebral cortex initiates voluntary movement Cerebellum coordinates motor activity Basal ganglia maintains posture Differentiate isotonic, isometric, isokinetic, aerobic, and anaerobic exercise. Isotonic (Dynamic) Exercise Muscle shortens to produce muscle contraction and active movement Increase muscle tone, mass, and strength Maintain joint flexibility and circulation Heart rate and cardiac output increase Most physical conditioning exercises (e.g., running and walking) are isotonic ADLs and active ROMs. Isometric (Static or Setting) Exercise Muscle contraction without moving the joint (muscle length does not change) Involve exerting pressure against a solid object Produce a mild increase in heart rate and cardiac output No apparent increase in blood flow to other parts of the body Figure 44-31 Example of an isometric exercise for the knees and legs. The client sits or lies on a flat surface with the legs straight out. Using a rolled towel between the knees, the person pushes the knees together and tightens the muscles in the front of the thighs by forcing the knees downward and holding for 10 seconds. Example of isometric would be extending leg in supine position, tensing the thigh muscle, and pressing the knee against the bed, holding it for several seconds. Isokinetic (Resistive) Exercise Muscle contraction or tension against resistance Can either be isotonic or isometric Person moves (isotonic) or tenses (isometric) against resistance An increase in blood pressure and blood flow to muscles occurs e.g. chest muscles may be increased in sized and strength by lifting weights Aerobic Exercise Amount of oxygen taken in the body is greater than that used to perform the activity Improve cardiovascular conditioning and physical fitness Anaerobic Muscles cannot draw enough oxygen from the bloodstream Anaerobic pathways are used to provide additional energy for a short time Used in endurance (toleration) training for athletes Compare the effects of exercise and immobility on body systems. Effect on the Musculoskeletal System Exercise Maintain size, shape, tone, and strength of muscles (including the heart muscle) Nourish joints Increase joint flexibility, stability, and ROM Maintain bone density and strength Immobility Disuse osteoporosis Disuse atrophy Contractures Stiffness and pain in the joints Effect on the Cardiovascular System Exercise Increases heart rate, strength of contraction, and blood supply to the heart and muscles Mediates the harmful effects of stress Immobility Diminished cardiac reserve Increased use of the Valsalva maneuver Orthostatic (postural) hypotension Venous vasodilation and stasis Dependent edema Thrombus formation Effect on the Respiratory System Exercise Increase ventilation and oxygen intake improving gas exchange Prevents pooling of secretions in the bronchi and bronchioles Immobility Decreased respiratory movement Pooling of respiratory secretions Atelectasis Hypostatic pneumonia Effect on the Metabolic/Endocrine System Exercise Elevates the metabolic rate, thus increasing the production of body heat and waste products and calorie use Decrease serum triglycerides and cholesterol Stabilize blood sugar and make cells more responsive to insulin Immobility Decreased metabolic rate Negative nitrogen balance Anorexia Negative calcium balance Effect on the Gastrointestinal System Exercise Improves the appetite Increases gastrointestinal tract tone Facilitates peristalsis Immobility Constipation Effect on the Urinary System Exercise Promotes blood flow to the kidneys causing body wastes to be excreted more effectively Prevents stasis (stagnation) of urine in the bladder Immobility Urinary stasis Renal calculi Urinary retention Urinary infection Effect on the Immune System Exercise Pumps lymph fluid from tissues into lymph capillaries and vessels throughout the body Increases circulation through lymph nodes where destruction of pathogens and removal of foreign antigens can occur Strenuous exercise may reduce immune function, leaving a window of opportunity for infection during recovery phase Effect on the Psychoneurologic System Exercise Elevates mood and relieving stress and anxiety across the lifespan Improves quality of sleep for most individuals Immobility Decline in mood elevating substances Perception of time intervals deteriorates Problem-solving and decision-making abilities may deteriorate Loss of control over events can cause anxiety Effect on Cognitive Function Exercise Positive effects on decision-making and problem-solving processes, planning, and paying attention Induces cells in the brain to strengthen and build neuronal connections Other Effects of Exercise and Immobility Evidence that certain types of exercise increase spiritual health Immobility causes reduced skin turgor and skin breakdown Identify factors influencing a person’s body alignment and activity. Factors Affecting Body Alignment, Mobility, and Daily Activity Level Growth and development Nutrition, personal values, and attitudes External factors (such as temperature, humidity, availability of recreational facilities and safety of the neighborhood) Prescribed limitations (such as casts, braces, traction, activity restrictions including bed rest) Assess activity-exercise pattern, alignment, mobility capabilities and limitations, activity tolerance, and potential problems related to immobility. Assessment of Activity and Exercise Nursing history Physical examination of the following: Body alignment Gait Appearance and movement of joints Capabilities and limitations for movement Muscle mass and strength Activity tolerance Problems related to immobility Figure 44-40 A standing person with A, good trunk alignment; B, poor trunk alignment. The arrows indicate the direction in which the pelvis is tilted. Figure 44-40 (continued) A standing person with A, good trunk alignment; B, poor trunk alignment. The arrows indicate the direction in which the pelvis is tilted. Develop nursing diagnoses and outcomes related to activity, exercise, and mobility problems. Mobility problems Nursing Diagnoses for Activity and Exercise Problems Activity intolerance Risk for activity intolerance Impaired physical mobility Sedentary lifestyle Risk for disuse syndrome NANDA Diagnoses: Mobility Problem Becomes the Etiology Fear (of falling) Ineffective coping Low self-esteem Powerlessness Risk for falls Self-care deficit Prolonged Immobility Ineffective airway clearance Risk for infection Risk for injury Risk for disturbed sleep pattern Risk for situational low self-esteem Examples of Desired Outcomes (NOC labels) Activity tolerance Body positioning Bowel elimination Fall prevention behavior Immobility consequences both physiological and psycho-cognitive Joint movement Mobility Respiratory status Ventilation and gas exchange Self-care Sleep Stress level Weight control Overall Goals for Problems Related to Mobility or Activity Increased tolerance for physical activity Restored or improved capability to ambulate and/or participate in ADLs Absence of injury from falling or improper use of body mechanics Enhanced physical fitness Absence of any complications associated with immobility Improved social, emotional, and intellectual wellbeing may be appropriate as the diagnostic label or as the etiology for other nursing diagnoses. NANDA includes the following nursing diagnostic labels for activity and exercise problems: Activity Intolerance, Risk for Activity Intolerance, Impaired Physical Mobility, Sedentary Lifestyle, and Risk for Disuse Syndrome . Use safe practices when positioning, moving, lifting, and ambulating clients. Safe Practice for Positioning, Moving, Lifting, Ambulating Clients Correct body mechanics required for nurse to prevent injury Correct body alignment for the client also so that undue stress is not placed on the musculoskeletal system General Guidelines for Moving and Lifting: Before moving, assess If indicated, use pain relief modalities Prepare any needed assistive devices Plan around encumbrance (obstacles) Be alert to the effects of any medications Obtain required assistance Explain the procedure to the client General Guidelines for Transferring a Client Plan what to do and how to do it Obtain essential equipment before starting Remove obstacles Explain the transfer to the client and nursing personnel who are assisting Support or hold the client rather than the equipment Explain step-by-step what the client should do Make a written plan including the client’s tolerance Transferring Between Bed and Chair Transferring Between Bed and Stretcher General Guidelines for Ambulating Assess the amount of assistance the client will require Assess for signs and symptoms of postural (orthostatic) hypotension and take appropriate action Prepare the client for ambulation Appropriately assist the client to ambulate Apply a transfer or walking belt Physically support the client Obtain assistance of other nursing personnel to follow with a wheelchair or to assist with physical support Teach the client to correctly use mechanical aids for walking Assisting the Client to Ambulate Figure 44-42 A, Balance is maintained when the line of gravity falls close to the base of support. B, Balance is precarious when the line of gravity falls at the edge of the base of support. C, Balance cannot be maintained when the line of gravity falls outside the base of support. Figure 44-42 (continued) A, Balance is maintained when the line of gravity falls close to the base of support. B, Balance is precarious (unstable) when the line of gravity falls at the edge of the base of support. C, Balance cannot be maintained when the line of gravity falls outside the base of support. Figure 44-42 (continued) A, Balance is maintained when the line of gravity falls close to the base of support. B, Balance is precarious when the line of gravity falls at the edge of the base of support. C, Balance cannot be maintained when the line of gravity falls outside the base of support. Figure 44-43 EZ Lift is an electric client lift that functions to lift clients from bed, chair, toilet, and floor. Figure 44-46 Lifting heavy objects from the floor to waist level. A, Stand close to the load and flex the back and the knees, lowering the body to grasp the load. B, Begin lifting with the back flexed, and gradually straighten the knees so that the leg muscles bear most of the burden. C, To hold or walk with the object, maintain a less flexed but not a completely straight position. Figure 44-47 Low Fowler’s (semi-Fowler’s) position (supported). Note that arm support is omitted in this instance. The amount of support depends on the needs of the individual client. Figure 44-48 Orthopneic position. Figure 44-49 Dorsal recumbent position (supported). Figure 44-50 Prone position (supported). Figure 44-51 Lateral position (supported). Figure 44-52 Sims’ position (supported). Figure 44-52 (continued) Sims’ position (supported). Figure 44-53 A one-piece seat hydraulic lift. Figure 44-54 Supporting the limb above and below the joint for passive exercise. Figure 44-55 Holding limbs for support during passive exercise: A, cupping; B, cradling. Figure 44-55 (continued) Holding limbs for support during passive exercise: A, cupping; B, cradling. Figure 44-56 Tensing the quadriceps femoris muscles before ambulation. Figure 44-57 A quad cane. Figure 44-58 Steps involved in using a cane to provide maximum support. Figure 44-58 (continued) Steps involved in using a cane to provide maximum support. Figure 44-59 Steps involved in using a cane when less than maximum support is required. Figure 44-59 (continued) Steps involved in using a cane when less than maximum support is required. Figure 44-60 A, standard walker. B, Two-wheeled walker. A Figure 44-60 (continued) A, standard walker. B, Two-wheeled walker. B Figure 44-61 Types of crutches: axillary, Lofstrand, and platform. Figure 44-62 The standing position for measuring the correct length for crutches. Figure 44-63 The tripod position. Figure 44-64 The four-point alternate crutch gait. Figure 44-65 The three-point crutch gait. Figure 44-66 The two-point alternate crutch gait. Figure 44-67 The swing-to crutch gait. Figure 44-67 (continued) The swing-to crutch gait. Figure 44-68 The swing-through crutch gait. Figure 44-68 (continued) The swing-through crutch gait. Figure 44-69 A client using crutches getting into a chair. Figure 44-70 Climbing stairs: placing weight on the crutches while first moving the unaffected leg onto a step. Figure 44-71 Descending stairs: moving the crutches and affected leg to the next step.