PERIODONTAL DISEASE AMONG COMMUNITY-DWELLING DIABETICS:
advertisement

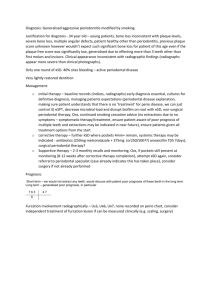
PERIODONTAL DISEASE AMONG COMMUNITY-DWELLING DIABETICS: EVIDENCE FROM A DIABETES EDUCATION AND PROMOTION EVENT by David C. Hay DMD, Temple University, 2013 Submitted to the Graduate Faculty of the Multidisciplinary MPH Program Graduate School of Public Health in partial fulfillment of the requirements for the degree of Master of Public Health University of Pittsburgh 2015 i UNIVERSITY OF PITTSBURGH GRADUATE SCHOOL OF PUBLIC HEALTH This essay is submitted by David C. Hay on March 31, 2015 and approved by Essay Advisor: David Finegold, MD Professor of Human Genetics Director Multidisciplinary MPH Program Graduate School of Public Health University of Pittsburgh _______________________________________ Essay Reader: Pouran Famili, DMD, MDS, MPH, PhD _______________________________________ Professor, Department of Periodontics and Preventive Dentistry Professor, Clinical and Translational Science Institute School of Dental Medicine University of Pittsburgh ii Copyright © by David C. Hay 2015 iii David Finegold, MD PERIODONTAL DISEASE AMONG COMMUNITY-DWELLING DIABETICS: EVIDENCE FROM A DIABETES EDUCATION AND PROMOTION EVENT David C. Hay, MPH University of Pittsburgh, 2015 ABSTRACT Periodontal disease is a chronic inflammatory condition and a major cause of tooth loss. The public health impact of periodontal disease is great. Nearly half of adults in the United States are affected by some degree of periodontal disease. The prevalence of periodontal disease increases with age and is closely related to certain systemic diseases such as diabetes. Diabetes is a chronic metabolic disease associated with a hyper-inflammatory state. Well-controlled diabetes will help to improve the periodontal condition, decreasing the public health impact of the disease. Objective. The objective of this investigation was to study the prevalence of periodontal disease in a population of community-dwelling adults attending an all-day diabetes awareness and education event. Methods. Retrospective study of periodontal disease and its relationship with diabetes. Data were collected from attendees at the Diabetes Expo in Pittsburgh, Pennsylvania, an event sponsored by the American Diabetes Association. Informed consent was obtained. iv Comprehensive periodontal examinations were performed. Information on age, gender, education, smoking, diabetes, periodontal disease, and oral health were collected and analyzed. Results. Participants = 206 individuals; 97 respondents had periodontal disease and 147 did not. Ninety-three (93) individuals (47.9%) without periodontal disease had diabetes and fifty-four (54) individuals (36.3%) did not have diabetes; this finding was not significant (p=0.847). Good oral health was important among the people attending this event. Those with good oral health had less diabetes compared to people with poor oral health; this finding was statistically significant (p=0.004). Conclusion. Retrospective investigation of periodontal disease among community-dwelling diabetics in this study revealed no significant relationship between diabetes and periodontal disease (p=0.847), although oral health was an important, significant factor (p=0.004). Further prospective research with larger sample size is recommended to confirm these findings. v TABLE OF CONTENTS 1.0 INTRODUCTION ........................................................................................................ 1 1.1 BACKGROUND ..................................................................................................2 1.1.1 Periodontal disease pathogenesis/Etiology…….……………………………2 1.1.2 Classification of disease………………………………………………………3 1.1.3 Prevalence of disease…………………………………………………………4 1.2 RISK FACTORS………………………………………......................................4 1.2.1 Bacterial plaque and host response………………………………………….4 1.2.2 Smoking ............................................................................................................ 5 1.2.3 Race ............................................................................................................ …...6 1.2.4 Gender .............................................................................................................. 6 1.2.5 Socioeconomic Status ...................................................................................... 7 1.2.6 Age..................................................................................................................... 7 1.2.7 Systemic Disease .............................................................................................. 8 vi 1.3 DIABETES PATHOGENESIS……………………………..............................9 1.3.1 Prevalence....................................................................................................... 11 1.3.2 Risk factors for diabetes................................................................................ 11 1.3.3 Periodontal disease and diabetes .................................................................. 13 2.0 METHODOLOGY..................................................................................................... 16 3.0 RESULTS ................................................................................................................... 17 4.0 DISCUSSION ............................................................................................................. 20 5.0 CONCLUSION........................................................................................................... 22 BIBLIOGRAPHY ....................................................................................................................... 23 vii LIST OF TABLES Table 1. Logistical regression test to show the association between individual covariates and the outcome of interest (Gum Disease)…........................................................................................... 18 Table 2. Multivariate logistical regression…............................................................................... 19 viii 1.0 INTRODUCTION Periodontitis is a chronic inflammatory disease of the oral cavity, which causes destruction of the periodontium. The periodontium acts as the support mechanism for the teeth and is made up of cementum, the periodontal ligament, and alveolar bone. As the periodontium is destroyed, teeth may become loose and eventually can be lost. The public health impact of periodontal disease is great. Nearly half of the United States population is affected by some degree of periodontal disease.1 A major risk factor for periodontal disease is diabetes. Diabetes is a metabolic disease where those affected either do not produce insulin or are resistant to its action. It is estimated that 27.8% of those with diabetes remain undiagnosed.2 Of those who are aware of their diabetic status, a large proportion is unable to adequately control their disease. Uncontrolled diabetes can lead to many systemic complications including damage to microvasculature and compromised healing. The connection between diabetes and periodontal disease is well documented in the literature.3-6 The systemic effects of diabetes increase susceptibility to periodontal disease, making diabetics an at-risk population for periodontitis. The public health implications of periodontal disease are great. Progressive alveolar bone loss, if left untreated, will eventually lead to tooth loss and partial or full edentulism. Decreased masticatory function can have adverse nutritional effects including decreased vegetable intake 1 and high fat, low fiber diets.7 Nutritional tendencies such as these are large factors in the quickly growing obesity epidemic in the United States. 1.1 BACKGROUND 1.1.1 Periodontal disease and pathogenesis/Etiology Periodontal disease bears the most significant burden of oral disease. It is one of the world’s most common dental diseases, highly prevalent worldwide.8,9 The primary etiology of periodontal disease is bacterial plaque. Historically, any and all plaque biofilm was thought to be disease causing. However, in 1979, Loesche presented the specific plaque hypothesis, which states that dental decay and periodontal disease appear to be due to specific bacterial infections following overgrowth of certain indigenous plaque bacteria.10 If the plaque biofilm is allowed to form and attach to the tooth surface, an immunological response is mounted by the host to combat the infection. It is due to this response that periodontal attachment in the form of cementum, periodontal ligament, and alveolar bone, is destroyed. As destruction of the periodontium progresses, the epithelial attachment to the tooth migrates down the root, forming a periodontal pocket. As the depth of the pocket increases, it becomes increasingly difficult, if not impossible, for the patient to clean. This further promotes biofilm growth and periodontal destruction. It is only once the biofilm is removed and pockets corrected that the disease process can be halted. 2 1.1.2 Classification of disease In its earliest form, periodontal disease manifests as gingivitis. Clinical signs of inflammation are notable and include edema, redness, and bleeding on probing. Histologically, inflammatory infiltrates consisting of neutrophils, lymphocytes, and plasma cells are detectable.11 In gingivitis, the inflammatory process is localized to the gingiva and does not cause destruction of the periodontium. In some cases the disease remains confined to the gingiva, however, in a susceptible patient, the lesion will progress and involve the alveolar bone. Once alveolar bone destruction has occurred, gingivitis has progressed to periodontitis. As classified by the 1999 International Workshop for a Classification of Periodontal Disease and Conditions, there are four main forms of periodontitis; chronic periodontitis, aggressive periodontitis, periodontitis as a manifestation of systemic disease, and necrotizing periodontal diseases.12 Of these, the most common form is chronic periodontitis. The degree of periodontal destruction is categorized as mild, moderate or severe. This is determined based on the amount of clinical attachment loss present throughout the dentition. Periodontitis is a progressive disease, however, not all individuals progress through the stages at the same rate. In fact, research clearly demonstrates that some patients do not progress through the stages at all. In a classic study by Löe et al. on Sri Lankan tea laborers who did not practice oral hygiene, it was discovered that 8% displayed rapid progression of periodontal disease, 81% displayed a moderate progression, and approximately 11% displayed no progression at all beyond gingivitis.13 3 1.1.3 Prevalence of disease Based on the most recent NHANES study, nearly half of the United States adult population suffers from some type of periodontal disease1. This corresponds to 64.7 million people with periodontitis. Moderate periodontitis was most common, with 30% of cases classified. Mild and severe periodontitis were found to constitute 8.7% and 8.5% of the population, respectively.1 Rates of periodontitis were highest in men, non-Asian Hispanics, smokers, adults with less than a high school education, and adults below 100% Federal Poverty Levels.1 1.2 RISK FACTORS FOR PERIODONTAL DISEASE 1.2.1 Bacterial Plaque and Host Response Bacterial plaque is the primary etiology of periodontal disease. While there is a clear, causal relationship between poor oral hygiene and gingivitis, the relationship of oral hygiene to periodontitis is less clear.14 Conclusions from numerous studies in populations with poor oral hygiene reveal that plaque accumulation correlates poorly with severe periodontitis.13, 15, 16 This has led to the more recent investigation into the critical nature of the host response in the literature. It has been discovered that bacteria are essential, but insufficient for disease and that they account for only a small proportion of the variance in susceptibility for disease expression.17 However, hereditary factors can account for roughly 50% of the variance.18 Genetic disorders 4 such as familial cyclic neutropenia, trisomy, and Papillon-Lefevre syndrome are all strongly associated with an increased susceptibility to periodontal disease due to their effects on neutrophil number or function.19 More recently, the importance of IL-1 polymorphism has been investigated. IL-1β, along with TNF-α, INF-γ, and PGE2, is greatly responsible for the destructive processes affecting the periodontium. These normally protective compounds are released by macrophages and monocytes when they become activated by lipopolysaccharide from periodontal pathogenic bacteria. Individuals with a specific IL-1 polymorphism produce about four times as much IL-1β as those who are genotype negative and are about twenty times more likely to develop severe adult periodontitis.20 1.2.2 Smoking Tobacco smoking has also been well documented as an independent risk factor for periodontal disease, when controlling for other factors such as oral hygiene. Meta-analysis on data examining the effect of smoking on periodontal attachment loss confirmed smoking as a risk factor, revealing an odds ratio of 2.8.21 Another review of the literature reveals that smokers are 2.5 to 6 times more likely to develop periodontal disease than non-smokers, and that the number of cigarettes smoked has a direct correlation with the risk of developing the disease.22 Both systemic and local effects are known to be detrimental to periodontal health. Clinically, the gingiva of smokers tends to be more fibrotic and display less bleeding, due to the decrease in vascularity of the gingiva. Smokers also tend to have larger amounts of plaque, maxillary anterior palatal attachment loss, and furcation involvement than non-smokers. It has also been reported that smokers with periodontitis suffer from more severe disease than do similar periodontitis patients who do not smoke.23 Smoking also renders non-surgical and surgical 5 treatment of periodontal disease less effective.24, 25 In fact, one study reported that approximately 90% of refractory periodontitis cases, periodontitis that does not respond at all to treatment, were in smokers.26 1.2.3 Race Based on the most recent NHANES data, periodontal disease is most common among Hispanics and non-Hispanic blacks with a prevalence of 63.5% and 59.1%, respectively. Non-Hispanic Asian Americans, with a prevalence of 50.0%, are the next most likely to be affected. The lowest prevalence reported was 40.8% among non-Hispanic whites1. These results agree with a study by Albandar et al. which demonstrated that United States subjects of African or Mexican descent have greater attachment loss than Caucasians.27 However, the true role of race as an independent risk factor for periodontal disease remains unclear, as the association is significantly reduced when accounting for other factors such as smoking and socioeconomic status.28 It is quite possible that the confounding effects of these other variables falsely represent the role of race/ethnicity in periodontal disease susceptibility. 1.2.4 Gender A generally consistent finding in all national surveys in the United States since the 1960s1, 29, 30, 31 is that periodontal disease is more prevalent among males than females. Though the true cause of this trend is unknown, the hypothesis is that males tend to practice less effective oral hygiene, visit a dentist less regularly, and have more negative attitudes about dental care than women. It is 6 unlikely that a true genetic difference predisposes males to periodontal disease more than women. 1.2.5 Socioeconomic Status As is the case with many other diseases, periodontal disease is more common among individuals of lower socioeconomic status (SES).1, 32 This historically reported relationship is likely attributable to multiple factors influenced by SES, such as education level and access to regular dental care. Oral hygiene and attitudes toward oral health are typically higher among the better educated. Higher SES groups are also more likely to have dental insurance to remove some of the financial burden of oral care. Furthermore, dentists tend to be more readily available in geographic locations with a higher SES population. Though the exact relationship is unknown, it is clear that SES is part of a complex, multifactorial group of variables along with education, location, and race, which make periodontal disease more prevalent among those of lower SES. 1.2.6 Age It is clear from multiple cross-sectional surveys1; 33-37 that the prevalence and severity of periodontal disease increase with age. For example, when examining the 2009-2010 NHANES data, it showed prevalence rates of clinical attachment loss (CAL) increase with age. In the 30-34 year old age group, prevalence of periodontitis of any severity was 24.4%. Contrast this with the ≥65 year old age group, which displayed a prevalence of 70.1%.33 Of the varying severities of periodontal disease, moderate periodontitis is the most common, with a prevalence of approximately 30%. Examining the prevalence of moderate periodontitis amongst different age 7 groups again reveals that older individuals are more likely to exhibit disease. Only 13% of those aged 30-34 years were found to have moderate periodontitis, whereas 53% of those in the ≥65 year old group were affected.33 Although this data may seem to represent periodontitis as a disease of aging, this dated theory is no longer accepted.35, 36 The current view recognizes the greater periodontal destruction observed in the elderly as reflecting lifetime disease accumulation rather than an age-specific condition.4 It is also notable that the prevalence will likely continue to rise as the United States population continues to age and, due to advances in oral care, these elderly persons retain their teeth longer into life. 1.2.7 Systemic Disease Due to the importance of the host response in the protection from periodontal pathogens, a welldocumented relationship exists between certain systemic diseases and susceptibility to periodontitis. The most well-defined relationship exists with systemic diseases which negatively affect neutrophils. The neutrophil is the central element of the host response against invading periodontal pathogens.38 Innate or acquired defects in number and/or function of neutrophils reveal the importance of this cell type to the pathogenesis of periodontitis.39 Systemic diseases affecting the number of neutrophils include agranulocytosis, cyclic neutropenia, familial benign chronic neutropenia, and systemic lupus erythematosus, among others. Diseases affecting neutrophil function include leukocyte adhesion deficiency Type I and II, Chédiak-Hagashi syndrome, Down’s syndrome, and Papillon-Lefèvre syndrome.39 Though many of these diseases are relatively rare to encounter in clinical practice, they often manifest as severe and rapid periodontal breakdown. Another well understood relationship exists between periodontitis and diabetes. This relationship has been well documented in the literature and periodontitis has been 8 labelled as a definitive complication of diabetes.40 Various mechanisms attempting to explain this relationship have been proposed and will be discussed in detail in a later section. Less clear relationships have begun to be elucidated more recently with obesity and osteoporosis. Saito et al.41 was the first to describe a potential relationship with obesity when it was discovered that patients with body-mass indexes (BMI) ≥30 had a relative risk of 8.6 for periodontitis, compared to those with BMI ≤20, after adjusting for confounding variables. A plausible mechanism is found in the discovery that adipose tissue is a complex and metabolically active endocrine organ, secreting numerous immunomodulatory factors which may affect the periodontium.42 Numerous other cross sectional studies have investigated this potential relationship with varying results. Longitudinal studies are needed to further investigate this potential relationship. Osteoporosis has also been investigated as a possible risk factor for periodontal disease, however mixed results have been obtained. It has been reported that severe osteoporosis may be associated with less than favorable attachment level in periodontal disease,43 however a more recent, longitudinal study by Famili et al. found no such association.44 1.3 DIABETES PATHOGENESIS Diabetes is a metabolic disease characterized by hyperglycemia deriving from defects of insulin secretion or insulin action. Uncontrolled diabetes can cause extreme metabolic dysfunction, up to the failure of multiple human organs, among them the kidneys, eyes, heart, nerve endings and blood vessels.45 There are two major types of diabetes, accounting for about 99% of cases; Type I and Type II. More rare forms of the disease, such as gestational diabetes, make up the remainder of cases. 9 Type I diabetes is characterized by an absolute insulin deficiency due to cellularmediated autoimmune destruction of β-cells in the pancreas.46 There are three known types of autoantibodies which contribute to β-cell destruction. Islet cell cytoplasmic autoantibodies are the primary autoantibody type, present in 90% of Type I diabetics. Their presence is highly predictive of future Type I diabetes.47 Islet cell surface antibodies are also very common in Type I diabetes cases, present approximately 80% of the time. Some patients with Type II diabetes have also been found to be Islet cell surface antibody positive.47 Specific antigenic targets of Islet cells may also be affected, with antibodies against glutamic acid decarboxylase and insulin being strongly predictive of future Type I diabetes in at risk populations.47 The onset of Type I diabetes is variable and dependent on the rate of β-cell destruction. The onset of clinical Type I diabetes marks the completed destruction of the human pancreas’ β-cells. Type II diabetes is a heterogenous disorder caused by a combination of genetic factors related to impaired insulin secretion, insulin resistance, and environmental factors such as obesity, over-eating, lack of exercise, stress and aging.48 It is widely reported as a multifactorial disease and characterized by the lack of need for insulin to prevent ketoacidosis.47 In contrast to Type I, it is not considered to be of autoimmune etiology. Normally, plasma glucose concentrations are maintained within a narrow range through a tightly regulated interaction between tissue sensitivity to insulin and insulin secretion.49 In Type II diabetic patients this interaction breaks down, leading to impaired insulin secretion due to a dysfunction of the pancreatic β-cells and impaired insulin action through insulin resistance.50 The genetic influence on Type II diabetes is thought to be greater than Type I, however the specific inheritance pattern and many of the influential genes remain unknown.47 10 1.3.1 Prevalence In the United States, a total of 29.1 million people or 9.3% of the population have diabetes.2 The prevalence of diabetes is increasing annually with older individuals, Native Americans, Hispanics, and non-Hispanic blacks more commonly affected than younger individuals and nonHispanic whites.2 The incidence of diabetes is also increasing, with 1.7 million new cases reported in 20122 and 1.9 million new cases reported in 201151 compared to 1.3 million cases in 2003 and 800,000 in 1998.52 Of the close to 30 million cases in the United States, approximately 90% are Type II.2 The World Health Organization estimates 177 million Type II diabetics worldwide and predicts that number doubling by the year 2030,53 with the greatest numbers of new diabetics likely to occur in developing and emerging societies, due to the global nutrition crisis rooted dually in hunger and obesity. Most data estimate the prevalence of undiagnosed and diagnosed Type II diabetes approaches twenty percent.51 1.3.2 Risk factors for Diabetes The risk factors for Type I diabetes are much less clear than those for Type II. While genetics is known to play a larger role in Type II, the prevalence of Type I diabetes is increased in those with a parent or sibling affected by Type I diabetes. According to the American Diabetes Association,54 the odds of having Type I diabetes if your father has Type I, are 1 in 17. The odds are less if your mother is affected. If both parents have Type I diabetes, the risk ranges from 1 in 10 to 1 in 4. If either parent suffers from Type II polyglandular autoimmune syndrome, a relatively common condition among Type I diabetics, the risk for the child is 1 in 2. This inherited risk alone is not sufficient to cause disease and requires an environmental factor, such 11 as diet or infection.55 Many hypothesized environmental factors, and their relationship to genetic susceptibility, are still not well understood. Risk factors for Type II diabetes are better understood and well described in the literature. Typically grouped into modifiable and non-modifiable, the constellation of risk factors convey a clear susceptibility to Type II diabetes. Non-modifiable risk factors include age, race, gender, and family history.56 The risk of developing diabetes increases significantly with age.50 Individuals of African American, Mexican American, and Native American ethnic origin are also at a higher risk for developing diabetes. The true effect of race is likely confounded by other factors prevalent among these racial groups including obesity, smoking, and hypertension.57 However, the magnitude of the differences between ethnic groups when exposed to similar environments implies a significant genetic contribution.56 This genetic contribution is further reinforced by a higher prevalence of Type II diabetes in those who have a family history of the disease, though the genes involved in this susceptibility remain unknown.56 The most important modifiable risk factor for Type II diabetes is obesity.56 More than one-third of American adults and 17% of youth are overweight or obese.58 A longitudinal study by Chan et al.59 demonstrated obesity to be a powerful predictor of future Type II diabetes. It has also been demonstrated that interventions aimed at reducing obesity are successful in reducing the incidence of Type II diabetes.56 While obesity is a problem, data suggest60 that the distribution of fat may be more important than total fat, with visceral or abdominal fat being the best indicator for future disease. In close relation to obesity, physical inactivity is also an important and independent risk factor. Studies have shown61, 62 that for equivalent levels of obesity, higher levels of physical activity were related with a lower incidence of diabetes. As one might expect when obesity is a large risk factor, diet seems to have an influence on diabetes 12 susceptibility, though the exact role is difficult to ascertain. It has been reported63 that a high total calorie and low dietary fiber intake, high glycemic load and a low polyunsaturated to saturated fat ratio may predispose to Type II diabetes. Lastly, metabolic syndrome has been shown to increase the risk for both cardiovascular disease and Type II diabetes.64 Metabolic syndrome is a common presentation in the United States and consists of at least three of the following clinical findings: abdominal adiposity, low HDL cholesterol, high triglycerides, hypertension, and impaired fasting glucose. In a prospective cohort study with a large sample size,64 metabolic syndrome was found to be associated with approximately half of the incident cases of Type II diabetes over an eight-year period with an age-adjusted relative risk of 6.92 (95% CI 4.47-10.8). While it is clear that many of these risk factors are interdependent, each has the ability to decrease the incidence of Type II diabetes if targeted in an intervention. These types of interventions should be the focus of public health and medicine in order to decrease the prevalence of Type II diabetes. 1.3.3 Periodontal disease and diabetes The most significant early work establishing relationship between diabetes and periodontal disease examined the rates of both in a homogenous population of non-insulin dependent diabetic Native Americans (Pima Indians)65,66,67 with Löe (1993)68 definitively labelling periodontal disease as the sixth complication of diabetes. Grossi and Genco established in the mid-1990s69, 70 that treatment of periodontal disease would have a beneficial effect on the Type II diabetes condition, reducing glycated hemoglobin; longitudinal research71 around the same time showed that poor control of Type II diabetes had a positive association on the severity and extent of periodontal disease. This was further supported by Kaur5 which demonstrated that patients 13 with poorly controlled diabetes are at a greater risk for the development of periodontal diseases, as well as a more severe disease course than non-diabetics. The bidirectional nature of the relationship between the two diseases suggested by Löe was then subsequently confirmed by Taylor in 2001.4 By 2005, Genco and Grossi laid groundwork toward defining an inflammatory model linking cytokine production in periodontal disease with the metabolic dysfunction created by obesity in diabetes.72 This model was expanded upon and, more recently, three major mechanisms explaining the link were presented.3 First, diabetic patients display impaired neutrophil activity consisting of a reduced chemotactic response and decreased phagocytic activity.73,74 The importance of neutrophil function for periodontal health has been well documented and is evidenced by the severe periodontal destruction seen in those suffering from genetic conditions negatively affecting neutrophil number or function. The diabetic hyper-inflammatory state is being increasingly demonstrated in the literature. While normally pro-inflammatory cytokines, such as interleukin-1β, play a protective role, over-expression can lead to extensive tissue destruction.3 One study compared the gingival levels of IL-1β in well controlled and poorly controlled Type II diabetics; revealing significantly higher IL-1β levels in the poorly controlled group.75 Furthermore, TNF-α has been shown to be increased in obese women.76 demonstrating the ability of adipose tissue in Type II diabetics to produce another pro-inflammatory cytokine, possibly contributing to periodontal destruction. The last proposed mechanism centers on the role of advanced glycation end-products (AGE). These end products are used as an indicator of diabetic control over the long-term, but also have been shown to lead to a hyper-inflammatory state with increased secretion of IL-1, IL-6, and TNF- α.77 It has also been suggested78 that AGE correlates with an increased level of destructive reactive oxygen species in the gingiva. AGE not only 14 enhances the inflammatory response, but may also reduce bone formation, interfering with remodeling and healing once periodontal treatment is completed.3 While research continues to unveil the details of the connection between diabetes and periodontal disease, these proposed mechanisms provide a valid framework for the interaction and underscore the importance of neutrophil function, pro-inflammatory cytokines and bone metabolism. 15 2.0 METHODOLOGY This was a retrospective study analyzing periodontal exam data and diabetic health surveys collected as part of the American Diabetes Association Diabetes Expo in Pittsburgh, Pennsylvania, an annual diabetes health education and promotion event. This study was approved by the Institutional Review Board (IRB) of the University of Pittsburgh (IRB#: PRO15010133). Attendees to the Expo were given the opportunity to have a free complete periodontal examination as one of the various health screenings available and educational pamphlets about the relationship between periodontal disease and diabetes were provided to participants. Information on age, gender, education, smoking, diabetes, periodontal disease and oral health were collected and analyzed. 16 3.0 RESULTS Data were collected on 206 people; 47 respondents had periodontal disease and 147 did not have periodontal disease, periodontal disease being defined as probing depth 4mm or more. Ninetythree (93) individuals [47.9 percent] without periodontal disease had diabetes and fifty-four (54) individuals [36.3 percent] did not have diabetes [p=0.847 and not significant]. Eighty-six (86) individuals [44.3 percent] with diabetes and without periodontal disease reported good oral health, versus only fifteen (15) individuals with diabetes and periodontal disease who reported good oral health, a difference p=0.004, which was significant. Education was not significant, p=0.182. Bleeding upon probing among both diabetics and non-diabetics with periodontal disease was significant, p=0.003 (Table 1). 17 Table 1. Logistical regression test to show the association between individual covariates and the outcome of interest (GumDisease). *GumTreatment, OralHealth, and GumBleeding are statistically important for predicting the outcome variable. 18 Table 2. Multivariate logistical regression. GumDisease Odds Ratio Std. Err. z P>|z| anticenter 2.32 1.41 1.38 0.167 [0.704, 7.61] gumtcenter 22.0 12.1 5.62 0.000 [7.49, 64.6] Gender 1.02 0.454 0.04 0.969 [0.425, 2.44] Education 0.710 0.134 -1.81 0.071 [0.490, 1.03] Diabetes 1.38 0.616 0.72 0.471 [0.575, 3.31] gumbcenter 1.77 0.770 1.31 0.190 [0.754, 4.15] MouthRinses 1.30 0.255 1.34 0.180 [0.886, 1.91] OralHealth 0.512 0.151 -2.26 0.024 [0.294, 0.918] 1.03 1.17 0.03 0.977 [0.111, 9.58] _cons [95% Conf. Interval] *Controlling for GumTreatment, Antibiotic, Gender, Education, Gumbleeding, MouthRinses, and OralHealth, the odds of having GumDisease vs. not having GumDisease in patients with diabetes is 1.38. 19 4.0 DISCUSSION Various studies have shown the effect of diabetes on periodontal disease, and vice versa. One large study by periodontists and endocrinologists combined found that periodontal disease may contribute to the increased mortality rates among diabetics,79 while others80 have rationalized that advanced periodontitis is associated with higher HbA1C in both diabetic and non-diabetic individuals, with the effect being greater in patients with progressive periodontitis. Minimal evidence supports any association between periodontal disease and diabetes complications. No studies have considered the level of periodontal disease associated with a likelihood of diabetes complications. Periodontal disease can cause problems for patients with diabetes, in whom the diabetes can be more severe and progress more rapidly than in diabetics who do not have periodontal disease. Control and prevention of periodontal disease may be more important in patients with diabetes. Uncontrolled periodontal disease may affect control of diabetes, and the opposite could be true. It is established that this effect can be modified by good oral hygiene and control of any existing periodontal disease.81, 82 Results from this research show that not all individuals with diabetes have periodontal disease. In our sample of 206 individuals on whom we performed complete periodontal examinations, 29 had both periodontal disease and diabetes, while 93 individuals with diabetes did not have periodontal disease, a difference that was not statistically significant (p=0.847). 20 Table 1 shows the importance of oral health, specifically that individuals with good oral health have less chance of having diabetes. Periodontal treatment was shown to be a significant factor on the effect of diabetes (p=0.001). Multivariate logistical regression analysis (Table 2) was shown, controlling for periodontal treatment, gender, education, bleeding upon probing and oral health. The odds of having periodontal disease versus not having periodontal disease among patients with diabetes in our sample was 1.38, a difference that was not statistically significant (p=0.847). Results from our research show that in individuals with diabetes who are aware of their illness and make attempts to control their glycemic condition, the prevalence of periodontal disease was low. These results, however, reflect only cross-sectional analysis with a convenience sample and the finding requires prospective study with larger sample sizes to confirm. 21 5.0 CONCLUSION Retrospective study of periodontal disease among community-dwelling diabetics in this research revealed no significant relationship between diabetes and periodontal disease (p=0.847), though oral health was an important, significant factor (p=0.004). While the public health implications of periodontal disease are vast, it appears that quality glycemic control in the diabetic population can help to alleviate the burden. Further prospective research with a larger sample size is necessary to confirm this finding. 22 BIBLIOGRAPHY 1. Eke PI. et al. Update on Prevalence of Periodontitis in Adults in the United States: NHANES 2009-2012. Journal of Periodontology 2015 Feb.; 1-18. 2. Centers for Disease Control and Prevention. "National diabetes statistics report: estimates of diabetes and its burden in the United States, 2014." Atlanta, GA: US Department of Health and Human Services (2014). 3. Lakschevitz F. et al. Diabetes and periodontal diseases: interplay and links. Current Diabetes Reviews 2011; 7(6): 433-439. 4. Taylor GW. Bidirectional interrelationships between diabetes and periodontal diseases: an epidemiological perspective. Annals of Periodontology 2001; 6(1):99-112. 5. Kaur G. Holtfreter B. Rathmann W. et al. Association between Type I and Type II diabetes with periodontal disease and tooth loss. Journal Clinical Periodontology 2009; 36(9): 765-774. 6. Tsai C. Hayes C. Taylor GW. Glycemic control of type 2 diabetes and severe periodontal disease in the US adult population. Community Dentistry and Oral Epidemiolology 2002; 30(3):182-92. 7. Nowjack-Raymer R E. Sheiham A. Association of edentulism and diet and nutrition in US adults. Journal of Dental Research 2003; 82(2):123-126. 8. Petersen PE. The World Oral Health Report 2003. Continuous improvement of oral health in the 21st century. The approach of the WHO Global Oral Health Programme. Community Dentistry and Oral Epidemiology 2003; 31 (Suppl. 1):3-24. 9. Papapanou PN. Epidemiology of periodontal diseases: An update. Journal of the International Academy of Periodontology 1999; 1(4):110-116. 10. Loesche WJ. Clinical and microbiological aspects of chemotherapeutic agents used according to the specific plaque hypothesis. Journal of Dental Research 1979;58(12):2404-2412. 11. Page RC. Schroeder HE. Pathogenesis of inflammatory periodontal disease. A summary of current work. Laboratory Investigation 1976; 34(3):235-249. 23 12. Armitage GC. Development of a classification system for periodontal diseases and conditions. Annals of Periodontology 1999; 4(1):1-6. 13. Löe H. Natural history of periodontal disease in man. J Clinical Perio 1986;13(5):431-440. 14. Page RC. Offenbacher S. Schroeder HE. Seymour GJ. Kornman KS. Advances in the pathogenesis of periodontitis: Summary of developments, clinical implications and future directions. Perio 2000 1997; 14:216-248. 15. Baelum V. Fejerskov O. Manji F. Periodontal diseases in adult Kenyans. J Clinical Perio 1988; 15(7):445-452. 16. Baelum V. Fejerskov O. Karring T. Oral hygiene, gingivitis and periodontal breakdown in adult Tanzanians. Journal of Periodontal Research 1986; 21(3):221-232. 17. Grossi SG. et al. Assessment of risk for periodontal disease. I. Risk indicators for attachment loss. Journal of Periodontology 1994; 65(3):260-267. 18. Michalowicz BS. et al. Periodontal findings in adult twins. J Perio 1991;62(5):293-299. 19. Page RC. Offenbacher S. Schroeder HE. Seymour GJ. Kornman KS. Advances in the pathogenesis of periodontitis: Summary of developments, clinical implications and future directions. Perio 2000 1997;14:216-248. 20. Kornman KS. et al. The interleukin‐1 genotype as a severity factor in adult periodontal disease. Journal of Clinical Periodontology 1997; 24(1):72-77. 21. Papapanou PN. Periodontal diseases: epidemiology. Annals Periodontology 1996;1(1):1-36. 22. Barbour SE. et al. Tobacco and smoking: environmental factors that modify the host response (immune system) and have an impact on periodontal health. Critical Reviews in Oral Biology and Medicine 1997; 8(4):437-460. 23. Bergström J. Preber H. Tobacco Use as a Risk Factor. Journal Perio 1994; 65(5):545-550. 24. Ah B. et al. The effect of smoking on the response to periodontal therapy. J Clinical Perio 1994; 21(2):91-97. 25. Haber J. Smoking is a major risk factor for periodontitis. Current Opinion Perio 1993; 12-18. 26. Bergström J. Blomlöf L. Tobacco smoking major risk factor associated with refractory periodontal disease. JDR 1992; 71(special issue) 297 #1530 IADR abstract. 27. Albandar JM. Brunelle JA. Kingman A. Destructive periodontal disease in adults 30 years of age and older in the United States, 1988-1994. Journal of Periodontology 1999; 70(1):13-29. 24 28. Hyman JJ. Reid BC. Epidemiologic risk factors for periodontal attachment loss among adults in the United States. J Clinical Periodontology 2003; 30(3):230-237. 29. National Center for Health Statistics (US). Oral Hygiene in Adults United States 1960-1962. 30. Oral Health of United States Adults: The National Survey of Oral Health in US Employed Adults and Seniors, 1985-1986: National Findings. National Institutes of Health 1987. 31. Kelly JE. Van Kirk LE. Periodontal disease in adults United States 1960-1962. US Department of Health Education and Welfare, Public Health Service. National Center for Health Statistics 1965. 32. Kelly JE. Harvey CE. Basic data on dental examination findings of persons 1-74 years. United States, 1971-1974. Vital and health statistics. Series 11, Data from the national health survey 214 (1979): 1-33. 33. Eke PI. et al. Prevalence of periodontitis in adults in the United States: 2009 and 2010. Journal of Dental Research 2012; 91(10):914-920. 34. Brown L. Jackson R. Oliver C. Loe H. Evaluating periodontal status of US employed adults. Journal of the American Dental Association 1990; 121(2):226-232. 35. Velden U. Effect of age on the periodontium. Journal Clinical Perio 1984; 11(5):281-294. 36. Johnson BD. et al. Aging or Disease? Periodontal changes and treatment considerations in the older dental patient 1. Gerodontology 1989; 8(4): 109-118. 37. AAP Position Paper 2005. Epidemiology of periodontal disease. 38. Hart TC. Shapira L. Van Dyke TE. Neutrophil defects as risk factors for periodontal diseases. J Perio 1994; 65(5 Suppl.):521-529. 39. Deas DE. Mackey SA. McDonnell HT. Systemic disease and periodontitis: manifestations of neutrophil dysfunction. Perio 2000 2003; 32(1):82-104. 40. Löe H. Periodontal disease: the sixth complication of diabetes mellitus. Diabetes Care 1993; 16(1):329-334. 41. Saito T. Shimazaki Y. Sakamoto M. Obesity and periodontitis. NEJM 1998; 339(7):482-483. 42. Ritchie CS. Obesity and periodontal disease. Perio 2000 2007; 44(1): 154-163. 43. von Wowern N. Klausen B. Kollerup G. Osteoporosis: a risk factor in periodontal disease." J Perio 1994; 65(12):1134-1138. 25 44. Famili P. et al. Longitudinal study of periodontal disease and edentulism with rates of bone loss in older women. J Perio 2005; 76(1):11-15. 45. Centers for Disease Control and Prevention. Complications due to diabetes. www.cdc.gov/diabetes/living/problems.html. Accessed 12-19-2014. 46. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2010; 33(Supplement 1):S62-S69. 47. Ozougwu JC. et al. The pathogenesis and pathophysiology of Type 1 and Type 2 diabetes mellitus. J Physiol Pathophysiol 2013; 4: 40-57. 48. Kohei KAKU. Pathophysiology of Type 2 diabetes and its treatment policy. Journal of the Japan Medical Association 2010; 53(1):41-46. 49. DeFronzo RA. The triumvirate: β-cell, muscle, liver. A collusion responsable for NIDDM. Diabetes 1988; 37(6):667-687. 50. Holt RIG. Diagnosis, epidemiology and pathogenesis of diabetes mellitus: an update for psychiatrists. The British Journal of Psychiatry 2004; 184(47): s55-s63. 51. Centers for Disease Control and Prevention (CDC). National diabetes fact sheet: national estimates and general information on diabetes and pre-diabetes in the United States 2011. US Department of Health and Human Services, Centers for Disease Control and Prevention 2011. 52. Centers for Disease Control and Prevention. National diabetes fact sheet 2005. Accessed 15 February 2015. 53. World Health Organization. The World Health Report 2002. Reducing risks, promoting healthy life. Geneva: World Health Organization 2002. 54. American Diabetes Association. Genetics of Diabetes. www.diabetes.org/diabetesbasics/genetics-of-diabetes.html. Accessed 15 February 2015. 55. Dean L. McEntyre J. The genetic landscape of diabetes. Bethesda (MD): National Center for Biotechnology Information (US) 2004. 56. Alberti K. George MM. Zimmet P. Shaw J. International Diabetes Federation: a consensus on Type 2 diabetes prevention. Diabetic Medicine 2007; 24(5):451-463. 57. American Diabetes Association. Non-Modifiable Risk Factors. www.professional.diabetes.org/resourcesforprofessionals. Accessed 15 February 2015. 58. Ogden CL. et al. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA 2014; 311(8):806-814. 26 59. Chan JM. et al. Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diabetes Care 1994; 17(9): 961-969. 60. Ohlson LO. et al. The influence of body fat distribution on the incidence of diabetes mellitus: 13.5 years of follow-up of the participants in the study of men born in 1913. Diabetes 1985; 34(10):1055-1058. 61. Hu FB. et al. Television watching and other sedentary behaviors in relation to risk of obesity and Type 2 diabetes mellitus in women. JAMA 2003; 289(14):1785-1791. 62. Hu FB. et al. Physical activity and television watching in relation to risk for Type 2 diabetes mellitus in men. Archives of Internal Medicine 2001; 161(12):1542-1548. 63. Hu FB. et al. Diet, lifestyle, and the risk of Type 2 diabetes mellitus in women. NEJM 2001; 345(11):790-797. 64. Wilson PWF. et al. Metabolic syndrome as a precursor of cardiovascular disease and Type 2 diabetes mellitus. Circulation 2005; 112(20): 3066-3072. 65. Shlossman M. et al. Type 2 diabetes mellitus and periodontal disease. JADA 1990; 121(4):532-536 66. Nelson RG. et al. Periodontal disease and NIDDM in Pima Indians. Diabetes Care 1990; 13(.8):836-840. 67. Emrich LJ. Shlossman M. Genco RJ. Periodontal disease in non-insulin-dependent diabetes mellitus. J Perio 1991; 62(2): 123-131. 68. Löe H. Periodontal disease: the sixth complication of diabetes mellitus. Diabetes Care 1993; 16(1): 329-334. 69. Grossi SG.et al. Response to periodontal therapy in diabetics and smokers. J Perio 1996; 67(10 Suppl.): 094-1102. 70. Grossi SG. et al. Treatment of periodontal disease in diabetics reduces glycated hemoglobin. J Perio 1997; 68(8):713-719. 71. Taylor GW. et al. Glycemic control and alveolar bone loss progression in Type 2 diabetes. Annals of Periodontology 1998; 3(1):30-39. 72. Genco RJ. et al. A proposed model linking inflammation to obesity, diabetes, and periodontal infections. J Periodontology 2005; 76(11-Suppl.): 2075-2084. 73. Gursoy UK. Marakoglu I. Ostop AY. Relationship between neutrophil functions and severity of periodontitis in obese and/or Type 2 diabetic chronic periodontitis patients. Quintessence International 2008; 39(6): 485-489. 27 74. Chanchamroen S. Kewcharoenwong C. Susaengrat W. Ato M. Lertmemongkolchai G. Human polymorphonuclear neutrophil responses to Burkoholderia pseudomallei in healthy and diabetic subjects. Infection and Immunity 2009; 77(1): 456-463. 75. Cutler CW. Machen RL. Jotwani R. Iacopino AM. Heightened gingival inflammation and attachment loss in Type II diabetes with hyperlipidemia. J Perio 1999; 70(11):1313-1321. 76. Bullo M. Garcia-Lorda P. Megias I. Salas-Salvado J. Systemic inflammation, adipose tissue tumor necrosis factor and leptin expression. Obesity Research 2003; 11(4): 525-531. 77. Goldin A. Beckman JA. Schmidt AM. Creager MA. Advanced glycation end products: sparking the development of diabetic vascular injury. Circulation 2006; 114(6):597-605. 78. Schmidt AM. Weidman E. Lalla E. et al. Advanced glycation end-products (AGEs) induce oxidant stress in the gingiva: a potential mechanism underlying accelerated periodontal disease associated with diabetes. Journal of Periodontal Research 1996; 31(7): 508-515. 79. Saremi A. et al. Periodontal disease and mortality in Type 2 diabetes. Diabetes Care 2005; 28(1):27-32. 80. Bascones-Martínez A. González-Febles J. Sanz-Esporrin J. Diabetes and periodontal disease. Review of the literature. American Journal of Dentistry 2014; 27(2): 63-67. 81. Katz P. et al. Epidemiology and prevention of periodontal disease in individuals with diabetes. Diabetes Care 1991; 14(5): 375-385. 82. Taylor GW. Borgnakke WS. Periodontal disease: associations with diabetes, glycemic control and complications. Oral Diseases 2008; 14(3):191-203. 28