Global TB control
Progress and challenges
Reaching all TB patients
Quality TB care for all
DOTS Expansion Working Group
Paris 15 October 2008
Léopold BLANC WHO/STB/TBS
Estimated TB incidence rate, 2006
West Pacific 21%
Estimated new TB cases
(all forms) per 100 000
population
Americas 4%
No estimate
0–24
25–49
Africa
31%
SE Asia 34%
East Mediterranean 6%
50–99
100–299
300 or more
Europe 5%
The boundaries and names shown and the designations used on this map do not imply the expression of any opinion whatsoever on the part of the World Health
Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries.
Dotted lines on maps represent approximate border lines for which there may not yet be full agreement.
WHO 2006. All rights reserved
Global TB Control Targets
2015: Goal 6: Combat HIV/AIDS, malaria and other diseases
Target 8:
Indicator 23:
Indicator 24:
to have halted by 2015 and begun to reverse the
incidence…
incidence, prevalence and deaths associated with TB
proportion of TB cases detected
and cured under DOTS
2015: 50% reduction in TB prevalence and deaths by 2015
2050: elimination (<1 case per million population)
Latest global TB estimates - 2006
Estimated
number of
cases
All forms of TB
Greatest number of cases in Asia;
greatest rates per capita in Africa
New Smear positive
Cases
reported
DOTS
9.15 million
5.27 million
(139 per 100,000)
(80 per 100,000)
4.1 million
2.5 million
(61%)
Multidrug-resistant
TB (MDR-TB)
489,000
HIV-associated TB
709,000 (8%)
23,353
??
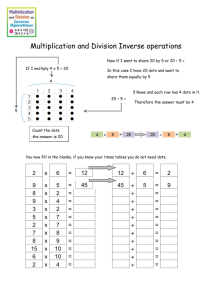
DOTS and overall SS+ case detection
a flattening curve
80
2.5 million
detected and
notified out
of 4.1 million
estimated
all notified
DOTS
60
40
100
80
60
40
20
0
20
77 69
67
52 52 46
Global Plan:
65% in 2006
78% by 2010
0
1990
1995
2000
2005
2010
Treatment success target reached in
2005 (globally, DOTS programmes)
79
83
85
80
79
77
244,662
78 77
74
82 82 82
84
2.34 million
81
82
2005
2004
2003
2002
2001
2000
1999
1998
1997
1996
1995
70
1994
Percentage
86
Europe: 71%, Africa: 76%, Americas: 78%
TB prevalence and mortality
Prevalence
Mortality
35
300
250
200
150
Target = 148
100
50
Deaths per 100,000 population
Cases per 100,000 population
350
30
25
20
15
Target = 14
10
5
Total deaths from TB
in 2006 = 1.65 million
0
0
1990 1995 2000 2005 2010 2015
1990 1995 2000 2005 2010 2015
Falling… but need to fall faster to reach targets
Incidence rates stable or falling slowly
400
Cases per 100,000 population
350
300
250
10
8
6
4
2
0
Cases in millions
9.15
Africa
South-East Asia
WORLD
200
Western Pacific
150
100
Eastern
Mediterranean
Europe
50
Americas
0
The STOP TB Strategy
1. Pursue high-quality DOTS expansion and enhancement
•
Political commitment with increased and sustained financing
•
Early case detection through quality assured bacteriology
•
Standardised treatment, with supervision and patient support
•
An effective drug supply and management system
•
Monitoring & evaluation system, and impact measurement
2. Address TB-HIV, MDR-TB and other challenges
TB/HIV collaborative activities
Prevention and control of multidrug-resistant TB
Addressing TB contacts, prisoners, refugees, and other highly vulnerable groups and special situations
3. Contribute to health system strengthening
Active participation in efforts to improve system-wide policy, human resources, financing, management, service
delivery, and information systems
Sharing of innovations that strengthen systems, including the Practical Approach to Lung Health (PAL) and infection
control in congregate settings
Adaptation of innovations from other fields
4. Engage all care providers
Public-public, and public-private mix (PPM) approaches, including NGOs, FBOs and professional societies
International Standards for TB Care
5. Empower people with TB, and communities
Advocacy, communication and social mobilization
Community participation in TB Care
Patients' Charter for Tuberculosis Care
6. Enable and promote research
Programme-based operational research and introduction of new tools into practice
Research to develop new diagnostics, drugs and vaccines
The Stop TB strategy in a framework
Political commitment with
increased and sustained
financing
2. TB-HIV, TB contacts,
prisoners, refugees,
vulnerable groups,
special situations
1. High quality DOTS (ISTC)
Susceptible or resistant (MDR-XDR)
adult or children
5. Empower
people with TB,
communities
ACSM, CTBC,
Patient charter
• Case detection through quality
assured bacteriology
• Effective (std) treatment, with
supervision and patient support
• Effective drug supply and
management system
• Monitoring & evaluation system,
impact measurement
6. Enable and promote research
New diagnostics, drugs, vaccines
Re-tooling, OR
3. Contribute to HSS
HR , Financing, PAL,
Laboratory, IC etc…
4. Engage all
care providers
(PPM)
What are the key challenges to
increasing case detection?
• About 40% (3 – 5.6 M) of estimated cases
are not notified (and not diagnosed?)
• Are the cases not notified or not identified?
Identified but not notified: in health sector but
not in DOTS providers
Not notified because not identified : informal
care providers, home, etc….
Contribution of case recovery into the NTP by
different care providers, Yogyakarta, 2000-2004
Courtesy: Dr Jan Voskens, KNCV, Indonesia
Contribution of case recovery into the NTP by
different care providers, Mumbai, 1999-2003
70
Annualised rate NSP / 100,000
60
40% increase by PPM
providers
50
TB hosp DOT
NGOs
Med colleges DOT
Mumbai PP
40
30
Mumbai RNTCP
20
10
Quarter
Source: RNTCP, Mumbai, India
4Q2003
3Q2003
2Q2003
1Q2003
4Q2002
3Q2002
2Q2002
1Q2002
4Q2001
3Q2001
2Q2001
1Q2001
4Q2000
3Q2000
2Q2000
1Q2000
4Q1999
3Q1999
2Q1999
1Q1999
0
Annualised rate of ss+ cases diagnosed per 100,000
Contribution of case recovery into the NTP by
different care providers, Bangalore, 1999-2005
160
140
120
NGO
100
Private
80
Corporate
Medical college
60
Other Government
Health Department
40
20
0
05q3
05q1
04q3
04q1
03q3
03q1
02q3
02q1
01q3
01q1
00q3
00q1
99q3
99q1
Quarter
•Public and private medical colleges (yellow) diagnose a huge number of cases, but many of them are from outside the city
and need to be refereed for treatment elsewhere.
•The increase in diagnosed cases represents increased notification after medical colleges and other providers started to
report to NTP in a standardised way
The stop TB strategy not
broadly implemented
•
TB/HIV: systematic provision of HIV test not yet widely
implemented in areas with high HIV prevalence
•
MDR-TB management limited to small projects except in
few countries
•
Involvement of non public health care providers in TB
control still limited (scaling-up PPM in only few countries)
•
•
Human resources crisis in Africa in particular
•
Patient charter available in very limited number of
countries
Community involvement still timid in many countries.
Patients groups just starting
Key issues
• Case notification not increasing in many settings
• >= 85% success rate obtained in many DOTS countries
• Need to accelerate efforts in TB control by:
– continue increasing treatment success
– aiming at reaching all TB patients
– shorten diagnostic delay (cut transmission, reduce suffering): no
indicator of delay in diagnostic
• A proposed framework to identify required actions to
improve case detection and reduce delays
Conceptual framework for improved and
early case notification/detection
TB and Poverty
DOTS / MDR/HIV
Expansion
Minimize
Effective TB screening in
access
health services, on broader
barriers
indication
ACSM
Community
engagement
HSS/HR
PPM
Health
education
Symptoms
recognised
Patient
delay
Health care
utilisation
Paediat. TB
PAL
Improve
Lab
diagnostic Srtength
quality, new
tools
Short-cut
Active TB
Active case finding
Contact
investig
Infected
TB determinants
TB/HIV
-Children
-Other risk
groups
-All household
-Workplace
-Wider
Diagnosis
Clinical risk
Risk
groups
populations
-HIV
-Previous TB
-Malnourished
-Smokers
-Diabetics
-Drug abusers
-Prisons
-Urban slums
-Poor areas
-Migrants
-Workplace
-Elderly
Notification
Improve
referral
and
notification
systems
New diagnostic tools
Infection control
Proposing a framework for
priority setting
1.
Intensify effective case identification on broader indications and ensure current policy is
followed throughout health system
2.
Target cases already diagnosed but not notified under DOTS
–
Expansion / intensification of DOTS, MDR-TB management, PPM, TB/HIV
–
Improve referral and notification systems, regulation and enforcement
3.
Improve diagnostic capacity and quality (in whole health system)
–
Effective use of existing tools for diagnosing drug-susceptible and drug-resistant TB
–
Implement new tools
4.
Reinforce current strategy for active case finding and broaden it
–
Broaden contact investigation
–
Broaden indication for screening of additional clinical risk groups beside HIV
–
Screening in risk populations in particular HIV infected persons
–
Reinforce household contact investigatio
5.
Improve health education and social mobilization to improve knowledge and rational
health seeking