Health Care in developing world A Road Map to Paradigm Shift
advertisement

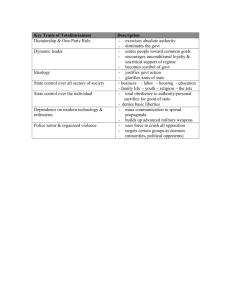
Health Care in developing world A Road Map to Paradigm Shift Prof. D K Gupta Vice Chancellor-CSMMU, (KGMU), LKO Professor and Head, Dept of Pediatric Surgery AllMS, New Delhi Where are we - today • • • • • Health – Major Disparity in the world India: Poverty, illiteracy, hygiene Population explosion Basic needs : ?? Food, water, education New Epidemic: DM, HT, Trauma, Obesity, psychiatric problems • Cancers: Infants, Children, adults, old age • 1 million pts. die globally /year : No help • High expectations – why not ?? Chronic Disease Burden • CDs result for 60% of deaths in 2005. • >80% of deaths in low to middle income countries (LMIC). • NCDs are killing more people in their prime adult years. • TB, HIV and malaria account for 10% of the global deaths. Age at death region wise Source: Global Burden of Disease, 2004 Update, used by permission Major Causes of Death, World area 1 2 3 4 5 6 7 8 9 10 Disease or Injury Ischemic heart disease Cerebrovascular disease Lower respiratory infections COPD Diarrheal diseases HIV/AIDS Tuberculosis Trachea, bronchus, lung cancers Road traffic accidents Prematurity and low birth weight Deaths/ % of total million deaths 7.2 12.2 5.7 9.7 4.2 7.1 3 5.1 2.2 3.7 2 3.5 2.5 1.5 1.3 2.3 1.3 2.2 1.2 2 Source: The Global Burden of Disease: 2004 update, WHO Life style : factors Lack of Physical exercise • 2 million deaths worldwide annually. • A causal factor for; • 10-16% breast , colon cancers, diabetes • 22% of ischemic heart disease. Overweight & Obesity WHO Report: 2.3 billion overweight adults in the world Over 700 million of them will be obese by 2015. Hypertension • Responsible for 13% of deaths world-wide. • 26% of adults had hypertension in 2000, • Expected to jump to 30% by 2025 globally • 2/3 with HTN live in developing world. Disease association with Tobacco use Source: WHO Report on Global Tobacco Epidemic, 2008 Health Problems in developing world • • • • • • • 2/3rd Population is in developing world 2 Billion children malnourished Infection, diarrhoea, Malnutrition : ??? Congenital malformations (2%) Cancers – presenting quite late Trauma – common, 90% preventable Life style disorders – common, early age - Hypertension, Diabetes, Obesity, - Psychiatric / mental health disorders Urban India – Medical Tourism Indian medical scenario • • • • • • • • Vast country – limited health facilities Facilities - Mostly in urban areas Long distances / time to travel Specialized services only to 20% population Expensive hospital stay/ medical services Limited health insurance No insurance for serious Cong. Mal., cancers, High IMR, MMR, TFR Indian scenario • • • • • Population: 1.2 billion India will cross China in 2030 ( 1.45 bn.) > 400 million children <14 yr age GDP health Share : 1.2% Now increased from 1.2% to 2% Special health issues • • • • • • 80% villages: Poor overall development Poor state of Primary, community & district Poor state of Medical college, Hospitals Poor vaccination – in rural sector Poor education, hygiene, literacy, schooling Inadequate Medical & Paramedical staff Special health problems in India • • • • • • Mean Age : M- 65 : F- 57 yr Old age: No shelter homes Communicable diseases Snake bites Disasters – Tsunami, Earth quakes, floods Very high trauma – 90% preventable 90% accidents : Preventable in children • News 26-7-2012 - KGMU Trauma Center caters to 5 neighboring states & Nepal - 9 more trauma centers Indian scenario - Preventive & Control programs : Govt. • • • Primary / Tertiary Health Care : Govt. 80% OPD services by Private sector 60% indoor beds in private sector 80%: No access to modern health care 70% cost born by the patient himself Every 7th in the world - is an Indian Medical/ Dental Colleges (recognized / un-recognized) Govt. sector Private sector Medical colleges ~160 ~ 200 ~ 360 in India Mostly Old - Mostly in 10 yrs Dental Colleges ~ 357 in India ~ 38 ~ 320 - Mostly in 20 yrs Medical Graduation – 6 years Post-Graduation -3 yrs more Super-specialty – 3 yrs more ( Total 12 years) + Fellowship ?? Tough Life of a Institutional Doctor • • • • • • • • Doctors are trusted & kept in high esteem High expectations from the Role Models Sacrifice – personal & family life No working hours for doctors - indoor service Tough life before, during and after operations Must know Recent advances Seminars, Journal clubs during training period Preparing for Lectures, Conferences, workshops, What do people want from Govt. • Reliable & Affordable Medical services • Free treatment for major problems - Cancer, Heart, Liver, kidney, transplant • Free treatment to all those who are poor • Institutions to be only as a referral center • Availability of good quality Medicines ( 30-40% medicines are spurious) • Free Medicines to all pts. in PHC / CHC ( Generic: cost, control of quality, confidence) Emphasis is on now ; • • • • • • • Improvement in Mother & child care Improve IMR from 57 to 37 Improve MMR from 388 to 200 Reduce TFR from 3.8 to 2.5 Filling the medical / staff vacant posts Develop work ethos and culture Improve competency level Strategies to improve health • Preventive and Therapeutic : Govt. Responsibility (Polio eradicated recently) • More doctors, nurses and paramedics • Medical college each of 626 districts • Generic and quality medicines – free to all • Corporate Hospitals – super-speciality • Medical Tourism Additional health Planning • • • • • • • • • Budget increased from 1.2% to 2% Ambulance : Free services, Joint Control rooms Mid day meals for school children Free Health for all Girl students National Rural health Mission National urban health Mission Public Health Foundation – BPL, Insurance Janani Baccha Suraksha Yojna (MCH Services) National Disaster Management Authority Govt. Recent efforts • 6 new AIIMS like Institutes • Incentives for PG seats for rural doctors (10 marks for 1 yr , max. 30 marks for 3 yr service) • • • • • New Medical Colleges – Govt. / Pvt. PPP Model for the Rural sector Corporate Hospitals to have PG seats. DNB – PG seats in Big hospitals 13000 UG and 4000 NEW PG seats Govt. New Incentives • • • • • • • New Colleges of Nursing Regional Institutes of Paramedical sc. 8 RIPS BRHC- Bachelor Rural Health Care: 3 yr course 18 wk training for obst. and anesthesiologists 1 yr course in Cardiology, DM, Dialysis, Insurance cover for all Aadhar / BPL cards to poor population Improving Health services • • • • - Health services – PHC, CHC, District Teaching Institutions – Govt. / Pvt. Private sector - Major share in OPD & Indoor 4 Tier Health care delivery Model PHC, CHC, District, State Level with specialists National level Hospitals for referred cases Institutes: Transplant, Heart, Liver, Kidney, children Improvement of Health services Incentives to workers in PHC/CHC: • Local staff- others • Pharmacist, Ambulance driver • Physicians and Surgeon Minimal available Medical infrastructure • Minimal facilities for the staff/ doctors • Due respect & responsibility • Trust, freedom and Autonomy Alternate model - difficult Curative and Preventive Role • PHC : Doctors in Mobile Units, staff • Counseling on Preventive programs • National disease control program • Vaccinations – mother & child care • Distributing free medicines • Referring serious pts. to higher center • NGOs, teleconferencing for help • Visitor Nurses / paramedics for FU Role of NGs to bridge the gap Education and Awareness Parental counseling • • • • • • • Keeping children away from cooking area Away from industrial hazards Keeping medicines / acids away Ban on strong acids and alkalis Ban on washing soda Use of Seat belts in vehicles Use of Cycle helmets and reflecting lamps Core Group Recommendations ; • Better designs : Roads, flyovers, school buses, • Better House designs: with high walls, better doors, windows, toilet sheets, glass panes • Adequate Covers – manholes, wells, • No to fire crackers around Deewali • No Kite flying from roof tops Gupta DK. Chairman – Core Group Recommendations to the Ministry, rd 3 World Congress on Pediatric Esophagus , AIIMS, New Delhi. 2002 International Delegation Meets Hon’ble Prime Minister of India, health concerns of Children Other health related concerns • • • • • • • • Safe drinking water to public Garbage disposal from city & villages Technically sound Roads and streets Construction of Public toilets Proper sewage disposal Proper hygiene at Rly. stations Measures to prevent CDs/ NCDs Awareness on preventing trauma Health indicators continue to be poor and high mortality rates of infants and pregnant women have been a cause of serious concern. “Government has decided to continue the National Rural Health Mission for next five years. We are now proposing a new National Urban Health Mission in order to focus on the health challenges in our towns and cities,“ Prime Minister of India, 2012 Road Map to improvement Increase in health Budget & Facilities Give Respect & Responsibility Have Trust & commitment Competency and care Expect nothing from 21st century. It is the 21st Century that expects everything from us. (Gabriel Garcia Marquez)