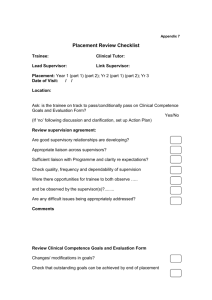
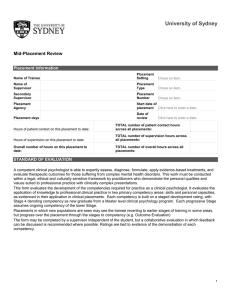
University of Sydney End-of-Placement Review Placement Information
advertisement

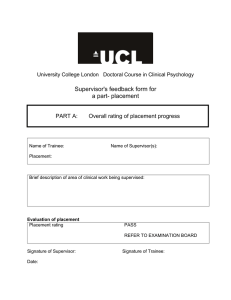
University of Sydney End-of-Placement Review Placement Information Name of Trainee Placement Setting Chose an item. Name of Supervisor Placement Type Chose an item. Secondary Supervisor Placement Number Chose an item. Placement Agency Start date of placement Click here to enter a date. Placement days Date of review Click here to enter a date. Hours of patient contact on this placement: TOTAL number of patient contact hours across all placements: Hours of supervision on this placement: TOTAL number of supervision hours across all placements: Overall number of hours on this placement: TOTAL number of overall hours across all placements: STANDARD OF EVALUATION A competent clinical psychologist is able to expertly assess, diagnose, formulate, apply evidence-based treatments, and evaluate therapeutic outcomes for those suffering from complex mental health disorders. This work must be conducted within a legal, ethical and culturally sensitive framework by practitioners who demonstrate the personal qualities and values suited to professional practice with clinically complex presentations. This form evaluates the development of the competencies required for practice as a clinical psychologist. It evaluates the application of knowledge to professional clinical practice in two primary competency areas: skills and personal capacities, as evidenced in their application in clinical placements. Each competency is built on a staged development rating, with Stage 4 denoting competency as new graduate from a Master level clinical psychology program. Each progressive Stage assumes ongoing competency of the lower Stage. Placements in which new populations are seen may see the trainee reverting to earlier stages of training in some areas, but progress over the placement through the stages to competency (e.g. Outcome Evaluation) The form may be completed by a supervisor independent of the student, but a collaborative evaluation in which feedback can be discussed is recommended where possible. Ratings are tied to evidence of the demonstration of each competency. 1 SELF APPRAISAL BY TRAINEE: Give your own views about your learning on this placement. Identify the areas where you feel you have demonstrated significant development, the areas in which you have been challenged, and the areas that you need to develop more strongly to reach competency. TRAINEE’S SELF-EVALUATION AREAS OF STRONGEST DEVELOPMENT ON THIS PLACEMENT: AREAS OF GREATEST CHALLENGE ON THIS PLACEMENT: AREAS FOR FURTHER DEVELOPMENT: 2 THE SUPERVISOR: Your role is to assess trainees and act as sound gate-keepers to the profession. You are required to itemise any concerns you have about the trainee’s suitability for clinical practice, slow progress, or specific areas where development is required. COMPETENCIES - Skills Assessment: Stage 1: Assesses straightforward presentations, such as anxiety and depression, following an externally cued semistructured biopsychosocial interview schedule over two sessions. Identifies significant relevant factors to explore in greater depth according to individual presentation. Stage 2: Assesses straightforward presentations with formulation commenced within two sessions. Balances appropriate breadth and depth of questioning through brief screening for impacting factors to selection and exploration of relevant factors with greater depth. Generates hypotheses related to the contributing impact of these factors. Stage 3: Completes an assessment of straightforward presentations within a single session, with sound depth and breadth, identifying individual issues of relevance and generating hypotheses in relation to impacting factors, which are shared and tested with the individual. More complex cases take longer Stage 4: Assesses complex presentations using an internalised, flexible, semi-structured interview schedule, generating hypotheses, and testing these via mini-formulations, with efficiency and focus adapted to the individual. Stage 1 Left click and hold on the arrow Stage 2 Stage 3 Stage 4 to move it to the place on the slider you wish to rate. Comment (indicate via initials a case in which this skill level was demonstrated): 3 Diagnosis: Stage 1: Assesses criteria and differentiates straightforward anxiety and depressive disorders with reference to an established taxonomy of disorders, such as the current DSM or ICD. Describes the usefulness and limitations of diagnostic systems. Stage 2: Assesses criteria and differentiates straightforward anxiety and depressive disorders with some internalised knowledge of an established taxonomy. Differentiates and diagnoses less familiar, discrete, more severe presentations (e.g. bipolar disorder, schizophrenia, borderline personality disorder) with reference to the established taxonomy of choice. Stage 3: Applies internalized knowledge of straightforward and singular complex diagnoses and is developing a working application of more complex presentations, such as personality disorders, dual diagnoses incorporating drug and alcohol disorders, and differential diagnoses. Stage 4: Identifies, assesses, differentiates and accurately diagnoses complex and unusual presentations. Describes highly complex issues and weighs complex differential diagnoses. Stage 1 Left click and hold on the arrow Stage 2 Stage 3 Stage 4 to move it to the place on the slider you wish to rate. Comment (indicate via initials a case in which this skill level was demonstrated): 4 Formulation: Stage 1: Identifies biopsychosocial background factors, maintaining factors, and triggering events for straightforward presentations, such as various anxiety and depressive disorders, according to a specific model. Develops these formulations collaboratively in a diagrammatical model with the individual. Stage 2: Develops diagrammatical formulations and writes a descriptive formulation that explains the mechanisms through which background factors influence development of disorders and how maintaining factors develop for the individual as coping mechanisms for more complex problems. Applies to clinical work the integration of theoretical models of development and maintenance of disorders with specific unique personal factors relevant for the individual for more specific complex problems (e.g. bipolar disorder, schizophrenia, borderline personality disorder). Stage 3: Applies to clinical work the integration of the theoretical and individual mechanisms of development and expression of the patient’s coping strategies that lead to and maintain their difficulties in the development, contribution and maintenance of more complex problems (e.g. personality disorders, dual diagnoses incorporating drug and alcohol disorders, and differential diagnoses). Describes the contribution of more complex factors, such as religious or cultural beliefs that impact problem development and maintenance. Stage 4: Applies to clinical work a sophisticated personalized understanding of the mechanisms of development, maintenance and triggers of an individual’s problems when unusual and complex from multiple perspectives. Communicates this understanding in a clear manner that makes sense of the complexities and individual factors and increases understanding for the patient. Stage 1 Left click and hold on the arrow Stage 2 Stage 3 Stage 4 to move it to the place on the slider you wish to rate. Comment (indicate via initials a case in which this skill level was demonstrated): 5 Treatment: Stage 1: Plans evidence-based, formulation-driven, goal directed treatment using the primary learned model to straightforward problems, such as anxiety and depression, following a specific primary model (e.g. CBT) of therapy. Applies sound skills to straightforward problems and demonstrates development of more advanced skills in the primary model. Stage 2: Applies advanced skills in primary model flexibly and responsively to more severe presentations of straight forward problems. Applies a formulation driven selection of new skills and approaches for specific individuals with more complex problems (e.g. DBT skills). Identifies and addresses factors contributing to problems (e.g. beliefs, themes, meanings, dynamics, and schemas) as they arise in session. Stage 3: Uses formulation to guide the appropriate choice of treatment and demonstrates advanced skills and creativity in the application of treatment in response to the individual’s experience. Demonstrates understanding of the limitations of all models of therapy. Addresses contributing factors as they arise in within session. Identifies complex interactions of belief systems, such as religious, cultural and social beliefs. Stage 4: Flexibly and responsively applies formulation driven understanding and ensuing models of evidence-based treatments (e.g. Schema Therapy, DBT, TFT etc.) for complex presentations, adapted to the needs of the individual, and applies the theoretical underpinnings of models to adapt and develop individually tailored and responsive interventions. Manages complex interactions of belief systems, such as religious, cultural and social beliefs. Stage 1 Left click and hold on the arrow Stage 2 Stage 3 Stage 4 to move it to the place on the slider you wish to rate. Comment (indicate via initials a case in which this skill level was demonstrated): 6 Outcome evaluation: Stage 1: Uses measures to support diagnoses and track progress in therapy. Uses standard battery of outcome measures that screen for common disorders, adding to these as required for more specific detail to support diagnosis, refine treatment and assess more unusual disorders and treatment outcomes. Stage 2: Identifies measures for less common disorders and applies these at baseline, during therapy as new disorders become evident, at handover, and at discharge to assess the trajectory of therapeutic change. Plots sessional outcomes where a specific intervention allows (e.g. SUDS ratings during exposure, amount of hair pulled for trichotillomania). Stage 3: Appropriately selects the best approach to monitor change and measure outcomes both within and across treatment sessions. Stage 4: Develops unique, meaningful and effective methods for monitoring and evaluating outcomes. Analyses outcome data for evaluation of personal performance, with the purpose of identifying areas needed for skill development, new approaches, and interventions for different presentations. Stage 1 Left click and hold on the arrow Stage 2 Stage 3 Stage 4 to move it to the place on the slider you wish to rate. Comment (indicate via initials a case in which this skill level was demonstrated): 7 COMPETENCIES – Interpersonal responsiveness (meta-competency) Stage 1: Demonstrates appropriate warmth, compassion, and empathy for suffering in a benign, accepting manner, regardless of the mode of relating of the individual. Demonstrates the capacity to be actively involved and responsive (as opposed to passive) to increase collaboration and focus of sessions. Identifies coping styles (defenses, avoidance strategies, etc.) in interpersonal dynamics and negative affect of the self and other. Stage 2: Makes sustained effort to understand the patient and their experiences and history. Demonstrates an involved, active, and appropriately responsive relating style. Identifies individuals’ coping styles and can describe these and their purpose, as they occur, to address blocks to therapy. Demonstrates attuned responsiveness to overt emotion and identifies covert, controlled or denied affect and the impact of this on relationship and response to therapy. Demonstrates tolerance and thoughtfulness in relation to negative affects of the self and other. Identifies ruptures in the therapeutic relationship and repairs basic ruptures. Stage 3: Applies accurate empathy for and understanding of the current emotional experiences and relating style of the individual, the circumstances in which these have developed, and their impact on relationships and the therapeutic alliance. Demonstrates understanding of different personality styles and the resultant needs in the therapeutic relationship (e.g. providing distance for those with more schizoid styles, and being more active with those who are difficult to contain). Differentiates empathy for current experience separately from early experience where these are disconnected for the individual and uses these appropriately. Identifies transference and countertransference reactions and repairs more difficult relationship ruptures responsively and therapeutically. Stage 4: Applies flexible, adaptive and differentiated responsivity throughout assessment, formulation and intervention. Applies sound judgement and sensitivity in work with strong, negative, controlled, covert or denied affect to develop insight and awareness. Applies knowledge and understanding of personality styles within the therapeutic relationship. Repairs therapeutic ruptures, and identifies and addresses transference reactions with acceptance, understanding, and sensitivity. Works towards healthy relating styles. Stage 1 Left click and hold on the arrow Stage 2 Stage 3 Stage 4 to move it to the place on the slider you wish to ra Comment (indicate via initials a case in which this skill level was demonstrated): 8 COMPETENCIES – Professional Ethical & Legal: Stage 1: Adheres to the profession’s Code of Ethics and to policies and procedures for the service. Conducts clinical work within an ethical, boundaried, legal framework that ensures adequate informed consent, confidentiality, security of information, and respect and concern for the rights of the patient/client. Stage 2: Identifies common ethical challenges and seeks supervision to resolve these. Addresses ethical challenges to the therapeutic relationship (e.g. personal questions, attempts at boundary transgressions, erotic transference reactions) as they arise in a therapeutic manner with the support of supervision, Manages responsibilities to multiple persons and agencies where conflicts of interest arise. Stage 3 Manages more challenging ethical issues. Addresses multiple interests as they arise. Identifies and seeks supervision for complex and conflicting issues. Stage 4: Manages reasonably complex ethical issues. Seeks supervision as required. Identifies ethical challenges readily and requires minimal guidance in addressing common problems. Stage 1 Left click and hold on the arrow Stage 2 Stage 3 Stage 4 to move it to the place on the slider you wish to rate. Comments: 9 Administrative: Stage 1: Attends to duties in a timely, reliable and responsible manner, for example, note-keeping, file-keeping, report writing, booking sessions, responding to contact, Intake Duty etc. Writes basic notes and reports that need some supervisor input and structural editing, but style is quickly learned and incorporated. Stage 2: Completes administrative demands such as note-keeping, file-keeping, and report writing punctually and efficiently. Maintains files to a professional standard, with all relevant material being added to the file immediately it is received, with minimal if any supervisor input or editing. Maintains clinic space as neat and tidy at all times; configuration of rooms is returned at the end of the day where furniture is moved; and defects are notified to appropriate person. . Stage 3: Punctually completes reports notes and reports that require little editing or supervision. File keeping requires little supervision. Reliably organises and follows up required management of patient, such as writing to referring agents, contacting other health professionals as needed, etc. Takes responsibility for presentation of clinic facilities, ensuring presentation is professional and clean and defects are rectified. Stage 4: Pro-actively resolves administrative issues that may arise and seeks and suggests improvements for the functioning of the service. Writes sophisticated reports that demonstrate insight and awareness of complexities, and are written to a professional standard. Maintains presentation of clinic space responsibly. Stage 1 Left click and hold on the arrow Stage 2 Stage 3 Stage 4 to move it to the place on the slider you wish to rate. Comments: 10 COMPETENCIES – Personal Supervision: Stage 1: Uses structure, clear direction, direct instruction, and demonstration of the application of basic approaches within the primary model of training. Manages anxiety related to evaluation adequately. Is open to and incorporates feedback into practice and is responsive to direction. Works collaboratively with the supervisor. Stage 2: Organises time efficiently in supervision. Utilises supervision to extend a solid foundation of skills, reflects on difficulties with the application and utilisation of the model, and difficulties within the therapeutic relationship. Plans sessions independently and requests feedback and direction as needed. Uses direct instruction on more advanced skills and new approaches. Evidences reflective skills yielding insight and improved performance. Is more focused on the patient, the work and relationship than their own evaluation. Is aware of the supervisor wanting to help, rather than evaluate. Stage 3 Works with little direct supervision on technique or content with familiar presentations. Demonstrates a high level of reflective skills and interest in understanding the complexities of the therapeutic relationship and the intricacies of advanced therapy. Responds to alternative ways of thinking and approaching new problems and complex presentations. Shows clear focus on the patient, not the self, and the supervisor as a support. Stage 4: Uses supervision as a sounding board for new ideas and approaches and to discuss and extend understanding of complex cases and issues. Requires and enjoys challenges to previously established ways of thinking and working. Manages time and personal needs efficiently. Stage 1 Left click and hold on the arrow Stage 2 Stage 3 Stage 4 to move it to the place on the slider you wish to rate. Comment (indicate via initials a case in which this skill level was demonstrated): 11 Each of the following personal attributes is essential for practice as a competent clinical psychologist. Where these are lacking clinical work is generally compromised, as is patient/client care. Please rate these accordingly (double click on box to fill by clicking on ‘checked’): Inadequate Needs Development Adequate Well Developed Outstanding Attendance/Punctuality: Professional dress & presentation: Appropriate confidence in role: Appropriate authority in role: Professional assertiveness: Honesty & Integrity: Knowledge of limitations: Reliability: Critical thinking: Problem solving: Perceptiveness: Sound judgement: Concise & clear communication: Verbal expression: Written expression: Organisation & time management: 12 Inadequate Needs Development Adequate Well Developed Outstanding Preparedness: Dedication: Flexibility: Adaptability: Openness: Curiosity: Responsiveness to patient: Observing capacity: Initiative: Collaboration: Respect for cultural diversity: Affect tolerance Tolerance of ambiguity: Personal Courage: Self-reflective: Accurate self-appraisal: Awareness of impacts of own personal attributes: 13 Inadequate Needs Development Adequate Well Developed Outstanding Contribution to group discussion: Collegiality with colleagues: Collaborative with other health professionals: Respect for support staff: Self-care: Care of professional environment: Where relevant: Management of personal stress & distress Management of conflict: Comments: 14 PLACEMENT PROGRESS: Whereas in the previous section, trainees were assessed based on a standard of competence, items in this section must be rated relative to performance of peers and with respect to their current stage of development. Thus “unsatisfactory”, “slow”, or “excellent” progress may be assigned to trainees at any stage of development. Please rate the trainee’s progress thus far. If progress is below levels expected, please comment on factors in the free-text section or under confidential comments below. (e.g., attitudinal barriers, personal issues including illness). Please double click the appropriate box and select ‘checked’. EXCELLENT PROGRESS The trainee has demonstrated accelerated progress across the placement, much above the rate expected at this stage of training. DEVELOPING WELL Consistent and good progress has been achieved. The rate of progress matches expectations for trainees at this stage of training. INCONSISTENT PROGRESS Progress has been inconsistent or patchy across time and/or domains, with satisfactory progress achieved some of the time/in some domains, but not all the time/across all domains. SLOW PROGRESS Some progress has been made, but progress has been uniformly slow across most domains, or has been achieved following above-average investments of staff resources. Rate of progress is below the standard expected at this stage of training. UNSATISFACTORY PROGRESS Progress is considerably slower than the pace expected at this stage of training. Consequently, little or no change has been observed in the trainee's capabilities. Major deficits in one of more areas that are of serious concern. OVERALL EVALUATION: PASS WITH MERIT (PM) The clinical practice substantially exceeds the expected level of competence for the stage of training. Reserved for work of an exceptionally high standard that demonstrates independent thought, originality and comprehensive knowledge of the subject area. In order to be awarded a ‘Pass with Merit’, a trainee needs to perform in the top 10% of MCP students, and meet all of the following requirements, in addition to the core competencies: Demonstrates an exceptional understanding of therapeutic principles and their conceptual and theoretical underpinnings; Demonstrates a superior capacity to generate hypothesis testing and formulation within the therapy session; Works independently, with minimal supervision, professionally and therapeutically; Shows initiative and creativity; Is highly professional; Contributes significantly to the supervision process and supports all members of the supervision team. PASS (P) The material or clinical practice meets the expected level of competence for the stage of training. A pass is considered to signify work that is of a good to very good standard, according to the relevant expectations. IDENTIFIED DIFFICULTIES (ID) The level of competence expected at this stage of training in professional or clinical practice has not been met in one or more areas. These competencies need to be attained to an acceptable standard before a student can be passed in the placement. A remediation plan that targets the area/s of concern needs to be developed and implemented in consultation with the Placement Coordinator. A final grade will not be awarded for the relevant placement until the competency or competencies have been attained or are unable to be remediated within a reasonable set timeframe. FAIL (F) The student has a sufficiently low level of competence that their continuation would compromise patient care. Any Unit of Study that the trainee is deemed to have failed will have to be repeated. The trainee will be required to re-enrol in any Unit of Study that they have failed. Trainees are only eligible to repeat Units of Study once. 15 Verification of Review By signing this form, you confirm that you have discussed this review with your supervisor. Signing this form does not necessarily indicate that you agree with this evaluation. Trainee’s Signature Date Supervisor’s Signature Date 16 Please help us improve this form: POSITIVE COMMENTS FROM TRAINEE & SUPERVISOR: NEGATIVE COMMENTS FROM TRAINEE & SUPERVISOR: 17